Material and abutment selection for CAD/CAM implant-supported fixed dental prostheses in partially edentulous patients – A narrative review
Abstract
Restorative material selection has become increasingly challenging due to the speed of new developments in the field of dental material science. The present narrative review gives an overview of the current indications for implant abutments and restoration materials for provisional and definitive implant-supported fixed dental prostheses in partially edentulous patients. For single implant restorations, titanium base abutments for crowns are suggested as an alternative to the conventional stock- and customized abutments made out of metal or zirconia. They combine the mechanical stability of a metallic connection with the esthetic potential of ceramics. For multiple-unit restorations, conical titanium bases especially designed for bridges are recommended, to compensate for deviating implant insertion axes and angulations. Even though titanium base abutments with different geometries and heights are available, certain clinical scenarios still benefit from customized titanium abutments. Indications for the definitive material in fixed implant restorations depend on the region of tooth replacement. In the posterior (not esthetically critical) zone, ceramics such as zirconia (3–5-Ymol%) and lithium-disilicate are recommended to be used in a monolithic fashion. In the anterior sector, ceramic restorations may be buccally micro-veneered for an optimal esthetic appearance. Lithium-disilicate is only recommended for single-crowns, while zirconia (3–5-Ymol%) is also recommended for multiple-unit and cantilever restorations. Attention must be given to the specific mechanical properties of different types of zirconia, as some feature reduced mechanical strengths and are therefore not indicated for all regions and restoration span lengths. Metal-ceramics remain an option, especially for cantilever restorations.
1 INTRODUCTION
In the past, dentistry relied on the manual fabrication of frameworks and restorations, often requiring a multitude of analog clinical and laboratory steps (Mangano et al., 2017). With the rise of computer technology, newer fabrication methods, and materials have become available (Çakmak et al., 2021; Mizumoto & Yilmaz, 2018). Digital planning, commonly referred to as computer-aided design (CAD), and industrial manufacturing, known as computer-aided manufacturing (CAM), have revolutionized the selection of treatment modalities available to dentists today (Alexakou et al., 2019; Legaz et al., 2020). As a consequence of this shift to a digitalized workflow, there have been major material developments on implant abutment level (Cevik et al., 2022; Südbeck et al., 2022) as well as provisional- (Suphangul et al., 2022) and definitive (AlTarawneh et al., 2021; Pjetursson et al., 2021) restoration level. A broad variety of materials are available for implant-supported single-crowns (SC) (Agustin-Panadero et al., 2020) and multiple-unit fixed dental prostheses (FDPs) (Pjetursson et al., 2015) as provisional—as well as definitive restorative materials.
Provisional implant restorations, also known as temporary restorations or interim restorations, play a crucial role during implant treatment (Santosa, 2007). They may serve as diagnostic aids, surgical guides, and functional and esthetic evaluators (Ionescu et al., 2022; Lewis & Klineberg, 2011; Moscovitch & Saba, 1996; Siadat et al., 2017). They can also be used to shape and support the peri-implant mucosa, and to maintain interproximal and occlusal contact points until the fabrication of the definitive restoration (Buser et al., 2004). Furthermore, an interim restoration may also be used as a prototype: a first or preliminary version of an object from which other forms are developed. The data gathered from evaluating such a prototype may help guide the fabrication of the definitive restoration with the goal to optimize function, esthetic appearance, and patient satisfaction (Legaz et al., 2020; Santosa, 2007; Siadat et al., 2017). Additionally, both interim restorations and prototypes may help the patient to visualize a possible final outcome and therefore present a useful communication tool for the restorative treatment team (Conejo et al., 2021; Santosa, 2007; Siadat et al., 2017; Touati et al., 2022).
The selection of a restorative material for provisional implant restorations requires a careful consideration of factors like mechanical strength, indication spectrum, biocompatibility, and esthetic appearance. Due to those restorations being temporary, additional secondary factors such as time- and cost-efficiency should also be considered (Südbeck et al., 2022). The advancement of CAD/CAM technology has enabled implant-supported provisional restorations to be fabricated via a direct chairside workflow or an indirect laboratory approach (Tsujimoto et al., 2019).
Definitive restorative materials generally offer different advantages and disadvantages, and thus biological, mechanical, and esthetic aspects have to be carefully considered during the decision-making process (Sailer et al., 2022). Ceramic materials are often preferred by patients due to their tooth-like color and therefore highly esthetic appearance (Li et al., 2014). Furthermore, dental ceramics exhibit high biocompatibility, which seems to be of importance for ensuring healthy peri-implant tissues (Mallineni et al., 2013). Nevertheless, mechanical properties such as limited flexural strengths limit the range of indications for all-ceramic materials. In contrast, metal-ceramic restorations are well documented over the last decades and present excellent mechanical characteristics while exhibiting limitations such as esthetic appearance and fabrication complexity. In both metal-ceramic and veneered all-ceramic materials, technical complications such as fractures of the veneering ceramic, occur commonly (Sailer et al., 2022). Other known technical complications to be considered when selecting abutment and restoration materials are framework fractures, screw-loosening, screw fractures, and loss of retention of the crown (Sailer et al., 2022).
