An update on congenital melanocytic nevus syndrome: A case report and literature review
Corresponding Author
Lilaf Abdulmajid
Faculty of Medicine and Health Sciences, University Antwerp, Wilrijk, Belgium
Correspondence
Lilaf Abdulmajid, Antwerp University, Campus Drie Eiken, Universiteitsplein 1, 2610 Wilrijk, Belgium.
Email: [email protected]
Search for more papers by this authorFrancesca Maria Bosisio
Department of Pathology, University Hospitals Leuven, KU Leuven, Leuven, Belgium
Search for more papers by this authorHilde Brems
Department of Human Genetics, University Hospitals Leuven, UZ/KU Leuven, Leuven, Belgium
Search for more papers by this authorGreet De Vlieger
Clinical Division and Laboratory of Intensive Care Medicine, Department of Cellular and Molecular Medicine, KU Leuven, Leuven, Belgium
Search for more papers by this authorMarjan Garmyn
Department of Dermatology, University Hospitals Leuven, KU Leuven, Leuven, Belgium
Search for more papers by this authorHeidi Segers
Department of Pediatric Hemato-Oncology, University Hospitals Leuven, KU Leuven, Leuven, Belgium
Search for more papers by this authorPhilippe Demaerel
Department of Radiology, University Hospitals Leuven, KU Leuven, Leuven, Belgium
Search for more papers by this authorKatarina Segers
Department of Plastic and Reconstructive surgery, University Hospitals Leuven, KU Leuven, Leuven, Belgium
Search for more papers by this authorKatrien Jansen
Department of Development and Regeneration, University Hospitals Leuven, KU Leuven, Leuven, Belgium
Search for more papers by this authorLieven Lagae
Department of Development and Regeneration, Section Pediatric Neurology, University Hospitals Leuven, KU Leuven, Leuven, Belgium
Search for more papers by this authorMagali Verheecke
Department of Obstetrics and Gynecology, AZ Turnhout, Turnhout, Belgium
Search for more papers by this authorCorresponding Author
Lilaf Abdulmajid
Faculty of Medicine and Health Sciences, University Antwerp, Wilrijk, Belgium
Correspondence
Lilaf Abdulmajid, Antwerp University, Campus Drie Eiken, Universiteitsplein 1, 2610 Wilrijk, Belgium.
Email: [email protected]
Search for more papers by this authorFrancesca Maria Bosisio
Department of Pathology, University Hospitals Leuven, KU Leuven, Leuven, Belgium
Search for more papers by this authorHilde Brems
Department of Human Genetics, University Hospitals Leuven, UZ/KU Leuven, Leuven, Belgium
Search for more papers by this authorGreet De Vlieger
Clinical Division and Laboratory of Intensive Care Medicine, Department of Cellular and Molecular Medicine, KU Leuven, Leuven, Belgium
Search for more papers by this authorMarjan Garmyn
Department of Dermatology, University Hospitals Leuven, KU Leuven, Leuven, Belgium
Search for more papers by this authorHeidi Segers
Department of Pediatric Hemato-Oncology, University Hospitals Leuven, KU Leuven, Leuven, Belgium
Search for more papers by this authorPhilippe Demaerel
Department of Radiology, University Hospitals Leuven, KU Leuven, Leuven, Belgium
