Discovery of Mieap-regulated mitochondrial quality control as a new function of tumor suppressor p53
Funding Information
AMED, (Grant/Award Number: ‘15ck0106006h0002‘) KAKENHI, (Grant/Award Number: ‘22501021‘,’23659178‘,’24240117‘,’25430124‘,’25670169‘)
Abstract
The tumor suppressor p53 gene is frequently mutated in human cancers, and the p53 protein suppresses cancer. However, the mechanism behind the p53-mediated tumor suppression is still unclear. Recently, the mitochondria-eating protein (Mieap) was identified as a p53-inducible protein. Mieap induces the accumulation of lysosomal proteins within mitochondria (Mieap-induced accumulation of lysosome-like organelles within mitochondria, or MALM) in response to mitochondrial damage, and eliminates the oxidized mitochondrial proteins to repair unhealthy mitochondria. Furthermore, Mieap also induces vacuole-like structures (Mieap-induced vacuole, or MIV) to eat and degrade unhealthy mitochondria. Therefore, Mieap controls mitochondrial quality by repairing or eliminating unhealthy mitochondria by MALM or MIV, respectively. This mechanism is not mediated by canonical autophagy. Mieap-deficient ApcMin/+ mice show strikingly high rates of intestinal tumor development as well as advanced-grade adenomas and adenocarcinomas. The p53/Mieap/BCL2 interacting protein 3 mitochondrial quality control pathway is frequently inactivated in human colorectal cancers. Defects in Mieap-regulated mitochondrial quality control lead to accumulation of unhealthy mitochondria in cancer cells. Cancer-specific unhealthy mitochondria could contribute to cancer development and aggressiveness through mitochondrial reactive oxygen species and altered metabolism. Mieap-regulated mitochondrial quality control is a newly discovered function of p53 that plays a critical role in tumor suppression.
Abbreviations
-
- BNIP3
-
- BCL2 interacting protein 3
-
- KD
-
- knockdown
-
- LAMP
-
- lysosomal-associated membrane protein
-
- MALM
-
- Mieap-induced accumulation of lysosome-like organelles within mitochondria
-
- Mieap
-
- mitochondria-eating protein
-
- MIV
-
- Mieap-induced vacuole
-
- ROS
-
- reactive oxygen species
-
- UVRAG
-
- UV radiation resistance associated gene
The tumor suppressor p53 was first discovered in 1979 as an oncoprotein.1-6 Since then, a number of studies have been carried out to clarify the function of p53, resulting in a tremendous number of reports. Currently, the following are believed to be essential for p53: (i) it is a transcription factor that activates the transcription of its target genes by binding to specific sequences;7 (ii) cell cycle arrest, apoptosis, DNA repair, and anti-angiogenesis are the core functions in its tumor suppression;8 and (iii) it is frequently mutated in a broad range of human cancers.9 However, recent studies in murine models have clearly shown that cell cycle arrest and apoptosis are not required for tumor suppression.10, 11 These observations suggested that there is still a missing piece in the mechanism of p53-dependent tumor suppression. Therefore, the importance of p53 in cancer suppression is well established, but its mechanism is still unclear.
As p53 is a transcription factor that regulates a large number of genes, the identification and characterization of these target genes are critically important for understanding its functions.12, 13 So far, a number of p53-target genes have been identified and characterized by us, as well as other groups, as shown in Figure 1. It is known that p53AIP1,14 p53RDL1 (UNC5B),15 Bax,16 Noxa,17 Puma,18, 19 and UNC5A20 are apoptosis inducers, whereas Netrin-1 is an apoptosis inhibitor.21 In addition, p21WAF1,22 14-3-3sigma,23 and Reprimo24 are cell cycle regulators, and p53R2 (RRM2B),25 XPC,26 and GADD4527 are involved in DNA repair. BAI1,28 TSP1,29 and SEMA3F30 regulate anti-angiogenesis, whereas p53DINP1 (TP53INP1)31 and MDM232 are positive and negative regulators of p53, respectively. Both TIGAR33 and GLS234 are involved in metabolism and ALDH435 has anti-oxidant activity. Thus, p53 regulates a huge number of cellular functions through transcriptional activation of its target genes. However, the mechanisms behind the regulation of these multiple functions to suppress cancer, and which targets and/or functions are the most critical for p53 suppression of tumors, are still unclear.
