Census tract geospatial analysis comparing social determinants of health with tooth loss in California seniors: An ecologic study
Gabriel Tse Feng Chong: The study was conducted at the University of California San Francisco (UCSF)'s School of Dentistry.
Abstract
Objectives
Individual-level social determinant of health (SDOH) measures alone may insufficiently explain disparities in edentulism among seniors. Therefore, the authors examined the correlation of census tract-level SDOH and residential racial segregation measures with edentulism in Californian adults aged ≥65 years old.
Methods
Explanatory variables were obtained from Healthy Places Index (HPI), the National Cancer Institute and diversitydatakids.org. The edentulism outcome variable was obtained from CDC's PLACES small area estimates from the 2018 Behavioral Risk Factor Surveillance System data. Pearson and Spearman rank correlations were estimated. Multiple linear regression and multi-collinearity evaluations were performed. The Global Moran's I statistic assessed partial autocorrelation within census tracts.
Results
Pearson and Spearman correlations were similar, supporting robustness. HPI, an area measure of advantage, strongly negatively correlated with edentulism prevalence [correlation coefficient: −0.87; 95% confidence interval (CI): −0.87, −0.86]. A change of 1.0 in HPI corresponded to an estimated decrease in edentulism prevalence of 5.9% (linear model adjusted R2 = 0.78). Racially segregated census tracts with Hispanics or Blacks alone were positively correlated with edentulism prevalence [0.60, 95% CI: 0.58, 0.62; and 0.33, 95% CI: 0.31, 0.35, respectively]. The converse was seen in census tracts with non-Hispanic Whites alone [−0.57, 95% CI: −0.58, −0.55]. Global Moran's I statistic for edentulism (0.13) and HPI scores (0.19) were significant (both p < .001) indicating geospatial autocorrelation.
Conclusions
Higher disadvantage and minority racial segregation within census tracts were positively correlated with edentulism prevalence. Future research and policy should consider possible interventions improving SDOH to reduce oral health inequities.
1 INTRODUCTION
Total tooth loss (edentulism) in human life course is the end-stage of the two most prevalent oral diseases afflicting humans (dental caries and periodontal disease). Though very rarely life-threatening, edentulism significantly reduces the affected individual's self-image, oral function and oral health-related quality of life.1 Edentulous individuals without dentures are at-risk for poorer nutrition intake and malnutrition resulting in either weight loss or obesity.1-3 A review of the literature also show an association between edentulism and several systemic comorbid diseases, including but not limited to: cardiovascular diseases, gastrointestinal diseases, type II diabetes mellitus, rheumatoid arthritis, chronic obstructive pulmonary disease, Alzheimer's disease and related dementias, chronic kidney disease, obstructive sleep apnoea and even mortality.1-3
As the irreversible end-state of complete tooth mortality, edentulism has been described as the ‘ultimate marker of disease burden for oral health’.4 The most recent Global Burden of Disease Study found that in 2017, edentulism was the leading cause of global oral health associated years lived with disability at 7.3 million (95% uncertainty interval: 4.9–10.4 million),5 affecting an estimated 267 million people (95% uncertainty interval: 235–300 million) with an age-standardized prevalence rate of 3.3%.5 A secondary analysis of the global spatiotemporal trends of edentulism, based on the most recent (2019) Global Burden of Disease study, found that ‘although the age-standardized incidence rate, age-standardized prevalence rate and age-standardized disability-adjusted life years (DALY) rate for edentulism had declined over the past three decades in most countries and regions, the number of prevalent cases and disability-adjusted life years nearly doubled’ and as a result ‘the absolute disease burden due to edentulism was increasing in many countries and regions’.6
In the United States (US), an estimated 17% of seniors in the United States (aged ≥65 years) are edentulous.7 In California, the region of interest for this study, an estimated 8.7% of seniors are edentulous.8 The population edentulism prevalence in the United States is projected to decline gradually to 2.6% by 2050.9 Despite more seniors in the United States retaining their natural teeth,9, 10 disparities in edentulism still persist among this population.10 Edentulism prevalence is three times higher among seniors who have lower income (34%) compared to those who does not have lower income (11%), and among those who received less than a high school education (35%) compared to those who had at least graduated from high school (9%).7 Disparities are also found among the different racial and ethnic groups with non-Hispanic Black older adults being nearly twice as likely (31%) to be edentulous as their Hispanic (17%) and non-Hispanic White (15%) counterparts.10 Rural residency within the United States is another independent correlate for edentulism. After adjusting for socio-economic status, race/ethnicity, age and smoking status, US adults who were partially and completely edentulous are, respectively, 23% and 63% more likely to be living in rural areas.11 A recent secondary analysis using the 2018 Behavioral Risk Factor Surveillance System (BRFSS) data found that adults who are male, non-Hispanic Blacks or more than one race or another racial/ethnic minority, with low socio-economic status are more likely to lose one or more teeth due to caries or periodontal disease than comparable other adults.12
