Reducing the risk of post-endoscopic retrograde cholangiopancreatography pancreatitis using 4-Fr pancreatic plastic stents placed with common-type guidewires: Results from a prospective multinational registry
Abstract
Background and Aim
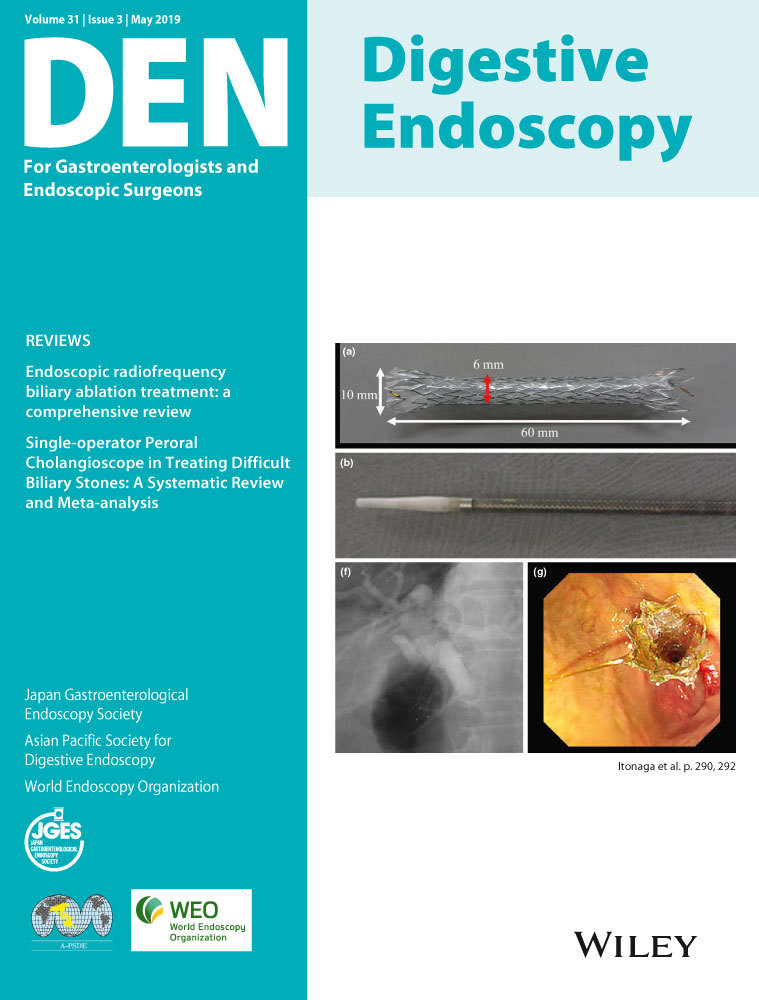
Pancreatic plastic stents (PPS) can reduce the risk of post-endoscopic retrograde cholangiopancreatography pancreatitis (PEP). Prospective multicenter documentation of PEP rate after PPS placement is scarce. A new 4-Fr stent designed to be deployed over a 0.035-inch guidewire was used to assess the effectiveness of PEP prophylaxis.
Methods
High-PEP-risk patients received a 4-Fr PPS for primary or secondary prophylaxis at seven centers in four countries. Patients were followed until spontaneous PPS migration, endoscopic stent removal, or for 4 months, whichever came first. Main outcome was PEP rate.
Results
One hundred six (106) patients received PPS for PEP prophylaxis [61 (58%) primary, 45 (42%) secondary prophylaxis]. Median age was 54 years. Eighty-one (76%) PPS were placed using a 0.035-inch guidewire. By investigator choice 99 (93%) stents were single pigtail. Median stent length was 8 cm (range 3–12 cm). Technical success achieved in 100% of cases. Two patients in the primary prophylaxis group (3%, 95% CI 0.4–11%) experienced mild/moderate PEP. Seventy-eight PPS available for analysis underwent spontaneous migration after a median of 29 days. There were no reports of stent-induced ductal trauma. Post-hoc analysis of migration rate by PPS length showed no statistically significant trend.
Conclusions
Among high-risk patients in the primary prophylaxis group, observed rates of PEP are low (3%, 95% CI 0.4–11%) with the use of prophylactic 4-Fr pancreatic duct stents compatible with a 0.035-inch guidewire. This low rate is not unequivocally due to the prophylactic stent.
Conflicts of Interest
A.R. is a consultant for Boston Scientific. G.A.C. is a consultant for Boston Scientific and Olympus Corporation. H.N. receives research support from Boston Scientific, Cook Medical, ERBE, and CDx Diagnostics, and he is a consultant for Boston Scientific, Cook Medical, ERBE, and Olympus. H.N. also receives speaker's fees from Boston Scientific, Cook Medical, ERBE, Olympus, the Falk Foundation, Fujifilm, and Medtronic. M.J.B. is a consultant for and receives research grants from Boston Scientific, Cook Medical, 3M, and Pentax Medical. R.K. receives research support from Boston Scientific and book royalties from Wiley-Blackwell, Springer, and Elsevier. T.B. is a consultant for Boston Scientific. J.W.P. is a consultant for Boston Scientific, Cook Endoscopy, and Pentax Medical. M.F. is a consultant for Boston Scientific and receives speaker's fees from Cook Endoscopy. P.K. is a consultant for Boston Scientific. P.T. is a consultant for Boston Scientific. All other authors declare no conflicts of interest with respect to this work. This registry was sponsored by Boston Scientific Corporation and registered under number NCT02262845 in the USA and CTRI/2015/09/006194 in India.