In addition to the material characteristics, patient- and site-specific factors have to be taken into consideration when choosing the adequate material for each clinical situation. The implant location (esthetic/non-esthetic area) and individual patient conditions such as the height of the smile line, tooth/soft tissue exposure, and the patient's esthetic demands will determine specific esthetic requirements (Buser et al., 2004). Another important aspect is the mechanical stress to which the restoration will be subjected. The restoration material will be exposed to different forces, depending on implant position (anterior/posterior), and the restoration size (single-/multiple-units) (Li et al., 2014). Thus, these aspects also play a major role in the material choice and site-specific mechanical requirements will need to be considered. These factors are of particular importance, when working under specific functional and parafunctional demands for example, in patients with bruxism, reduced prosthetic space, or the use of cantilevers.
In the present narrative review, an overview of the current state-of-the-art with regards to abutment and restoration materials for provisional and definitive implant-supported restorations is presented. It serves as guide to clinicians for the adequate material selection and flow charts are provided for clinical decision making on abutment-, provisional-, and definitive restoration material choice.
2 ABUTMENT SELECTION
The selection of an appropriate implant abutment plays an important role in achieving optimal function, esthetics, and long-term success of dental implants (Mattheos et al., 2021; Pjetursson et al., 2018). The abutment serves as a connecting element between the dental implant and the prosthetic restoration.
Conventional standard or stock abutments offer a more cost-efficient option compared to cast abutments, as they are readily available and can be selected based on the clinical situation (Muhlemann et al., 2018). In contrast, they do not always provide the ideal emergence profile, which may bring some challenges when it comes to cement excess removal (Linkevicius et al., 2013). Biological problems caused by remnants of cement excess, along with the lack of retrievability of cement-retained restorations, have led to screw-retention becoming more preferable in the majority of cases (Sailer et al., 2012; Wittneben et al., 2014).
Screw-retention in restorations can be mainly performed in two manners, either directly to the implant (implant level) or using an intermediate abutment firstly connected to the implant with the restoration being secured on this abutment via another smaller screw (abutment level).
With regards to the abutment material, both metal-ceramic (titanium, gold-alloys) and all-ceramic (zirconia) have been used with acceptable clinical outcomes (Ferrantino et al., 2023; Humm et al., 2023; Pjetursson et al., 2018). Although zirconia may appear esthetically superior (Bittencourt et al., 2023; Ferrantino et al., 2023), some mechanical concerns are raised due to the intrinsic brittleness of ceramics (Gehrke et al., 2016; Sailer et al., 2009). Over recent years, the options for implant abutments have evolved significantly, with new prosthetic solutions facilitated by computer-aided design and computer-aided manufacturing (CAD-CAM) developments. Customized CAD-CAM abutments and titanium base abutments have become very popular due to their integration into digital workflows and consequently increased cost-efficiency (Muhlemann et al., 2018).
2.1 Abutments for implant-supported single crowns (SCs)
2.1.1 Titanium base abutments
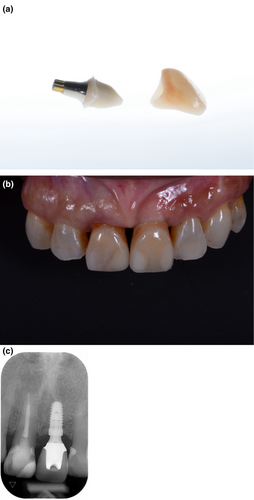
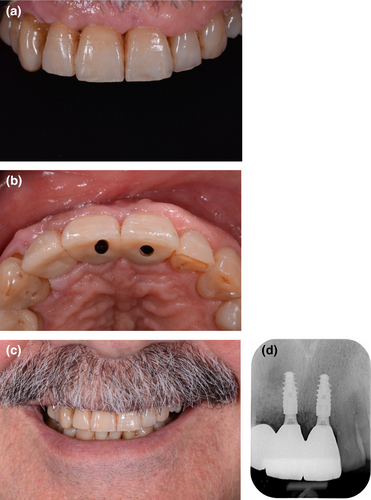
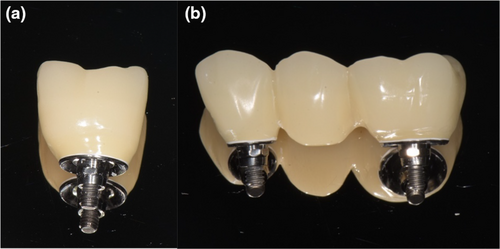
Titanium base abutments are prefabricated standard titanium abutments with an anti-rotational feature and relatively parallel walls in order to support either customized all-ceramic meso-abutments (hybrid abutment) or full-contour crowns (hybrid abutment-crown). In the first scenario, an all-ceramic customized meso-abutment is extra-orally bonded onto the titanium base and then screw-retained on the implant (Figure 1). A separate crown is then intraorally cemented on top of the meso-abutment, with good access to the cementation margins, as the abutment was customized according to the soft tissue profile. Furthermore, a screw access hole can be incorporated into the palatal or occlusal aspect of the crown, allowing to unscrew the entire suprastructure from the implant as a one-piece screw-retained restoration (Edelhoff et al., 2019). However, this methodology is only advisable if the implant axis is in the correct three-dimensional angulation, meaning a screw-access hole in the palatal/lingual (anterior crowns) or occlusal (posterior crowns) aspect. In cases where the access hole would be located on the labial aspect, a conventional cement-retained restoration is preferable.