Search for more papers by this authorKatarina Segers
Department of Plastic and Reconstructive surgery, University Hospitals Leuven, KU Leuven, Leuven, Belgium
Search for more papers by this authorKatrien Jansen
Department of Development and Regeneration, University Hospitals Leuven, KU Leuven, Leuven, Belgium
Search for more papers by this authorLieven Lagae
Department of Development and Regeneration, Section Pediatric Neurology, University Hospitals Leuven, KU Leuven, Leuven, Belgium
Search for more papers by this authorMagali Verheecke
Department of Obstetrics and Gynecology, AZ Turnhout, Turnhout, Belgium
Search for more papers by this authorAbstract
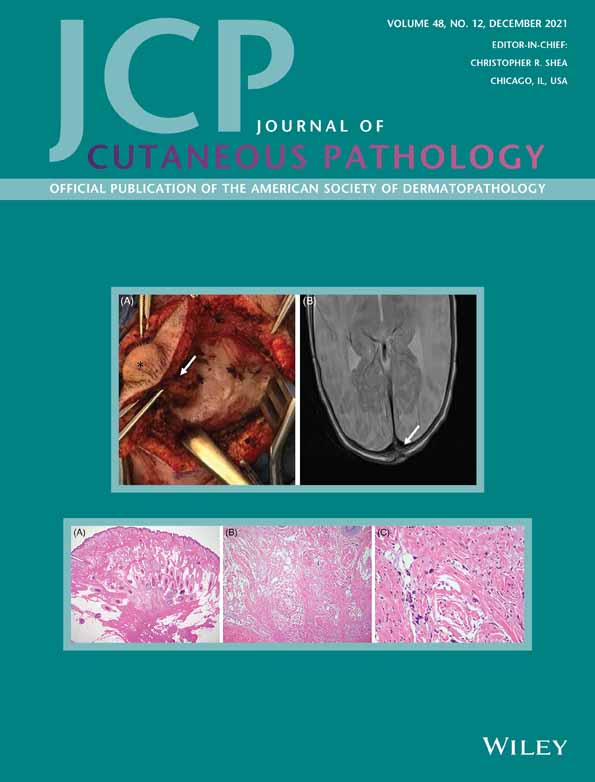
Congenital melanocytic nevus syndrome (CMNS) is a rare condition characterized by pigmented skin lesions that are usually present at birth and are associated with an increased risk of neurological abnormalities and malignant melanoma. It mostly results from a post-zygotic NRAS mutation of neural-derived crest cells, leading to uncontrolled cell growth. Because of the increased knowledge of the genetics underlying CMNS, targeted therapy becomes a promising treatment option. We present a case of CMNS in a newborn. Physical examination at birth showed a giant congenital melanocytic nevus, extending from the occipital to the lower lumbar region. A magnetic resonance imaging scan revealed multiple cerebral and cerebellar parenchymal lesions. Genetic analysis of the cutaneous lesions showed the presence of an NRAS Q61R mutation. The patient was treated with dermabrasion to reduce the color intensity of the nevus. However, this was complicated by recurrent wound infections and laborious wound healing. At the age of 1 year, the patient had an age-appropriate psychomotor development, without neurological deficits.
Open Research
DATA AVAILABILITY STATEMENT
Author elects to not share data
REFERENCES
- 1Ma T, Fan K, Li L, et al. Tissue expansion in the treatment of giant congenital melanocytic nevi of the upper extremity. Medicine (Baltimore). 2017; 96(13):e6358.
- 2Castilla EE, da Graça DM, Orioli-Parreiras IM. Epidemiology of congenital pigmented naevi: I. Incidence rates and relative frequencies. Br J Dermatol. 1981; 104(3): 307-315.
- 3Kadonaga JN, Frieden IJ. Neurocutaneous melanosis: definition and review of the literature. J Am Acad Dermatol. 1991; 24(5 Pt 1): 747-755.
- 4Kinsler V, Shaw AC, Merks JH, Hennekam RC. The face in congenital melanocytic nevus syndrome. Am J Med Genet A. 2012; 158A(5): 1014-1019.
- 5Ramaswamy V, Delaney H, Haque S, Marghoob A, Khakoo Y. Spectrum of central nervous system abnormalities in neurocutaneous melanocytosis. Dev Med Child Neurol. 2012; 54(6): 563-568.
- 6Islam MP. Neurocutaneous melanosis. Handb Clin Neurol. 2015; 132: 111-117.
- 7Kinsler VA, Thomas AC, Ishida M, et al. Multiple congenital melanocytic nevi and neurocutaneous melanosis are caused by postzygotic mutations in codon 61 of NRAS. J Invest Dermatol. 2013; 133(9): 2229-2236.