Social determinants of health (SDOH) can be studied at individual and area levels.13 Individual-level SDOH measures alone, such as income, educational level and access to health insurance, may be insufficient to explain disparities in edentulism among seniors in the United States because health results from a complex interplay of SDOH factors operating at both individual and neighbourhood levels.13 Area-level measures of structural SDOH exert important influences on an individual's health outcomes.14, 15 Living in a less well-off neighbourhood means, for example, lower availability and accessibility to resources (such as dentists,16 healthy foods,17 public transportation18 and high-quality public schools19) and conversely greater exposure to advertisements and/or sale of tobacco products,20 alcohol,21 and/or unhealthy fast foods.22, 23 Living in lower income neighbourhoods can also compound the effect of individual-level SDOH factors resulting in increased disparities.14, 15 For example, a study in England found that individuals with low income living in deprived neighbourhoods had worse overall and mental health, whereas low-income individuals living in affluent neighbourhoods did not have similar negative overall and mental health outcomes.15 There are many studies that have studied individual-level SDOH in relation to edentulism,12, 24-27 and one recent study examined state-level measures of structural SDOH and edentulism together.28
Compared to ZIP codes (or ZIP Code Tabulation Areas), using census tracts has several notable advantages providing (i) better and more stable geographical areas over time, (ii) more statistical uniformity in average population size and (iii) more cohesive neighbourhoods. In dental public health research, geographical information systems (GIS) has gained popularity and has been mainly used to map and analyse dental service availability29, 30 and to a lesser extent present spatial differences in oral disease epidemiology,31, 32 across large geographical areas. However, no studies are known to have used GIS to analyse differences in geospatial edentulism patterns across US census tracts. Novel contributions of this study are: (i) assessing GIS used to present edentulism prevalence in California; and (ii) using GIS in dental public health research to test for geospatial autocorrelation.
By addressing the current knowledge gap in epidemiological literature, this study also responds to calls by the US National Institute on Aging (NIA)33 and the National Institute of Dental and Craniofacial Research (NIDCR)34 for ‘inter-disciplinary research into population-level health disparities that affect the overall health of older adults’,33 to potentially identify interventions that can counteract the life-long SDOH effects34 which in the case of oral health may lead to complete tooth loss. In addition to GIS, another advantage of this study is including novel explanatory variables from the socioecologic framework33, 35: (i) composite indices (such as the Healthy Places Index, HPI) to measure resource disadvantage at the neighbourhood level. (HPI covers a wide range of SDOH domains, beyond socio-economics, such as access to supermarkets, parks and points of alcohol sales.); and (ii) residential structural racial/ethnic segregation indices at the neighbourhood level.
The purpose of this study was to investigate the correlation of structural social determinant of health measures with complete edentulism in seniors living in California (aged ≥65 years old). Study objectives were twofold: (i) to analyse the correlation of neighbourhood area (census tract)-level SDOH measures with complete edentulism in seniors living in California, and (ii) to geospatially examine variations and correlations in SDOH and edentulism within California census tracts. The null hypothesis is there is no correlation of neighbourhood-area SDOH measures at the census tract level with prevalence of complete edentulism in seniors living in California.
2 METHODS
The authors adopted a PI/ECOT framework to answer the research question: what is the correlation of neighbourhood-level SDOH measures, such as the HPI and structural residential racial/ethnic segregation, with complete tooth loss in seniors living in California? In this ecological study, the authors included older adults aged ≥65 years old living in California census tracts as the population (P) (note: the primary data sets used 2010 US census tract boundaries) with the following exposures (E): lower HPI status for each census tract. Census tracts with higher HPI status were used as the comparators (C). For the outcome measure (O), the authors considered edentulism in 2018 (T)—which is the most recent data available.
The authors used an University of California San Francisco (UCSF) Institutional Review Board (IRB) self-administered flowchart36 to determine that no IRB review was required as this study did not involve any human subjects or biological specimens, but only publicly available de-identified data sets.