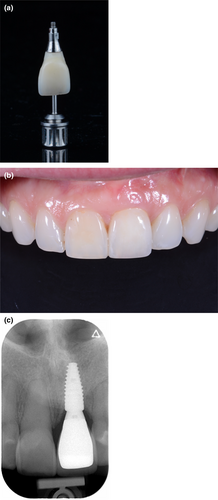
The second scenario consists of a full-contour crown, including the submucosal areas, which is bonded extra-orally to a titanium base abutment and then screw-retained on the implant (Figure 2). An advantage of this approach is the use of only one component, contrary to the two components (meso-abutment and crown) in the first scenario (Edelhoff et al., 2019). Consequently, the production costs may be reduced. However, similar to the 1-piece screw-retained crown from the first scenario, an ideal implant angulation is required from an esthetic point of view.
As hybrid abutment or hybrid abutment-crown, titanium bases represent an interesting alternative to zirconia abutments, as they combine the mechanical stability of a metallic connection (Gehrke et al., 2016) with the esthetic potential of a zirconia superstructure (Vazouras et al., 2022) (Figures 2 and 3). From a purely mechanical standpoint, titanium bases appear to be stable enough to withstand the masticatory forces present in the oral cavity when combined with high-resistance ceramics (Derksen & Wismeijer, 2022; Zhang et al., 2023) (Muhlemann et al., 2020; Pitta et al., 2021) (De Angelis et al., 2020; Elsayed et al., 2018). A recent systematic review showed promising short-term outcomes with an estimated survival rate of 98.6% after 1-year of follow-up (Chantler et al., 2023).
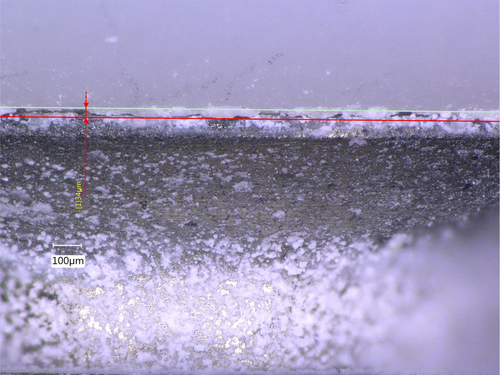
However, concerns were raised regarding the bonding stability between titanium bases and crowns, with the cement interface being suggested as the weakest point of this type of restoration (Pitta et al., 2021). In fact, a large part of the occlusal load during function is likely absorbed by the cement, which may contribute to cement degradation and partial debonding of the crown. Even though this debonding does not necessarily lead to complete loss of retention at an initial stage, it could cause microleakage and plaque accumulation, which in turn increase inflammation in the surrounding tissues (Figure 4). Although the biological implications of cement degradation on the peri-implant tissues are not yet fully clear (Pamato et al., 2020; Rathe et al., 2022), all measures should be applied to reduce the risk of debonding of the crown. Several strategies have been proposed to improve the stability of the bonding interface. On the one hand, an adequate surface treatment of the titanium base is recommended, which may include airborne-particle abrasion (APA) with 50 μm aluminum oxide at 2.5 bar for machined-surface titanium bases (Pitta, Burkhardt, et al., 2020). On the other hand, the choice of primers, bonding agents and cement system should be adapted to the selected ceramic restorative material (Burkhardt et al., 2022). Moreover, the titanium base configuration and height may also play an important role in the overall stability. An increased prosthetic height allows for a larger bonding surface, while straighter and less tapered walls improve retention. Hence, long and cylindrical titanium bases are preferred to short and conical ones.
With regards to the submucosal area, titanium bases with different gingival heights and shapes are often available. Even though very limited data is available on the influence of the gingival or mucosal height on the peri-implant biological outcomes (Linkevicius et al., 2018, 2022), a recent systematic review based on 6 randomized controlled clinical trials (RCT's) suggested a protective effect of longer gingival height abutments (≥2 mm) on the marginal bone level changes (Munoz et al., 2023). This may assume particular importance in cases with a thin tissue phenotype (Linkevicius et al., 2018; Pico et al., 2019). In addition, narrower and concave submucosal shapes are currently preferred as they have shown less marginal bone level changes (Bernabeu-Mira et al., 2023; Perez-Sayans et al., 2022; Valente et al., 2020) and greater mucosal marginal stability (Siegenthaler et al., 2022). In the same vein, steep restorative angles (>30 degrees) may increase the risk for the development of peri-implantitis around bone level implants (Katafuchi et al., 2018; Majzoub et al., 2021; Strauss et al., 2022). Whenever the manufacturers provide multiple titanium base options, these factors should be considered for the selection of the appropriate titanium base.
In situations in which the implant does not allow for a straight screw-access channel, angulated screw-channel abutments can be considered (Kan et al., 2023). Short-term clinical data have shown positive results (Di Fiore et al., 2023; Lv et al., 2021), even though an increased risk of ceramic fracture has been reported in laboratory studies (Drew et al., 2020). Some manufacturers already offer titanium base abutments with angulated screw-channels. However, a potential issue that needs to be investigated is the reduced abutment height due to the angulated screw-channel requiring more space. This might result in reduced surface for retention, which could lead to more frequent debonding (Ibrahim et al., 2023).