- 8Salgado CM, Basu D, Nikiforova M, et al. Amplification of mutated NRAS leading to congenital melanoma in neurocutaneous melanocytosis. Melanoma Res. 2015; 25(5): 453-460.
- 9Belysheva TS, Vishnevskaya YV, Nasedkina TV, et al. Melanoma arising in a giant congenital melanocytic nevus: two case reports. Diagn Pathol. 2019; 14(1): 21.
- 10Salgado CM, Basu D, Nikiorova M, et al. BRAF mutations are also associated with neurocutaneous melanocytosis and large/giant congenital melanocytic nevi. Pediatr Dev Pathol. 2015; 18(1): 1-9.
- 11Welfringer-Morin A, Pinto G, Baujat G, et al. Hypophosphatemic rickets: a rare complication of congenital melanocytic nevus syndrome. Pediatr Dermatol. 2020; 37(3): 541-544.
- 12Sakaguchi Y, Uehara T, Sasaki M, et al. Hereditary spastic paraplegia masqueraded by congenital melanocytic nevus syndrome: dual pathogenesis of germline non-mosaicism and somatic mosaicism. Eur J Med Genet. 2020; 63(4): 103803.
- 13Chen L, Zhai L, Al-Kzayer LFY, et al. Neurocutaneous melanosis in association with large congenital melanocytic nevi in children: a report of 2 cases with clinical, radiological, and pathogenetic evaluation. Front Neurol. 2019; 10: 79.
- 14Ulrich M, Tinschert S, Siebert E, et al. Detection of a multilineage mosaic NRAS mutation c.181C>A (p>Gln61Lys) in an individual with a complex nevus syndrome. Pigment Cell Melanoma Res. 2019; 32(3): 470-473.
- 15Maridet C, Morice-Picard F, Gros A, et al. Mosaic NRASopathy in a child with giant melanocytic congenital nevus, epidermal hamartoma and bilateral nephroblastomatosis: clinical implication for follow-up. J Eur Acad Dermatol Venereol. 2018; 32(7): e258-e260.
- 16De la Rosa CD, Vindenes H, Kinsler V, et al. Aggressive melanoma in an infant with congenital melanocytic nevus syndrome and multiple, NRAS and BRAF mutation-negative nodules. Pediatr Dermatol. 2018; 35(5): e281-e285.
- 17Habougit C, Forest F, Boutet C, et al. An 11-year-old boy with a leptomeningeal tumor. Brain Pathol. 2017; 27(4): 553-554.
- 18Recio A, Sánchez-Moya AI, Félix V, Campos Y. Congenital melanocytic nevus syndrome: a case series. Actas Dermosifiliogr. 2017; 108(9): e57-e62.
- 19Ramesh R, Shaw N, Miles EK, Richard B, Colmenero I, Moss C. Mosaic NRAS Q61R mutation in a child with giant congenital melanocytic naevus, epidermal naevus syndrome and hypophosphataemic rickets. Clin Exp Dermatol. 2017; 42(1): 75-79.
- 20Kolin DL, Geddie WR, Ko HM. CSF cytology diagnosis of NRAS-mutated primary leptomeningeal melanomatosis with neurocutaneous melanosis. Cytopathology. 2017; 28(3): 235-238.
- 21Uguen A, Laurent C, Samaison L, et al. Severe hydrocephalus caused by diffuse leptomeningeal and neurocutaneous melanocytosis of antenatal onset: a clinical, pathologic, and molecular study of 2 cases. Hum Pathol. 2015; 46(8): 1189-1196.
- 22Küsters-Vandevelde HV, Willemsen AE, Groenen PJ, et al. Experimental treatment of NRAS-mutated neurocutaneous melanocytosis with MEK162, a MEK-inhibitor. Acta Neuropathol Commun. 2014; 2: 41.
- 23Shih F, Yip S, McDonald PJ, Chudley AE, Del Bigio MR. Oncogenic codon 13 NRAS mutation in a primary mesenchymal brain neoplasm and nevus of a child with neurocutaneous melanosis. Acta Neuropathol Commun. 2014; 2: 140.