2.1 Outcome variable
The 2021 Centers for Disease Control and Prevention's (CDC) PLACES data set contained small area estimates of prevalence of adults aged ≥65 years having lost all their natural teeth (edentulism) at the census tract level.37 CDC's PLACES 2021 estimates were, in turn, based on data from the 2018 Behavioral Risk Factor Surveillance System (BRFSS).38 CDC's PLACES data ‘provides model-based population-level analysis and community estimates’.38
2.2 Explanatory variables
Explanatory variables at the census tract-level were obtained from the following primary data sets: (i) Healthy Places Index (HPI)39 (Public Health Alliance of Southern California and Virginia Commonwealth University, calculated in 2021 from 2017 data); (ii) the National Cancer Institute's (NCI) SDOH data (calculated in 2021 from the 2008–2012 American Community Survey data)40; and (iii) additional SDOH variables from diversitydatakids.org (Brandeis University, calculated in 2021 from the 2013–2017 American Community Survey data).41
HPI is a composite deprivation score based on 28 census tract-level indicators in eight SDOH domains (economic, educational, healthcare, housing, neighbourhood resources, environment, social and transportation).39 The eight HPI domains broadly cover the Healthy People 2030's five SDOH domains.42 The Yost socio-economic status (SES) index40 is a census tract-level composite SES index derived from seven variables (educational attainment, proportion of people with blue-collar jobs, proportion in the workforce without a job, median household income, proportion <200% of the Federal Poverty Level (FPL), median rent and median house value)43 that the NCI's Surveillance, Epidemiology, and End Results (SEER) program uses to evaluate relationships between SES and cancer incidence and survival.44 Rurality40 is operationalized according to the US Department of Agriculture's Rural Urban Commuting Area (RUCA) codes which ‘classifies US census tracts using measures of population density, urbanization, and daily commuting’45; and specifically the four-category RUCA code ‘reflects the rural nature of the immediate environment and may be most relevant for studies that focus on behaviours and risk’.44 Other neighbourhood (census tract)-level explanatory variables include: percentage attaining different educational levels40; percentage of persons aged ≥65 years living <100% FPL41; percentage of crowded housing units41; percentage of households with no vehicle41; racial/ethnic group percentage in census tracts40; and four residential neighbourhood structural racial/ethnic segregation indices: (i) Location Quotient (for Whites, Blacks, Asians or Pacific Islanders, Hispanics and non-Hispanic Whites); (ii) Index of Concentration at the Extremes (for Blacks, Asians or Pacific Islanders and Hispanics); (iii) Local Exposure and Isolation (for Blacks, Asian or Pacific Islanders, and Hispanics); and (iv) Local Isolation Score (for Whites, Blacks, Asians or Pacific Islanders, Hispanics and non-Hispanic Whites).40
2.3 Data analyses
Multiple linear regression of census tract SDOH measures was undertaken in relation to prevalence of edentulous adults aged ≥65 years old. Edentulism prevalence data and explanatory variables were available for 7998 US census tracts (representing 99.3% of the total of 8057 census tracts in California), so this was the sample size for the analyses. Several multiple linear regression models were developed to assess correlation of edentulism in census tracts with (i) overall advantage of a census tract (HPI and Yost SES Index) and rurality; (ii) the eight HPI domains; (iii) each HPI domain score and their sub-domain variables; (iv) different levels of educational attainment; (v) percentage of different racial/ethnic groups; and (vi) the four different residential racial/ethnic segregation indices. Multi-collinearity among the various SDOH variables was also assessed so models were not collinear—operationalized as variance inflation factors (VIFs) less than 10 and condition numbers (CNs) less than 30.46 Pearson and Spearman rank correlations were compared to assess consistency of parametric versus nonparametric (rank) results. Correlation results were presented in the form of a matrix of scatter plots with Pearson correlations. Statistical analyses were conducted using R (version 4.1.1; The R Foundation for Statistical Computing, Vienna, Austria).
Geospatial (GIS) mapping was undertaken using Tableau (version 2021.2; Tableau Software LLC, Seattle, WA, US) to visualize and map differences in edentulism rates among seniors across California census tracts. GIS enables visualization, mapping and analysis of a broad range of spatial data.47 Spatial autocorrelation of edentulism and HPI scores within California census tracts was assessed using Global Moran's I statistic.48
3 RESULTS
3.1 Descriptive statistics
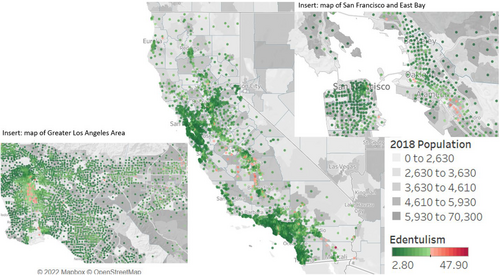
The mean 2018 census tract-level edentulism prevalence among adults aged ≥65 years in California was 11.9% (95% confidence interval [CI]: 8.6%–15.8%). The census tract with the lowest edentulism prevalence was in the city of Manhattan Beach (Los Angeles County) (2.8%; 95% CI: 2.0%–4.8%), and the census tract with the highest edentulism prevalence was Estelle in Imperial County (47.9%; 95% CI: 41.7%–53.5%) (some 200 miles southeast of Manhattan Beach).