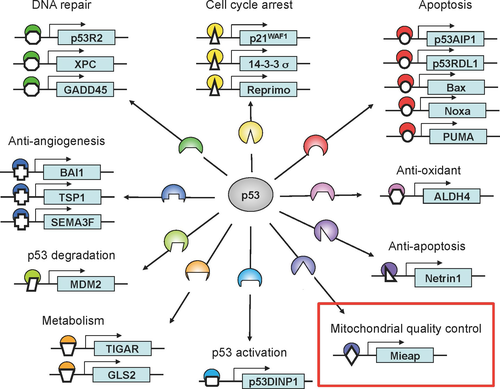
Mieap (the mitochondria-eating protein) was identified as a p53-target gene, and has been found to be frequently inactivated in human cancer cell lines through promoter methylation, implying the role of Mieap in tumor suppression.36 Surprisingly, Mieap was also found to be involved in mitochondrial quality control (Fig. 1).36, 37 Mieap-regulated mitochondrial quality control is frequently inactivated in human cancers. This leads to a striking and specific accumulation of unhealthy mitochondria in cancer cells, and the cancer-specific unhealthy mitochondria generate high levels of ROS. Mitochondrial ROS and abnormal metabolism caused by cancer-specific unhealthy mitochondria probably contribute to cancer development and progression. Mieap-regulated mitochondrial quality control is likely one of the new mechanisms for p53 tumor suppression.
New mechanisms for mitochondrial quality control
Mieap controls mitochondrial quality by repairing or eliminating unhealthy mitochondria through MALM or MIV, respectively (Fig. 2).36, 37 In response to mitochondrial damage, lysosomal proteins are accumulated in the mitochondria in a Mieap-dependent manner. This phenomenon is generally considered as mitochondrial autophagy or mitophagy. However, during this phenomenon, the destruction of mitochondrial structure does not occur in spite of the accumulation of lysosomal proteins.36 In addition, autophagosomes and autolysosomes are not observed through electron microscopic analysis. At least four lysosomal proteins (LAMP1, LAMP2, cathepsin B, and cathepsin D) have been detected within the mitochondria by immuno-electron microscopic analysis, while two lysosomal proteins (cathepsin B and cathepsin D) were shown to be within the mitochondria through a proteinase K protection assay. In brief, in this assay, isolated mitochondria are subjected to proteinase K digestion. The proteins within the mitochondria are protected from degradation. Therefore, after the treatment, the result is rapidly and easily confirmed by Western blot analysis.36 Therefore, this function has been denoted as MALM.