2.1.2 Customized CAD-CAM abutments
Although titanium bases can cover a wide spectrum of clinical indications and even be used with angulated screw-channels, depending on the prosthetic options provided by each manufacturer, they may not be the preferred concept in certain clinical scenarios. One aspect which should be considered is the crown-to-abutment ratio (Urdaneta et al., 2010). Very long implant crowns supported by short titanium base abutments may be more prone to bonding failure. In such cases, customized CAD-CAM titanium abutments may still be the first choice to provide an increased support, retention, and bonding area to the restoration (Figure 5). Following the same concept as for titanium bases, a restoration with an occlusal or palatal/lingual screw access hole can be cemented extra-orally to the customized titanium abutment, resulting in a one-piece screw-retained restoration.

Customized CAD-CAM abutment can also be fabricated out of zirconia. The use of full zirconia abutments has been initially proposed to improve aesthetic outcomes in anterior regions (Bittencourt et al., 2023; Ferrantino et al., 2023). While in some studies survival rates are high and comparable to titanium (Ferrantino et al., 2023; Humm et al., 2023; Zembic et al., 2013), other studies reported fractures more frequently (Carrillo de Albornoz et al., 2014; Ferrari et al., 2016). These fractures may be associated with the specific geometry and dimensions of the utilized zirconia connections. Some fractures were even observed while tightening the abutments, which reveals the sensitive handling of this type of abutments (Carrillo de Albornoz et al., 2014, Ferrari et al., 2016). An increased risk of wear of the implant connection is well documented for zirconia abutments (de Holanda Cavalcanti Pereira et al., 2022) Although zirconia customized abutments are a valid solution for anterior aesthetic cases with low mechanical risk (Wittneben et al., 2024), their theoretical esthetic advantages can be surpassed by the use of titanium base abutments, which make their actual indications limited.
2.2 Abutments for implant-supported multiple-unit fixed dental prostheses (FDPs)
For multiple-unit restorations, the use of titanium base abutments is possible, but their selection is determined by the implant parallelism and restoration insertion axis. In cases where multiple implants are not placed ideally parallel, achieving a passive path of insertion, and screw-retention of the prosthesis at implant level may not be possible. The use of abutments with non-engaging or anti-rotational features may help to solve issues of insertion improving the fit of the restoration (Rutkunas et al., 2023). However, some manufacturers only offer short and conical non-indexed titanium bases which may interfere with the bonding stability. Moreover, laboratory studies have shown increased mechanical stability of engaging abutments compared to non-engaging ones (Kwan & Kwan, 2022; Savignano et al., 2021). For these reasons, the combination of engaging with non-engaging titanium bases has been proposed, but research is needed to support this solution.
Another possibility is to restore at the abutment level by using intermediary components, such as multi-unit abutments (MUA), which can compensate for some of the angulation discrepancies. Depending on the desired prosthesis design, a metal framework can be produced which, after being veneered or covered by ceramic crowns, is directly screw-retained onto the MUA. Another possibility is the use of titanium bases onto which monolithic or veneered zirconia prostheses are cemented extra-orally and then screw-retained on the MUA. A commonly raised issue with the use of MUA is the reduced torque allowed on the prosthetic screw, which is reported to increase the risk for screw-loosening (Sánchez-Torres et al., 2021).
From a biological point of view, MUA rarely needs to be removed from the implant and may therefore share some benefits reported by studies of the “one abutment, one time” concept (Atieh et al., 2017). Although the differences in bone level changes may be significant in some studies (Bressan et al., 2017), long-term studies did not show a benefit in clinical outcomes, unless a correction of implant angulation is required (Todisco et al., 2018).
2.3 Provisional abutments
In most of the digital CAD libraries, titanium base abutments remain the only solution for provisional restorations following a fully digital workflow. However, a clinically encountered yet underreported issue is the bonding stability of PMMA materials on titanium bases. Some strategies, including APA of the PMMA intaglio surface and application of a PMMA primer have been suggested (Pitta, Bijelic-Donova, et al., 2020). Still, the use of a conventional provisional cylinder abutment, which can be cut according to the crown dimensions, represents the most reliable solution to avoid debonding (Pitta, Bijelic-Donova, et al., 2020).
3 RESTORATION MATERIAL SELECTION
Today, the definitive restorative materials commonly used in implant dentistry are silicate ceramics, oxide ceramics, and metal-ceramics. Furthermore, a new material class are hybrid materials, in which ceramic structures and polymers are combined (Spitznagel et al., 2018; Zhang & Kelly, 2017). Both dental technician and dentist require detailed knowledge in manufacturing procedures and handling guidelines in order to ensure an optimal material selection tailored to each clinical situation (Zhang & Kelly, 2017). While additive and subtractive manufacturing are both viable techniques for provisional restorations, only subtractive manufacturing (SM) is recommended for definitive restorations at the moment (Derksen et al., 2023). In the posterior region and in patients with lower esthetic expectations, monolithic FDPs can be solely stained and polished, so that veneering is not necessary (Janyavula et al., 2013). If the esthetic outcome is of greater importance, micro-veneering may be applied to the buccal area, not including the incisal edges or occlusal surfaces of the restorations. It seems to be of relevance to maintain the occlusal surface completely monolithic, to prevent fractures of the ceramic veneering. In a recent systematic review for instance, veneered all-ceramic restorations presented significantly higher annual ceramic chipping rates (1.7%) compared to monolithic ceramic restorations (0.4%) (Pjetursson et al., 2021). Additionally, the occlusal surface often remains smoother without veneering and therefore less abrasive to the antagonists (Janyavula et al., 2013).