3.2 Multiple linear regression and correlation results
Higher advantage in a census tract was negatively correlated with edentulism prevalence (see Table 1). Pearson (r) and Spearman (rs) correlations were similar, thereby showing consistency (robustness) in parametric and nonparametric results. All explanatory variables were assessed for multi-collinearity. All VIFs were less than 10 and CNs less than 30, except for the following variables: (i) percentage of uncrowded households (HPI housing sub-domain39), (ii) percentage of households with kitchen facilities and plumbing requiring repair (HPI housing sub-domain39), (iii) percentage of gross retail, entertainment, and education employment density (HPI neighbourhood sub-domain39), (iv) mean ozone concentration during summer months (HPI pollution sub-domain39), (v) diesel particulate matter emissions (HPI pollution sub-domain39), (vi) attainment of education levels below 12th grade40 and (vii) attended some college but did not graduate.40 The multiple linear model with different levels of educational attainment had the highest CN (27.97) after excluding those explanatory variables with CN more than 30 from the analyses.
| Explanatory variables | Non-standardized multiple linear regression coefficient estimate [95% CI] | Standardized multiple linear regression | ||
|---|---|---|---|---|
| Adj R2 | Coefficient estimate [95% CI] | t Value (all p < .001 unless specified) | ||
| Sources: references s/n 35 & 36 | ||||
| Healthy Places Index (HPI) score: higher score increases advantage | −5.91 [−6.17, −5.65] | 0.78 | −0.54 [−0.56, −0.52] | −45.02 |
| Yost Index for state: 5 quintiles, higher quintile increases advantage | −1.48 [−1.57, −1.38] | −0.35 [−0.37, −0.33] | −29.18 | |
| Rural Urban Commuting Codes (RUCA): higher score implies greater rurality | 0.42 [0.27, 0.57] | 0.03 [0.02, 0.04] | 5.50 | |
| HPI neighbourhood domain and sub-domain variables (source: reference s/n 35) | ||||
| Neighbourhood domain | −1.95 [−2.57, −.133] | 0.15 | −0.13 [−0.17, −0.09] | −6.18 |
| Alcohol access (% of population residing >¼ mile beyond alcohol sales outlet) | −0.05 [−0.06, −0.05] | −0.30 [−0.33, −0.27] | −18.51 | |
| Park access (% living within 1/2 mile park, beach or open-space greater than 1 acre) | −0.02 [−0.02, −0.01] | −0.11 [−0.13, −0.08] | −6.94 | |
| Supermarkets (% of urban and rural population residing less than 1/2 mile or 1 mile, respectively, from a supermarket) | −0.006 [−0.01, −0.001] | −0.04 [−0.07, −0.006] | −2.32 (p = .021) | |
| Tree canopy (population-weighted % of census tract with tree canopy) | −0.05 [−0.07, −0.03] | −0.08 [−0.11, −0.05] | −5.17 | |
| Percentage of attaining different educational levels (source: reference s/n 36) | ||||
| Between 9th and 12th Grade | 0.14 [0.12, 0.16] | 0.69 | 0.15 [0.13, 0.18] | 12.50 |
| High school graduate | −0.10 [−0.12, −0.08] | −0.13 [−0.15, −0.11] | −12.01 | |
| Associate degree | −0.29 [−0.31, −0.26] | −0.16 [−0.18, −0.15] | −22.09 | |
| Bachelor degree | −0.29 [−0.31, −0.28] | −0.55 [−0.58, −0.52] | −39.40 | |
| Master degree or professional degree | −0.18 [−0.19, −0.16] | −0.25 [−0.27, −0.22] | −18.01 | |
| Doctorate degree | 0.02 [−0.02, 0.07] | 0.008 [−0.01, 0.03] | 0.91 (p = .365) | |
| Other SDOH variables (source: reference s/n 37) | ||||
| % of persons aged ≥65 y.o. <100% FPL | 0.17 [0.15, 0.18] | 0.39 | 0.29 [0.26, 0.31] | 26.40 |
| % Crowded housing (defined as >1 person/room) | 0.02 [0.016, 0.017] | 0.36 [0.35, 0.38] | 37.75 | |
| % Households without vehicle | 0.09 [0.08, 0.10] | 0.13 [0.11, 0.15] | 12.26 | |
Both HPI and Yost SES index were very strongly correlated with edentulism prevalence at the census tract-level, with HPI being more strongly correlated [r = −0.87; 95% CI: −0.87, −0.86] (Table S1). A change of 1.0 in HPI and in Yost SES index corresponded to estimated decreases in edentulism prevalence of 5.9% and 1.5%, respectively (linear model adjusted R2 = 0.78) (Table 1). Increased rurality was modestly positively correlated with edentulism [r = 0.11; 95% CI: 0.09, 0.13]. A change of 1.0 in RUCA 4-category score (i.e. increased rurality) corresponded to an estimated increase of 0.4% in edentulism prevalence.