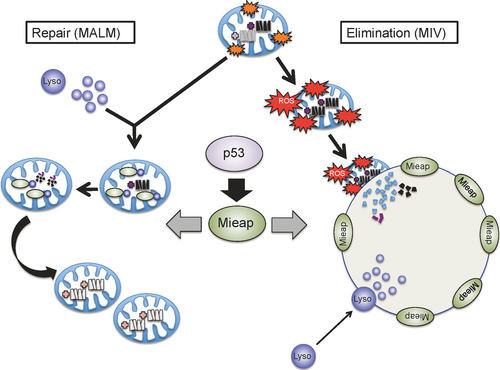
One possible role of MALM is the elimination of oxidized mitochondrial proteins, because oxidized proteins are accumulated in the mitochondria of MALM-deficient cells.36 In addition, mitochondrial ROS levels are known to be higher in MALM-deficient cells.36 These observations suggest that MALM plays a role in the elimination of oxidized mitochondrial proteins to maintain the mitochondrial integrity. Consistent with this hypothesis, MALM has also been reported to improve ATP synthesis activity and decrease mitochondrial ROS generation, thus promoting the health of mitochondria (Fig. 3).36
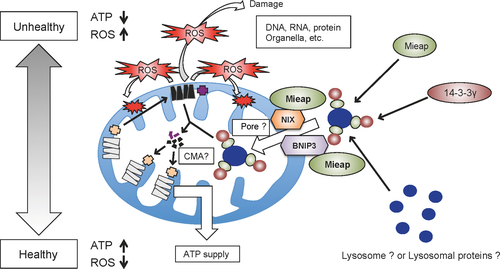
Both BNIP3 and NIX mediate the induction of MALM by interacting with Mieap at the mitochondrial outer membrane in response to mitochondrial damage, mitochondrial ROS generation, and/or hypoxia (Fig. 3).38 The interaction of Mieap, BNIP3, and NIX induces the formation of a pore in the mitochondrial double membrane, which mediates the translocation of lysosomal proteins from the cytosol to the intramitochondrial region.38 Interestingly, the pore formed by the interaction of the three proteins is not associated with cell death.38
In contrast, 14-3-3γ was also identified as a Mieap-interacting protein, but its role was found to be critically different from that of BNIP3 and NIX.39 It was found that 14-3-3γ interacts with Mieap in the cytosol, and then translocates into the mitochondria.39 It then mediates the lysosomal degradation of the oxidized mitochondrial proteins within the mitochondria (Fig. 3).39
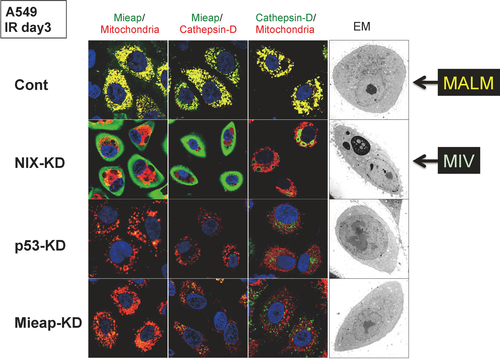
Mieap-induced vacuoles are vacuole-like structures (Fig. 4).37 They ingest and degrade unhealthy mitochondria by accumulating lysosomes.37 Mieap-induced vacuoles can be produced by the overexpression of Mieap in various cancer cell lines, but not in normal cell lines. This is due to the difference in the mitochondrial ROS levels between cancer cells and normal cells.37 Reactive oxygen species scavengers (ebselen and N-acetylcysteine) efficiently inhibit MALM induction and degradation of mitochondria by MIV.37 Therefore, high levels of mitochondrial ROS may play a critical role in targeting unhealthy mitochondria by MALM and MIV.
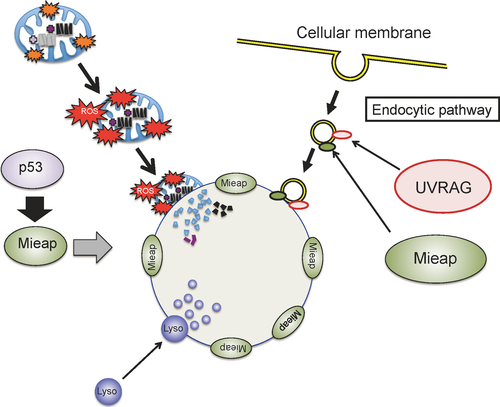
We found that UVRAG40 mediated the formation of MIV (2016) (Fig. 4). It was previously reported that UVRAG regulates the maturation of endosomes and autolysosomes.41, 42 The formation of MIVs is inhibited by phosphatidylinositol 3-kinase inhibitors, including 3MA and LY294002.37 Therefore, the endocytic pathway may be involved in the generation of MIVs (Fig. 4). The UVRAG gene has been reported to be mutated in the cancer cells of a small proportion (3%–5%) of colorectal cancer patients.43
When MALM is inhibited, MIV generation is induced through endogenous Mieap (Fig. 5).37 This implies that the highly dangerous and unhealthy mitochondria that MALM is unable to repair produces high levels of ROS, and are thus eliminated by MIV. Because the knockdown of p53 and/or Mieap in A549 cells completely inhibited the induction of both MALM and MIV, the mechanisms of MALM and MIV are probably strictly regulated by the p53/Mieap-regulatory pathway (Fig. 5).37 These facts strongly suggest that p53 maintains mitochondrial integrity through transcriptional activation of Mieap, which regulates the mitochondrial quality control.