The buccal micro-veneering is recommended to around a maximum of 0.5 mm thickness in non-functional areas only (Pjetursson et al., 2021). During the computer aided designing, the laboratory technician reduces the buccal volume of the planned restoration performing a so-called “cut-back”, thereby creating space for the following manual micro-veneering.
Even though the indications for metal-ceramic solutions are diminishing, this material nevertheless remains an important treatment option for implant-supported fixed restorations.
The main reasons for a decreased use of metal-ceramic materials are the complexity of the fabrication process, the higher material and fabrication cost and the metallic color. Metal abutments or frameworks may result in a greyish appearance of the surrounding mucosa and match unrestored neighboring teeth less well than all-ceramic restorations (Jung et al., 2008). Also, growing awareness among patients concerning biocompatibility and metal-free solutions resulted in a decreased demand for metal-ceramic options. Different manufacturing methods can be applied for the fabrication of metal-ceramic restorations. Conventional casting of metal frameworks brings challenges especially in regard to the implant-abutment connection, the risk for misfit due to casting distortions and possible material impurities or inhomogeneities. Modern CAD/CAM manufacturing techniques offer the possibility of milling or 3D metal printing instead of traditional casting (Katsoulis et al., 2015; Revilla León et al., 2017). Despite the aforementioned shortcomings, several advantages of metal-ceramic restorations should also be considered. Metal frameworks can be manufactured in extremely thin layers, which is not possible with innately brittle ceramic materials. In extreme cases, the occlusal surface in posterior areas may even be kept in metal, without any ceramic layering. Furthermore, metal occlusal surfaces may be indicated for patients with high masticatory forces, or for patients with severe parafunctions such as bruxism (Misch, 2002; Moshaverinia et al., 2014). In these patients, all-ceramic, metal-ceramic, or metal-acrylic restorations show a higher probability of mechanical and technical complications, such as fractures or cracks, or screw loosening, or screw fractures (Chrcanovic et al., 2017; Häggman-Henrikson et al., 2024; Salvi & Brägger, 2009).
3.1 Implant-supported definitive single crowns (SCs)
For the fabrication of implant-supported SCs, several materials are available today. Due to the small span of implant-supported SCs, lower material strength and mechanical resistance are required compared to medium- and long-span FDPs. Therefore, lithium-disilicate reinforced glass ceramics, oxide ceramics, as well as polymer-infiltrated ceramic network (PICN) materials are proposed options in these cases (Katsoulis et al., 2015, Revilla León et al., 2017).
Lithium-disilicate reinforced glass ceramics exhibit a flexural strength of ~350–400 MPa, which allows its use in a monolithic design. Lithium-disilicate blocks can additionally be used chairside, as they are available in an intermediate crystalline state (and more recently even in a fully crystallized state), which allows for an efficient chairside workflow with reduced laboratory costs and shorter treatment time for the patient. So far, medium-term data on survival and complication rates of all-ceramic monolithic and micro-veneered implant-supported restorations are scarce, and there is a severe lack of long-term data. A recently published systematic review reported promising estimated 3-year survival rates for lithium-disilicate implant-supported SCs (Pjetursson et al., 2021). Veneered reinforced glass–ceramic implant-supported SCs presented survival rates of 97.6%, and monolithic reinforced glass–ceramic implant-supported SCs showed estimated 3-year survival rates of 97.0%. These differences were not statistically significant (Pjetursson et al., 2021).
An alternative material for implant-supported SCs are oxide ceramics (Figures 2 and 3). Among those, 3 mol% yttria-stabilized tetragonal zirconia polycrystal (3Y-TZP) is mostly used in dentistry and is known as a high-strength ceramic, with flexural strengths of ~1000–1200 MPa. Clinically, zirconia-ceramic restorations have proven to be successful and are well documented (Pjetursson et al., 2021; Rabel et al., 2018). The estimated 3-year survival rates of veneered zirconia SCs were found to be 96.3%, whereas the monolithic zirconia SCs presented survival rates of 96.1% (Pjetursson et al., 2021). Likewise to the lithium-disilicate groups, these differences were not statistically significant (Pjetursson et al., 2021). While 3Y-TZP materials are mechanically exceptionally strong, they are also highly opaque and offer a limited esthetic appearance. In order to alleviate this drawback and improve the translucency of zirconia, a higher concentration of yttrium can be used, leading to a partially stabilized zirconia (4–8 mol% yttria-PSZ). While offering greatly improved esthetic characteristics, such PSZ materials also feature reduced mechanical strength (400–800 MPa). Consequently, PSZ materials may offer different and more restricted clinical indications compared to 3Y-TZP. Currently, there is insufficient clinical evidence on the application of these novel zirconia materials for implant-supported restorations. Survival and complication rates will have to be further evaluated scientifically, but care must be taken when choosing a specific composition of zirconia ceramics.