Increased advantage for each of the eight HPI domains was negatively correlated with edentulism (all p < .001) (Figure 1). Amongst the eight HPI domains, the economic domain was the strongest correlate of edentulism prevalence (r = −0.86; 95% CI: −0.87, −0.86) with healthcare access being the next strongest correlate (r = −0.72; 95% CI: −0.73, −0.71) (Table 1). One unit of change in economic domain and healthcare access scores corresponded to an estimated decrease of 4.1% and 1.1% of edentulism, respectively (linear model adjusted R2 = 0.78). Four HPI domains (social, education, housing and transportation) were moderately correlated with edentulism. The remaining two domains (pollution and neighbourhood resources) were weakly correlated with edentulism.

With respect to educational attainment levels (linear model adjusted R2 = 0.69), census tracts with higher percentages of individuals who completed high school or less were strongly positively correlated with edentulism (Table 1). The strongest correlate for edentulism prevalence was education level of 9th to 12th grade [r = 0.74; 95% CI: 0.73, 0.75], where a unit change of 1.0% corresponded to an estimated increase of 0.1% of edentulism prevalence. In contrast, attainment of a bachelor's degree was strongly negatively correlated [r = −0.79; 95% CI: −0.80, −0.78]. A change of 1.0% in bachelor's education attainment corresponded to an estimated decrease in 0.3% of edentulism prevalence. Interestingly, the correlations with edentulism for attainment of master's or professional school degree [r = −0.68; 95% CI: −0.69, −0.67] and doctorate degree [r = −0.44; 95% CI: −0.46, −0.42] were less strong compared to bachelor's degree perhaps due to being less common.
Racially/ethnically residential segregated census tracts with the Local Isolation measure with Hispanics [r = 0.60; 95% CI: 0.58, 0.62] or Blacks alone [r = 0.33; 95% CI: 0.31, 0.35] were correlated with edentulism prevalence (see Table 2 and Table S2). A change of 1.0 in Hispanic alone corresponds to an estimated increase of 2.8% in edentulism prevalence (linear model adjusted R2 = 0.44). For Blacks alone, a change of 1.0 corresponds to an estimated increase of 1.1% in edentulism prevalence. The converse was seen in census tracts with non-Hispanic Whites alone [r = −0.57; 95% CI: −0.58, −0.55], where a change of 1.0 corresponded to an estimated decrease of 1.2% of edentulism prevalence.
| Explanatory variables | Non-standardized multiple linear regression coefficient estimate [95% CI] | Standardized multiple linear regression coefficients | ||
|---|---|---|---|---|
| Adj R2 | Coefficient estimate [95% CI] | t Value (All p < .001 unless specified) | ||
| Percentage of racial/ethnic group in census tracts (source: reference s/n 35) | ||||
| Black | 0.17 [0.16, 0.18] | 0.52 | 0.26 [0.24, 0.28] | 32.39 |
| Asian | −0.04 [−0.05, −0.03] | −0.10 [−0.12, −0.08] | 51.67 | |
| Hispanic | 0.13 [0.13, 0.14] | 0.59 [0.57, 0.61] | 51.67 | |
| Multiple races | −0.13 [−0.22, −0.03] | −0.03 [−0.06, −0.007] | −2.56 (p = .01) | |
| Native American and Alaska Native | 0.74 [0.67, 0.81] | 0.17 [0.16, 0.19] | 22.18 | |
| Native Hawaiian and Pacific Islander | 0.36 [0.19, 0.53] | 0.04 [0.02, 0.05] | 4.21 | |
| HPI and percentage of racial/ethnic group in census tracts (source: reference s/n 35) | ||||
| Healthy Places Index (HPI) score | −8.08 [−8.26, −7.91] | 0.77 | −0.74 [−0.76, −0.72] | −90.97 |
| Black | 0.04 [0.04, 0.05] | 0.07 [0.06, 0.08] | 11.67 | |
| Asian | −0.03 [−0.04, −0.03] | −0.08 [−0.09, −0.07] | −13.86 | |
| Hispanic | 0.03 [0.02, 0.03] | 0.12 [0.10, 0.14] | 12.46 | |
| Multiple races | 0.10 [0.03, 0.17] | 0.02 [0.007, 0.04] | 2.82 (p = .005) | |
| Native American and Alaska Native | 0.24 [0.19, 0.28] | 0.06 [0.04, 0.07] | 9.85 | |
| Native Hawaiian and Pacific Islander | 0.22 [0.10, 0.34] | 0.02 [0.01, 0.03] | 3.73 | |
| Residential racial segregation indices (source: reference s/n 36) | ||||