In general, quality control of the mitochondria is regulated by the canonical autophagy of mitochondria, known as “mitophagy”.44 In this mechanism, the damaged mitochondria are sequestered by double-membraned autophagosomes; the autophagosomes containing the damaged mitochondria then fuse to lysosomes and turn into autolysosomes in order to degrade the autophagosomal content. Therefore, double-membraned autophagosomes are essential for canonical mitophagy. Additionally, the process is very rapid and is completed within a few hours.45, 46 In contrast, in Mieap-regulated mitochondrial quality control, autophagosomes and autolysosomes are not involved in MALM or MIV.36, 37 These processes are relatively slow and continue for 24–72 h.36, 37 Furthermore, Parkin and Pink1 have been established to play a pivotal role in mitophagy.47-50 However, they are not involved in MALM or MIV. These facts clearly suggest that Mieap-regulated mitochondrial quality control is critically different from the canonical autophagy of mitochondria, mitophagy.
Mieap-deficient colorectal cancer mouse model
In order to clarify the in vivo role of Mieap in tumorigenesis, we developed a strain of Mieap KO mice. Mieap KO mice were born normally and were able to grow after birth. Using these Mieap KO mice, we generated Mieap-deficient ApcMin/+ mice.51 ApcMin/+ mice develop multiple benign tumors in the small intestine, and are therefore a murine intestinal tumor model.52, 53 Mieap-deficient ApcMin/+ mice showed a much shorter lifetime compared to the Mieap-WT ApcMin/+ mice.51 This was due to substantially higher number and size of intestinal tumors in Mieap-deficient ApcMin/+ mice.51 Moreover, intestinal tumors in the Mieap-deficient ApcMin/+ mice showed more advanced grades of adenomas and adenocarcinomas than Mieap-WT ApcMin/+ mice.51 These results clearly suggest that Mieap deficiency promotes cancer development and malignancy in vivo.
Interestingly, the mitochondria in cancer cells of Mieap-deficient ApcMin/+ mice were morphologically abnormal, suggesting that Mieap deficiency leads to the accumulation of unhealthy mitochondria in cancer cells, thus causing increased oxidative stress in Mieap-deficient tumors.51
The results from the studies on Mieap-deficient ApcMin/+ mice suggest that the inactivation of the Mieap-regulated mitochondrial quality control leads to accumulation of unhealthy mitochondria and increased mitochondrial ROS generation, which probably promotes cancer development and aggressiveness in vivo.
Mieap-regulated mitochondrial quality control is frequently inactivated in human colorectal cancer
The promoter for the Mieap gene is frequently methylated in various human cancer cell lines, resulting in the loss of Mieap expression in cancer cell lines.36 To evaluate the status of the methylation of Mieap promoters in primary cancer tissues, we examined primary cancer samples from 57 colorectal cancer patients.54 We observed promoter methylation of Mieap in only 5 out of 57 patients (9%). In contrast, the promoter methylation of BNIP3 was found in 28 out of 57 patients (47%). p53 Mutation was found in nearly 50% of colorectal cancer tissues that did not show methylation of the Mieap and BNIP3 promoters. These results indicate that the p53/Mieap/BNIP3-regulated mitochondrial quality control pathway is inactivated in more than 70% of colorectal cancer patients.54 Therefore, BNIP3 is probably the most important target for inactivation of Mieap-regulated mitochondrial quality control in human colorectal cancers.