Today, graded zirconia material discs are available, which consist of a progression of chemical composition, shade and translucency within the disc, blending different types of zirconia (usually from 3 to 5 mol % yttria). This allows for more esthetic outcomes, even in a monolithic approach without the need for veneering. Several in-vitro studies reported on fatigue behavior, mechanical, and optical properties of different strength- and color-graded zirconia materials (Marini et al., 2023; Michailova et al., 2020; Spies et al., 2020). One study found higher mechanical properties for monolithic single molar crowns made from strength- and color-graded zirconia, compared to lithium-disilicate crowns serving as control group (Michailova et al., 2020). On the other hand, optical properties such as translucency were lower for the zirconia samples compared to the lithium-disilicate control group (Michailova et al., 2020). Regarding the manufacturing procedures, both lab-side and chair-side solutions are available: Zirconia blocks come in relatively soft pre-sintered stages that require reduced milling time, before then sintering at high temperatures. Furthermore, no negative impact on fracture load or restoration wear was detected when zirconia was sintered at high speed (Michailova et al., 2020).
In esthetically highly demanding areas, an alternative is the directly veneered customized CAD/CAM zirconia abutment. Instead of using a standard titanium base or a metal abutment, a zirconia abutment is designed to be perfectly adapted to the emergence profile and the crown is inserted as a one-piece restoration. Studies on directly veneered zirconia abutments showed excellent clinical results (Fonseca et al., 2021).
Finally, hybrid materials such as hybrid ceramics and resin matrix ceramics (RMC) have been proposed by the industry as an alternative for single-unit implant-supported restorations. An example of a hybrid ceramic is the polymer-infiltrated ceramic network (PICN) material. PICN is formed through the infiltration of a pre-sintered glass–ceramic scaffold with a monomer, followed by secondary polymerization. The ceramic network creates a three-dimensional scaffold of interconnected particles, unlike dispersed fillers. This network acts as a solid skeleton, effectively distributing stresses in all directions and enhancing resistance to structural breakdown phenomena (Mainjot et al., 2016). Furthermore, the elastic modulus of PICN is similar to the one of human dentine. This inherent flexibility of hybrid materials acts as a shock absorber and may lead to more evenly distributed stress during mastication (Coldea et al., 2013). The flexural strength of PICN reaches up to ~160 MPa (Coldea et al., 2013), making this material theoretically sufficiently strong for single crowns on implants, but not larger restorations.
RMC are composed of a monomer matrix (usually dimethacrylate monomers such as urethane dimethacrylate (UDMA), triethylene glycol dimethacrylate (TEGDMA)), and a high concentration of dispersed ceramic filler material. A key advantage of composite resins over many other restorative materials is the facilitated intraoral repairability (Marchesi et al., 2021). Additionally, composite materials have shown to be less abrasive to enamel antagonists (Lawson et al., 2016). Similar to PICN, industrially fabricated RMC materials demonstrate higher flexural strength compared to feldspathic ceramics, although lower than reinforced glass–ceramic materials (Awada & Nathanson, 2015).
Only very few clinical data are available for these rather new hybrid materials, especially in the field of implant dentistry. A significant difference in survival- and complications rates was found between resin-matrix-ceramics and all other ceramic materials in a recent systematic review (Pjetursson et al., 2021). There, a low estimated 3-year survival rate for RMCs of only 36.3% was reported (Pjetursson et al., 2021). The annual fracture rates of the RMC SCs amounted to 6.08%, and the annual complication rate to 15.5% (Pjetursson et al., 2021). One major complication reported was retention loss with 28.19% annually. Biologically, soft tissue complication rates were also higher compared to other ceramic materials, with 6.9% annually (Pjetursson et al., 2021). It has to be taken into consideration, that only two clinical studies on implant-supported RMC SCs were included in this systematic review (Agustin-Panadero et al., 2020; Schepke et al., 2018). More clinical evidence is needed to draw conclusions on the use of RMC and PICN materials for implant-supported SCs, but for the moment these materials cannot be recommended for definitive implant-supported restorations.
In clinical situations with limited vertical space, metal frameworks with partial ceramic veneering remain a valid treatment option, where lingual and palatal aspects of the crowns are kept solely in metal. Furthermore, patients with bruxism could profit from metal frameworks which exhibit high fracture resistances, and occlusal surfaces can be kept in metal without veneering ceramic (Moshaverinia et al., 2014; Zarone et al., 2007). However, generally only very little specific evidence supports an adequate material for implant-supported restorations in patients with bruxism, which limits the recommendations that can be given for this patient group (Chrcanovic et al., 2017; Häggman-Henrikson et al., 2024; Misch, 2002).
3.2 Implant-supported definitive multiple-unit fixed dental prostheses (FDPs)
In contrast to the indications for implant-supported SCs, lithium-disilicate reinforced glass ceramics are not indicated for use in implant-supported multiple-unit FDPs (Sailer et al., 2022). For these restoration types, most long-term evidence is still based on metal-ceramics as restoration material (Pjetursson et al., 2015). In a systematic review on multiple-unit implant-supported FDPs (iFDPs), cumulative survival rates of 98.7% were found for metal-ceramic implant-supported FDPs, while zirconia-ceramic iFDPs showed significantly lower 5-year survival rates of 93% (Sailer et al., 2018). For both materials, ceramic fractures and chipping were the major complication reported. However, zirconia-ceramics presented significantly higher complication rates. In this systematic review, no studies on monolithic zirconia multiple-unit FDPs could be included, due to the lack of published data. Looking at recent promising results on monolithic zirconia implant-supported SCs, it can be assumed that technical complications of zirconia multiple-unit FDPs will decrease when using a monolithic design.