| Local Isolation Score (LIS)—White alone | −1.09 [−1.53, −0.65] | 0.44 | −0.10 [−0.13, −0.06] | −4.87 (p = .002) |
| LIS—Black alone | 1.05 [0.92, 1.19] | 0.17 [0.15, 0.19] | 15.26 | |
| LIS—Asian or Pacific Islander alone | −1.24 [−1.40, −1.08] | −0.18 [−0.20, −0.16] | −15.00 | |
| LIS—Hispanic alone | 2.79 [2.56, 3.02] | 0.40 [0.37, 0.43] | 23.78 | |
| LIS—Non-Hispanic White alone | −1.15 [−1.42, −0.89] | −0.19 [−0.24, −0.15] | −8.60 | |
| HPI score and residential racial segregation indices (source: reference s/n 35 and 36) | ||||
| HPI score | −8.05 [−8.23, −7.88] | 0.77 | −0.74 [−0.75, −0.72] | −89.01 |
| LIS—White alone | 0.27 [−0.008, 0.56] | 0.02 [−0.0007, 0.05] | 1.91 (p = .06) | |
| LIS—Black alone | 0.37 [0.28, 0.46] | 0.06 [0.05, 0.07] | 8.33 | |
| LIS—Asian or Pacific Islander alone | −0.54 [−0.64, −0.43] | −0.08 [−0.09, −0.06] | −10.07 | |
| LIS—Hispanic alone | 0.46 [0.30, 0.61] | 0.07 [0.04, 0.09] | 5.74 | |
| LIS—Non-Hispanic White alone | −0.56 [−0.73, −0.39] | −0.09 [−0.12, −0.07] | −6.51 | |
When HPI was included in the multiple linear models with racial/ethnic segregation indices, the goodness of fit increased significantly (from adjusted R2 of 0.18 to 0.76 and from 0.46 to 0.77) (see Table 2). In these models, HPI was the strongest correlate for edentulism and adjusting for HPI greatly attenuated the racial/ethnicity relationship to edentulism and likewise the racial/ethnic segregation relationship to edentulism. Notably, the ‘protective’ effect of census tracts with Asian or Pacific Islanders alone against edentulism increases in the models after including HPI and either comes very close or even exceeds the ‘protective’ effect of census tracts with non-Hispanic Whites alone; (the non-standardized coefficient estimates for the model with Local Isolation Score are −0.54 vs. −0.56, respectively. In the model for Local Quotient, the respective non-standardized coefficient estimates are −0.45 vs. −0.39). Refer to the appendix for Figures S1–S13 showing additional matrix of Pearson correlation scatter plots and Tables S1 and S2 showing the standardized and non-standardized multiple linear regression coefficients, Pearson and Spearman correlations and VIFs.
3.3 GIS results
As shown in Figure 2, rural California areas (i.e. outside the main urban centres of the San Francisco Bay Area and San Jose, Greater Los Angeles and the Greater San Diego area) had higher levels of edentulism in 2018, with the highest prevalence in the Central Valley. The Global Moran's I statistic for edentulism (0.13) and HPI (0.19) were statistically significant (both p < .001) indicating geospatial autocorrelation.
4 DISCUSSION
The null hypothesis of no correlation between area SDOH measures and edentulism in adults ≥65 years was rejected based on the results. Higher disadvantage and minority racial segregation for Hispanics or Blacks alone within census tracts were positively correlated with edentulism prevalence. Conversely, census tracts with higher advantage, Asian or Pacific Islander segregation alone, and non-Hispanic White segregation alone were negatively correlated with edentulism. Oral health inequities have been at work for decades by the time a US adult loses any permanent tooth because of caries or periodontal disease.10, 12 This study provides evidence that unless these disparities are eliminated at both individual- and neighbourhood-levels, oral health inequities are almost sure to persist such that individuals are more likely to end up losing all of their teeth if they live in census tracts that (i) are lower-income, (ii) have high percentage of the population facing challenges accessing healthcare, (iii) have high percentage of the population who are less educated (high school and below), (iv) have high percentage of the population living in crowded housing and/or (v) are racially/ethnically segregated. Results could help guide policy makers to provide more resources including prevention and treatment of dental caries and periodontal disease, causes of edentulism, in census tracts with low HPI.