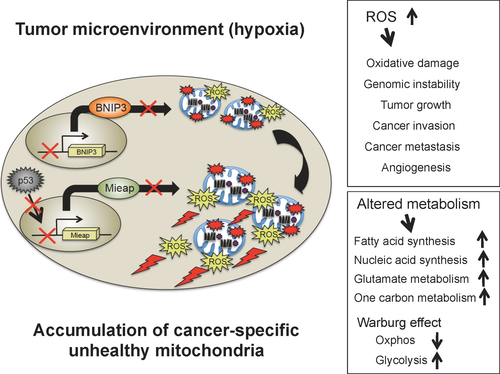
As a BH3-only protein that belongs to the Bcl-2 family, BNIP3 is believed to play a critical role in necrosis-like cell death under hypoxic conditions by causing the opening of mitochondrial permeability transition pores.55, 56 However, our recent study clearly showed that BNIP3 mediates MALM through pore formation by interacting with Mieap and NIX, and that these pores are not mitochondrial permeability transition pores.38 Knockdown of BNIP3-knockdown (KD) in LS174T colorectal cancer cell lines severely impaired mitochondrial localization of Mieap, resulting in the inhibition of MALM induction.54 The MALM-deficient cancer cells (p53-KD, Mieap-KD, and BNIP3-KD cancer cells) accumulated unhealthy mitochondria and these cancer-specific unhealthy mitochondria produced high levels of ROS under hypoxia.54 Interestingly, BNIP3-KD colorectal cancer cells as well as p53-KD and Mieap-KD cells showed a striking enhancement of migratory and invasive activities in hypoxic conditions.54 The enhanced migration and invasive activities of these cancer cells were dependent on increased generation of mitochondrial ROS.54
These observations from human colorectal cancer tissues clearly support our hypothesis that the Mieap-regulated mitochondrial quality control is frequently inactivated in human cancers in vivo, leading to the accumulation of unhealthy mitochondria producing high levels of ROS. These cancer-specific unhealthy mitochondria could greatly contribute to cancer development and aggressiveness through oxidative stress and abnormal metabolism (Fig. 6).
Implications and future directions
Discovery of Mieap as a p53-target gene opens up a new avenue for exploration of the mechanism behind p53 tumor suppression, in which mitochondrial quality control plays a critical role in tumor suppression. Inactivation of Mieap-regulated mitochondrial quality control results in the accumulation of unhealthy mitochondria in cancer cells. These cancer-specific unhealthy mitochondria produce high levels of ROS and cause abnormal metabolism, both of which would be beneficial for cancer progression. The Mieap-regulated mitochondrial quality control is inactivated in human gastric cancers, breast cancers, and pancreatic cancers (2016). Mieap-deficiency also promotes cancer development, aggressiveness, and malignancy in mouse models of gastric cancer (Tsuneki, Nakamura, and Arakawa, 2016). Therefore, p53/Mieap-regulated mitochondrial quality control plays an important role as a universal tumor suppressor in a broad range of human cancers.
Nearly 38 years after its discovery, the full mechanism for p53 tumor suppression remains unknown. Emerging evidence is suggesting that metabolic regulation and cellular redox control are additional core functions for this mechanism.57, 58 Mieap-regulated mitochondrial quality control is involved in both of these functions, because inactivation of the Mieap pathway in cancer cells results in the accumulation of unhealthy mitochondria, causing abnormal metabolism and increased oxidative stress. Therefore, the maintenance of mitochondrial integrity by p53 seems to be critical for the suppression of cancer development and progression.
In fact, many p53-target genes are known to be involved in the maintenance of mitochondrial integrity. p53R2 (RRM2B) was initially identified as a ribonucleotide reductase that supplies dNTPs for DNA repair.25 However, germ-line mutations of p53R2 were found in many patients with mitochondrial diseases, suggesting that p53R2 is essential for the supply of dNTPs for mitochondrial DNA synthesis.59 This implies that p53 also controls mitochondrial DNA synthesis through p53R2.59 In p53-mutated cancers, the concentration of dNTPs is dysregulated, leading to high rates of mutation of mitochondrial DNA and increased mitochondrial ROS generation. Aldehyde dehydrogenase 4 is an antioxidant in the mitochondria that effectively scavenges mitochondrial ROS.35 Glutaminase 2 also functions as an antioxidant protein in the mitochondria, catalyzing the hydrolysis of glutamine to glutamate.34 CABC160 encodes coenzyme Q10 and SCO261 catalyzes the synthesis of cytochrome c oxidase 2, both of which are key components in the oxidative phosphorylation chain. Based on these facts, we propose a hypothesis that tumor suppressor p53 is the guardian of the mitochondria.