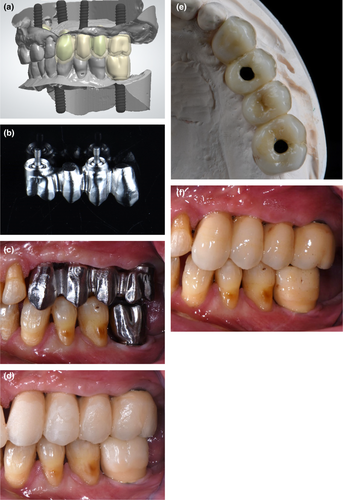
An alternative to the completely monolithic design may be a buccal veneering in esthetically demanding cases, similar to the procedure for SC restorations as described above (Figures 6 and 7).
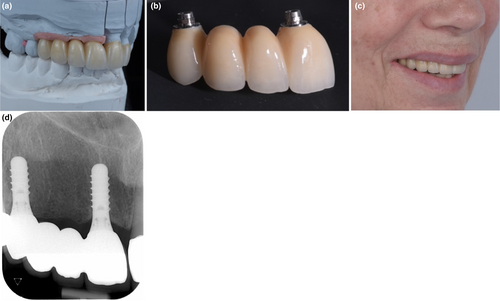
First data on monolithic or micro-veneered iFDPs were evaluated in a recent systematic review focusing on the posterior region (Pjetursson et al., 2023). The authors could include six studies on monolithic or micro-veneered zirconia iFDPs. The findings are in line with the results of the systematic review from 2018, and reported on 98.3% survival after 3 years for PFM iFDPs, 97.5% for zirconia-ceramic iFDPs, and 98.9% for monolithic or buccally micro-veneered iFDPs (Pjetursson et al., 2023). No significant differences in survival were found between groups, but monolithic and micro-veneered zirconia iFDPs exhibited less annual ceramic fracture and chipping rates compared to the other materials. However, it should be noted that different zirconia types are available and not all are indicated for multiple-unit iFDPs. 3Y-TZP zirconia with high flexural strengths, as well as multi-layer combinations of 3- and 5 Y-TZP can be recommended for posterior multiple-unit restorations (Pjetursson et al., 2023).
To overcome possible anatomical limitations regarding hard or soft tissue dimensions or limited available prosthetic space, cantilevered iFDPs may be a valuable solution in certain clinical situations. Because of high masticatory forces in the posterior area, unfavorable biomechanical behavior is expected, especially for iFDP restorations with distal cantilever (de Souza Batista et al., 2017). Mechanical aspects of the restoration materials and cantilever extension lengths have to be considered when planning a cantilevered iFDP. Metal-ceramic implant-supported restorations with metal framework may be used for this indication, with high 5-year survival rates (94.3–99.2%) (Aglietta et al., 2009; Freitas da Silva et al., 2018; Storelli et al., 2018) (Figure 8). However, studies showed that iFDPs with mesial or distal extension are more prone to technical complications, mostly associated with screw-loosenings, ceramic fractures and chippings and can reach up to 45.8% (Palmer et al., 2012; Romanos et al., 2012). Even though very limited data exist on the use of monolithic zirconia bonded to titanium base abutments for cantilever implant-supported FDPs, recent short-term data appear to be promising (Roccuzzo et al., 2023). Concurrently, neither lithium-disilicate nor hybrid materials are indicated as material for cantilevered iFDPs. Very little evidence is available regarding the maximum extension length of the cantilever. One study found a correlation between extension length and occurring technical complications (Kim et al., 2014). Technical complications were found especially in iFDPs with extensions of more than 8 mm (Kim et al., 2014).
3.3 Material selection for provisional implant restorations
Today, a wide range of provisional implant restoration materials are available (Südbeck et al., 2022), with the most prominent groups being acrylates and high-performance polymers from the polyaryletherketone (PAEK) family. Other materials such as polymer-infiltrated ceramic networks (PICN) or composite resins/resin matrix ceramics (RMC) have been proposed by the industry as definitive materials, but may also be suitable for provisional implant-borne restorations. A more detailed discussion of these last-mentioned materials is found in the definitive restoration materials section of this article.
3.3.1 Implant-supported provisional single crowns (SCs)
Polymethyl-methacrylate (PMMA) possesses a range of unique qualities that make it highly suitable and widely adopted as a provisional material. These characteristics include its low density, esthetic appeal, cost-effectiveness, ease of manipulation, and customizable physical and mechanical properties (Alexakou et al., 2019; Cevik et al., 2022; Ionescu et al., 2022). Moreover, several studies demonstrated that industrially fabricated PMMA blocks exhibit reduced toxicity due to their lower residual monomer content (Engler et al., 2020; Shim et al., 2019). Consequently, this decrease in toxicity is reported to reduce the risk of irritating peri-implant tissues and enhances cellular attachment (Shim et al., 2019; Ulker et al., 2009). Notably, CAD/CAM PMMA-blocks have demonstrated superior flexural strength, impact resistance and hardness when compared to conventionally polymerized materials (Alexakou et al., 2019; Sotto-Maior et al., 2019; Südbeck et al., 2022). Clinically, chairside PMMA-based provisionals are usually limited to single unit or small-span implant-supported FDPs. PMMA is thus often considered the gold standard for implant-borne provisional SC (Figure 9a).
