Facial follicular cysts: a case of lichen planus follicularis tumidus?
Abstract
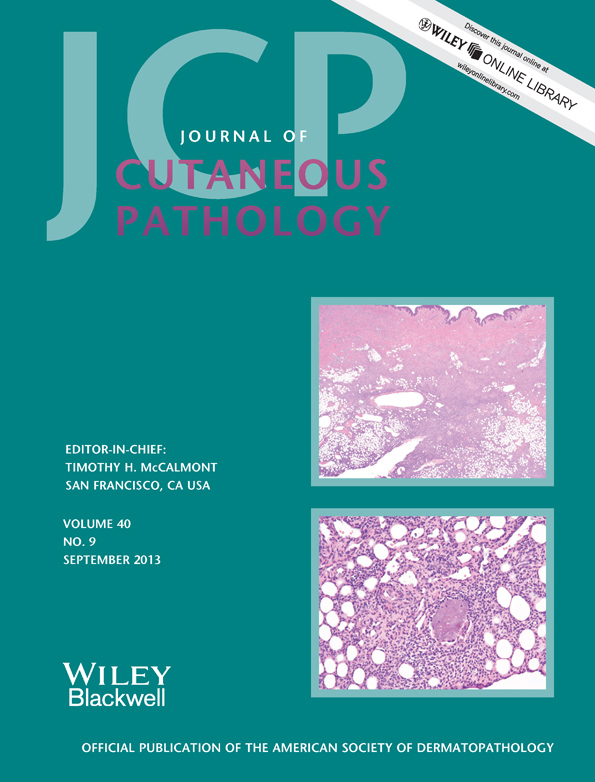
Lichen planus follicularis tumidus (LPFT) represents an uncommon variety of lichen planus (LP). Clinically, it presents with prominent purplish lesions or white-pigmented yellowish cysts and comedones. Histopathologically, it is similar to lichen planopilaris, and it is additionally characterized by follicles and cysts surrounded by a lichenoid lymphocytic infiltrate. The most common location is the retroauricular region, and it may be associated with other variants of LP. Herein, we describe the case of a 50-year-old woman with a history of lower limb hypertrophic LP who subsequently presented with multiple pink, tumid, pruritic plaques with white-yellow cysts and comedones extensively affecting the bilateral face. Histopathologic examination revealed a lichenoid infiltrate surrounding the follicles and cysts. We diagnosed LPFT and began treatment with topical corticosteroids, antihistamines, systemic corticosteroids and oral acitretin without improvement. Subsequently, the patient had an acceptable response to cyclosporine at doses of 5 mg/kg/day with remission of itching and tumidity but with residual cysts and comedones remaining. To date, the literature contains only 16 cases of LPFT. To our knowledge, this is the most severe case and is the only one with cessation of disease activity in response to cyclosporine.