Mutation of p53 and/or Mieap/BNIP3 promoter methylation leads to the accumulation of unhealthy mitochondria in cancer cells (Fig. 6). “Unhealthy mitochondria” are still functional, but produce lower levels of ATP and higher levels of ROS. They are not equivalent to “abnormal mitochondria” that are severely damaged, pathological, and non-functional, and fail to produce ATP due to dissipation of the mitochondrial membrane potential. Abnormal mitochondria are eliminated through Parkin/Pink1 pathway-mediated canonical autophagy (mitophagy).44, 47-50 Using electron microscopy, we further confirmed that unhealthy mitochondria in cancer cells are round and enlarged, and have a very poor cristae structure (2016). This may reflect the roles of these mitochondria in cancer metabolism and redox status. Therefore, we define these mitochondria as “cancer-specific unhealthy mitochondria.”
We observed that cancer-specific unhealthy mitochondria are accumulated in nearly 100% of cancer cells in the tumor microenvironment, and that this phenomenon is common in a broad range of human cancers (Nakamura, Tsuneki, and Arakawa, 2016). Cancer-specific unhealthy mitochondria produce high levels of ROS under the in vivo hypoxic tumor microenvironment (Fig. 6).62 The elevated mitochondrial ROS causes oxidative damage to the DNA, RNA, proteins, and lipids.63 This induces genomic instability. The mitochondrial ROS contribute to tumor growth, epithelial–mesenchymal transition, cancer invasion, cancer metastasis, and tumor angiogenesis through the activation of hypoxia-inducible factor-1, nuclear factor-κB, MMPs, AKT, Erk1/2, and JNK (Fig. 6).64-72 Cancer-specific unhealthy mitochondria also cause abnormalities in the metabolism, such as activation of fatty acid synthesis, nucleic acid synthesis, glutamate metabolism, one carbon metabolism, defective oxidative phosphorylation, upregulation of glycolysis, and reduction in activity of the TCA cycle (Fig. 6).73-76 We speculate that cancer-specific unhealthy mitochondria function as a driving force for cancer development and progression. Further comprehensive and careful investigation on cancer-specific unhealthy mitochondria would help in identification and characterization of molecules, signaling pathways, and metabolites that compose cancer's Achilles heel. For instance, an antibody against a molecule(s) localized in cancer-specific unhealthy mitochondria could be used to detect cancer cells during pathological diagnosis, thus acting as a novel biomarker(s). Inhibitors against oncogenic signaling pathways or oncometabolites derived from cancer-specific unhealthy mitochondria would be useful as new anticancer drugs. Therefore, the development of a method to target cancer-specific unhealthy mitochondria could provide new strategies for the prevention, diagnosis, and therapy of a broad range of human cancers.
Acknowledgments
We thank all of the members of Arakawa's Laboratory for their pivotal contributions to this work, who are largely responsible for discovery of the Mieap function. This work was supported in part by the Japan Society for the Promotion of Science (KAKENHI Grant Nos. 24240117 to H.A., 22501021 to Y.N., 23659178 to H.A., 25430124 to Y.N., and 25670169 to H.A.), the Ministry of Health, Labor and Welfare of Japan for the Practical Research for Innovative Cancer (H26-practical-general-001 to H.A.), the National Cancer Center Research and Development Fund (Grant No. 23-B-7 to H.A.), and the Japan Agency for Medical Research and Development (AMED Grant No. 15ck0106006h0002 to H.A.).
Disclosure Statement
The authors have no conflict of interest.