High-performance polymers from the PAEK family, such as polyetheretherketone (PEEK) and polyetherketoneketone (PEKK), are synthetic thermoplastic, monochromatic semi-crystalline materials (Chokaree et al., 2022; Suphangul et al., 2022). PEEK has been described as a suitable material for implant-borne provisional restorations and abutments (Kwan & Kwan, 2021). In the long term however, it seems that PEEK loses mechanical stability over time and thus a reinforcement with carbon fibers is desirable for long-term implant-supported provisionals (Suphangul et al., 2022). With similar reasoning, the addition of titanium dioxide particles leads to PEKK showing 80% higher compressive strength than PEEK (Alsadon et al., 2020). PEKK also has a lower melting point than PEEK, thereby facilitating additive manufacturing such as 3D-printing (Zol et al., 2023). Additionally, PEKK does not contain any methacrylate groups and therefore is reported to have better biocompatibility and a lower inflammatory response than PMMA (Cevik et al., 2022). These characteristics may allow PEKK to be used as a material for provisional implant-borne restorations and as a substitute for metals or ceramics, for example, as framework material for removable partial dentures (Alqurashi et al., 2021; Zol et al., 2023), or as precision attachment inserts (Zol et al., 2023). However, more clinical data is required to validate the performance of both PEEK and PEKK, before more precise recommendations can be made.
3.3.2 Implant-supported provisional multiple-unit fixed dental prostheses (FDPs)
Due to the strong mechanical properties of industrially prefabricated CAD/CAM PMMA blocks, this material can be used from single-unit provisional restorations, to long-span FDPs, and even full-arch interim restorations (Blatz & Conejo, 2019; Pyo et al., 2020; Sulaiman, 2020) (Figure 9b). Nevertheless, longer spanning provisional restorations are more prone to fractures than single units, increasing the importance of repairability. PMMA, composites, and high-performance polymers generally offer favorable repairability and relining capabilities, if the surface is properly pre-treated (Soliman et al., 2023; Wiegand et al., 2015). Due to the difficulty of conducting adhesive chemical bonding, surface roughening by air abrasion or diamond bur is highly recommended to maximize micromechanical retention of the repairing composite (Jeong & Kim, 2019; Soliman et al., 2023; Wiegand et al., 2015). Some authors suggested that PMMA can be used as long-term interim restorations for more complex cases with extended treatment time (Alexakou et al., 2019; Güth et al., 2012; Ionescu et al., 2022; Marchesi et al., 2021; Stawarczyk et al., 2015; Zafar, 2020). Both for long-term and long-span implant-supported provisional restorations, the addition of auxiliary reinforcing materials such as graphene may prove beneficial, but more scientific evidence is required in this field (Abad-Coronel et al., 2023).
A recent scoping review reported on three prospective studies and one case report using PEEK as implant framework material for implant-supported FDPs, reporting high survival rates (98.8%) at 12 months. The most frequent complications involved adhesive fractures between framework and veneering material (16%), which are repairable. Nevertheless, more clinical research is needed in order to support the use of PEEK as an (interim) restorative material for implant-borne FDPs (Paratelli et al., 2020). In the same vein, PEKK has been proposed as a material for the fabrication of implant abutments, longer-span implant-retained provisional restorations, frameworks for definitive implant restorations and even dental implants (Alqurashi et al., 2021; Najeeb et al., 2016). However, similar to PEEK, there is very limited evidence on the use of PEKK in implant dentistry at present. Further studies are needed before this material can be clinically recommended for provisional implant-supported FDPs (Cevik et al., 2022; Zol et al., 2023).
4 CONCLUSIONS
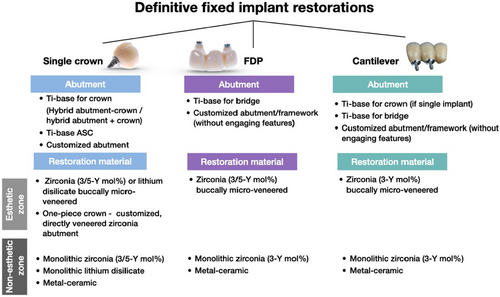
From the abutment to the restoration material, current CAD-CAM materials can cover most of the indications in modern implant prosthetic dentistry (Figure 10). While titanium-base abutments are now widely used, in certain clinical situations, the customization of a titanium abutment still remains beneficial. Improved optical properties of ceramics and attempts to reduce chipping fractures have pushed in the direction of monolithic restoration designs. Still, in the anterior zone and for cases with higher aesthetic demands, a micro-veneering of the buccal areas can be recommended. Even though metallic frameworks are in less demand, this restorative concept still has its justification, for example, in patients with bruxism, minimal prosthetic space, or cantilever iFDPs.
The rapid evolution in digital technology and material manufacturing procedures requires constantly updated research in order to validate their clinical use.
AUTHOR CONTRIBUTIONS
Malin Strasding: Concept/Design, Methodology, Data collection, Data Interpretation, Drafting article, Critical revision of the article. Laurent Marchand: Methodology, Data Interpretation, Drafting article, Critical revision of the article. Elisabeth Merino: Methodology, Data collection, Data Interpretation. Cristina Zarauz: Methodology, Data collection. João Pitta: Concept/Design, Methodology, Data collection, Data Interpretation, Drafting article, Critical revision of the article.
ACKNOWLEDGMENTS
The authors would like to acknowledge the dental laboratory technicians Mr. Cem Piskin, Mr. Elias Bühler and Mr. Vincent Fehmer for their laboratory work on the cases illustrated. Open access funding provided by Universite de Geneve.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.