As expected, this study's findings show some similarities in the association between economic advantage and edentulism experience at the individual- and area-level SDOH measures. For instance, a unit increase in economic advantage at the census tract-level corresponds to an estimated decrease of 4.1% in edentulism prevalence; whereas at the individual-level, edentulism rates among seniors who have lower income are three-times higher than those who are not.7 In addition, at the individual-level, non-Hispanic White seniors are half as likely as their non-Hispanic Black counterparts to be edentulous.24 The correlation findings between non-Hispanic White alone (r = −0.57) and Blacks alone (r = 0.33) seem to suggest that a stronger association of edentulism related to being Black is amplified at the census-tract level, perhaps due to access to resources and structural racism. This study therefore provides evidence of neighbourhood-level structural discrimination, in addition to socio-economics, relating to oral health outcomes.14, 49
However, there are some notable differences in this study's findings compared with the literature that have studied individual-level SDOH related to edentulism. At the individual level, non-Hispanic Black seniors have double the chances of being edentulous as their Hispanic and non-Hispanic White counterparts.24 However, this study shows that in California racially segregated census tracts with Hispanics alone (0.60; 95% CI: 0.58, 0.62) had almost double the correlation with edentulism prevalence compared to census tracts with Blacks alone (0.33; 95% CI: 0.31, 0.35). Structural racial/ethnic discrimination measures such as residential segregation at the census tract level (i.e. a more granular level) have been shown to relate more to other health conditions than city or regional segregation levels50; thus, assessing neighbourhood (census tract)-level residential segregation, rather than state-level measures,28 may be a better way to assess structural discrimination.
One hypothesis to explain the differences between the findings for Hispanic seniors compared to non-Hispanic seniors, at the individual and neighbourhood-level, could be due to the underrepresentation of Hispanic individuals among the dental workforce in California.51, 52 For instance, a 2007 study found that while about one-third of Californians are Hispanic, only one out of every 20 (5%) of Californian dentists are Hispanic.51 Furthermore, there is also a disparity in the representation of Hispanic compared to non-Hispanic Black dentists in the California workforce. For example, another study found that in 2020, 8.2% of California's dentists were Hispanic, whereas 39.3% of the state's population were Hispanic.52 On the other hand, while 1.9% of the Californian dentists were non-Hispanic Black, the percentage of non-Hispanic Blacks in the state's population was 6.5%.52 Hence, the disproportion of races/ethnicities in the Californian dental workforce compared to the racial/ethnic proportions in the state were much less for non-Hispanic Blacks (4.6% difference in percentages or a little more than three times) compared to Hispanics (31.1% difference in percentages or about five times). A recent report in 2023 found that ‘factors such as culture, language, immigration policies, anti-immigrant sentiments and racism, in addition to other social determinants of health, are influencing Latinos' inability to access oral healthcare’.53 Presumably, these SDOH factors listed in the 2023 report, especially language, could be amplified at the neighbourhood-level (i.e. neighbourhood-level structural discrimination), which could further explain why Hispanic dentists ‘shoulder a disproportionate share of dental care for minority and underserved communities’54 even though they are ‘drastically’54 underrepresented in the dental workforce.
At the individual level, adults who identify with more than one race have been reported as being more likely to lose one or more teeth due to caries or periodontal disease.12 In contrast, this study shows that census tracts with a higher percentage of people who identify with more than one race have a moderate negative correlation with edentulism prevalence (r = −0.41; 95% CI: −0.43, −0.39). Unfortunately, there is very little research on individuals who identify with more than one race compared to the amount of research available concerning non-Hispanic Whites, non-Hispanic Blacks, Hispanics, and Asian Americans.55 In fact, it was only at the 2000 US census that multi-racial Americans could identify themselves with more than one racial category on the census form.56 Prior to that, individuals who identify with more than one race could only be counted in one racial category.56 Moreover, most studies and data sets include small samples of people who identify as more than one race, meaning estimates have poor precision (large standard errors and wide confidence intervals). Therefore, unlike earlier where the authors could proffer a hypothesis to explain the differences between the findings for Hispanic seniors compared to non-Hispanic seniors at the individual- and neighbourhood-level, because of the paucity of data on people in the United States identifying as multi-racial, the authors have few suggestions of hypotheses for the differences in edentulism prevalence for multi-racial Americans at the individual- and neighbourhood-level.
This study also shows that the census tract-level association of rurality with edentulism is much weaker than at the individual level (r = 0.11; 95% CI: 0.09, 0.13; and non-standardized multiple linear regression coefficient of 0.42) where US adults who were completely edentulous were 62.7% more likely to be living in rural areas.11 Collectively, these differences in this study's findings compared with the literature that have studied individual-level SDOH related to edentulism suggest that individual-level SDOH measures alone may be insufficient to explain disparities in edentulism among older American adults. Unsurprisingly individual- and area-level deprivation measures have been found to be independently associated with other health conditions, such as poor mental health.15 More research on neigborhood-level SDOH factors is needed as there do not appear to be published studies pertaining to access to neighbourhood resources, for example accessibility to dental clinic(s), availability of healthy foods and public/personal transportation, at the individual-level in relation to edentulism.