- 24Basu D, Salgado CM, Bauer BS, et al. Nevospheres from neurocutaneous melanocytosis cells show reduced viability when treated with specific inhibitors of NRAS signaling pathway. Neuro Oncol. 2016; 18(4): 528-537.
- 25Yu Q, Wu M, Sheng L, Li Q, Xie F. Therapeutic effects of targeting RAS-ERK signaling in giant congenital melanocytic nevi. Am J Transl Res. 2018; 10(4): 1184-1194.
- 26Basu D, Salgado CM, Bauer B, et al. The dual PI3K/mToR inhibitor omipalisib/GSK21264458 inhibits clonogenic growth in oncogenically-transformed cells from neurocutaneous melanocytosis. Cancer Genomics Proteomics. 2018; 15(4): 239-248.
- 27Kinsler VA, O'Hare P, Jacques T, Hargrave D, Slater O. MEK inhibition appears to improve symptom control in primary NRAS-driven CNS melanoma in children. Br J Cancer. 2017; 116(8): 990-993.
- 28Patterson J, Hosler G, Prenshaw K. Weedon's Skin Pathology. 5th ed. Charlottesville, VA: Elsevier; 2020.
- 29Calonje EJ, Brenn T, Lazar A, Billings S. McKee's Pathology of the Skin. 5th ed. Cleveland, OH: Elsevier; 2019.
- 30Perry A, Daniel JB. Practical Surgical Neuropathology. Philadelphia, PA: Elsevier; 2010.
- 31Dhillon AS, Hagan S, Rath O, Kolch W. MAP kinase signaling pathways in cancer. Oncogene. 2007; 26(22): 3279-3290.
- 32Küsters-Vandevelde HV, Küsters B, van Engen-van Grunsven AC, Groenen PJ, Wesseling P, Blokx WA. Primary melanocytic tumors of the central nervous system: a review with focus on molecular aspects. Brain Pathol. 2015; 25(2): 209-226.
- 33Ichii-Nakato N, Takata M, Takayanagi S, et al. High frequency of BRAFV600E mutation in acquired nevi and small congenital nevi, but low frequency of mutation in medium-sized congenital nevi. J Invest Dermatol. 2006; 126(9): 2111-2118.
- 34Poynter JN, Elder JT, Fullen DR, et al. BRAF and NRAS mutations in melanoma and melanocytic nevi. Melanoma Res. 2006; 16(4): 267-273.
- 35Bauer J, Curtin JA, Pinkel D, Bastian BC. Congenital melanocytic nevi frequently harbor NRAS mutations but no BRAF mutations. J Invest Dermatol. 2007; 127(1): 179-182.
- 36Cohen AS, Wilson SL, Trinh J, Ye XC. Detecting somatic mosaicism: considerations and clinical implications. Clin Genet. 2015; 87(6): 554-562.
- 37Polubothu S, McGuire N, Al-Olabi L, et al. Does the gene matter? Genotype-phenotype and genotype-outcome associations in congenital melanocytic naevi. Br J Dermatol. 2020; 182(2): 434-443.
- 38Pawlikowski JS, Brock C, Chen SC, et al. Acute inhibition of MEK suppresses congenital melanocytic nevus syndrome in a murine model driven by activated NRAS and Wnt signaling. J Investig Dermatol. 2015; 135(8): 2093-2101.
- 39Sakamoto M, Morimoto N, Jinno C, et al. Melanin pigments in the melanocytic nevus regress spontaneously after inactivation by high hydrostatic pressure. PloS One. 2017; 12(11):e0186958.
- 40Marghoob AA, Borrego JP, Halpern AC. Congenital melanocytic nevi: treatment modalities and management options. Semin Cutan Med Surg. 2007; 26(4): 231-240.
- 41Dragieva G, Hafner J, Künzi W, et al. Malignant melanoma in a large congenital melanocytic nevus 9 years after dermabrasion in childhood. Dermatology. 2006; 212(2): 208-209.