Edentulism and HPI were both found to be clustered geospatially at the census tract. Future research in this area should take spatial autocorrelation into consideration, for instance, by conducting multi-level linear regressions to account for census tracts' proximity to each other. This study's findings have two potential applications for dental public health practice: (i) with regards to ‘prevention’, this study highlights areas of oral health inequities for policy makers and local community leaders to identify groups at the ‘extreme end of the health continuum’49; and (ii) with regards to ‘supply’, this study allows decision makers to prioritize ‘target populations’ for resource allocation during public oral health program planning. The findings can be used to inform healthcare delivery and policies such that ‘preventive’ and ‘supply’ resources can reach individuals living in the most disadvantaged neighbourhoods, at an earlier part of the dental caries and periodontal disease life course before the condition(s) become so severe that the only ‘treatment’ available is extraction of the diseased tooth. Preventive resources would include, for example, community water fluoridation, school-based sealant programs, addressing the levels of sugar consumption, oral health advocates drawn from the particular racial/ethnic group for those census tracts that are racially/ethnically segregated. Supply resources would include, for example, the availability and accessibility to culturally and linguistically appropriate dental clinics and providers. Of significance, ‘California Local Health Jurisdictions use (the) Healthy Places Index for various purposes’ (written communication on 2nd August 2021, Dr. Jay Kumar, State Dental Director, California Department of Public Health). As such, the hope is that this study's findings may be useful to the California Department of Public Health to work towards achieving one of the Healthy People 2030's objectives (OH-05) to ‘reduce the proportion of adults aged ≥45 years who have lost all their teeth’.57
The additional contributions this paper makes to the literature are (i) the focus on neighbourhood-level factors and including structural racial discrimination measures, in addition to socio-economic ones; and (ii) the use of GIS to present edentulism prevalence in California and to test for geospatial autocorrelation. Nonetheless, this study had some methodological limitations, the main one being ecological fallacy because the people with edentulism in a neighbourhood may not actually experience the neighbourhood-level deprivation; for example, they may work and recreate in neighbourhoods with many resources. Moreover, ecological fallacy applies when the area-level measure is proxy for an unmeasured individual-level measures; in fact, neighbourhood-level factors can contribute independently to health in addition to individual effects so multi-level studies utilizing neighbourhood-level factors actually avoid atomistic fallacy.58 US Census tracts, which have about 4800 residents, have been reported to be the functional size of neighbourhoods,59 which is a strength of this investigation. Second, people move their place of residence throughout their life, so their 2018 census tract at the time of participating in the BRFSS survey may not coincide with where they had spent most of their life and been exposed to the most risk indicators. This information is not captured in the primary data sets; this is also important from a life course perspective because there are associations of SDOH with caries and periodontal disease over individuals' life-courses (both of which ultimately result in tooth loss).60 Another limitation is that the outcome variable was derived in small area analyses from the BRFSS, which is a self-reported sample survey. All self-reported sample surveys are subject to the following errors or biases: (i) non-response bias (i.e. refusal to participate in the survey or to answer specific questions); (ii) systematic error resulting from noncoverage; and/or (iii) measurement biases (i.e. social desirability and/or recall biases). However, BRFSS uses survey science best practices to reduce these biases and their potential impact.
5 CONCLUSIONS
Area (census tract)-level SDOH measures (including, but not limited to, disadvantage and racial/ethnic minority segregation) correlate with edentulism prevalence in California adults aged ≥65 years. As such, future research and policy interventions addressing Healthy People 2030's OH-5 objective (i.e. reduction of edentulism prevalence) should consider possible interventions improving SDOH at both the individual- and neighbourhood-levels to reduce oral health inequities.
ACKNOWLEDGEMENTS
The authors acknowledge the assistance of Albert Lee from the UCSF Library's Data Science Initiative's Consultation Service to troubleshoot R code. Additionally, the authors acknowledge: the Healthcare Delivery Research Program, National Cancer Institute, as the source of NCI SDOH data set and documentation; this data set and documentation were created by Information Management Services, Inc. under US Government contracts HHSN261201500003B/75N91020F00001 to facilitate research activities of the NCI-funded Population-based Research to Optimize the Screening Process (PROSPR) consortium; and that PROSPR grantees, funded under US Government grants U24CA221936, UM1CA221939, UM1CA221940 and UM1CA222035, provided documentation for segregation indices and guidance regarding their creation.
CONFLICT OF INTEREST STATEMENT
The authors declare that no financial support was received for the conduct of this study and that there is no potential conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The primary data sets used in this study are publicly available, and the detailed findings can be found in Appendix S1.