Paediatric ischaemic stroke is a valid diagnosis in the Swedish National Patient Register
Funding information
AW: A private donation through the Knut and Alice Wallenberg Foundation for research on stroke and stroke-causing factors in infancy, A grant from the Region Östergötland Research Council. KS: A private donation through the Knut and Alice Wallenberg Foundation for research on stroke and stroke-causing factors in infancy. MG: None. PB: A private donation through the Knut and Alice Wallenberg Foundation for research on stroke and stroke-causing factors in infancy. HEKS: A private donation through the Knut and Alice Wallenberg Foundation for research on stroke and stroke-causing factors in infancy, A grant from the Region Östergötland Research Council. None of the funders had any role in the study's design and conduct; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Abstract
Aim
The Swedish National Patient Register offers unique opportunities for epidemiological research of paediatric ischaemic stroke. We aimed to validate the diagnosis of paediatric ischaemic stroke in the National Patient Register to ensure the quality of future research.
Methods
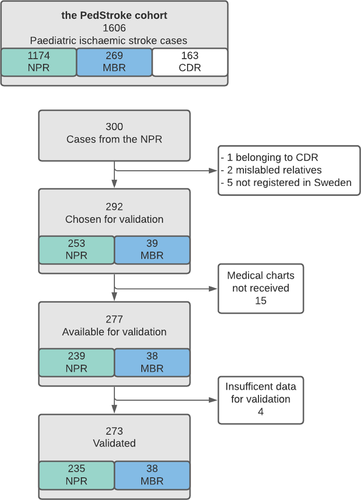
The PedStroke cohort consists of 1606 individuals aged <18 years with a diagnosis of paediatric ischaemic stroke (ICD-10: I63, I64; ICD-8 and 9: 433, 434, 436) in Swedish national health registers between 1969 and 2016. We selected 292 cases for validation by reviewing medical charts.
Results
In all, 277 of the 292 medical charts were received, of which 273 had enough information to qualify for review. The diagnosis was correct in 242/273 cases, yielding a positive predictive value (PPV) of 89% (95% confidence interval (CI): 0.85–0.92) for paediatric ischaemic stroke in the National Patient Register. After validation, seven cases of 222 with childhood stroke were re-categorised to perinatal stroke, resulting in a total of 56 perinatal stroke cases. In the Medical Birth Register, 38 stroke cases were identified of which 37 had correct diagnosis, generating a PPV of 97% (95% CI: 0.92–1.0). Incorrect diagnoses decreased over time and the number of diagnoses confirmed by radiology increased correspondingly.
Conclusion
The National Patient Register is reliable for epidemiological research of paediatric ischaemic stroke because of its high PPV for this diagnosis.
Abbreviations
-
- CI
-
- Confidence Interval
-
- ICD
-
- International Classification of Diseases
-
- MBR
-
- Medical Birth Register
-
- NPR
-
- Swedish National Patient Register
-
- PPV
-
- Positive Predictive Value
Key Notes
- There is a high positive predictive value of 89% for the diagnosis of paediatric ischaemic stroke in the Swedish National Patient Register, where radiological findings confirm 95% of all validated stroke diagnoses.
- The Swedish National Patient Register is reliable for epidemiological research in paediatric ischaemic stroke.
- Paediatric ischaemic stroke cases entailed 19% perinatal and 81% childhood strokes; however, validation showed that 3.6% of the latter in fact had perinatal stroke.
1 INTRODUCTION
Ischaemic stroke in children is less recognised than ischaemic stroke in adults, although stroke risk is greatest during the first week of life.1 The incidence declines during childhood but often resulting in lifelong disabilities,2 including neuromotor difficulties, language problems, intellectual disabilities, behavioural disorders and epilepsy.3, 4
Paediatric ischaemic stroke is a cerebral insult caused by ischaemia in an individual aged <18 years, typically verified and dated by imaging techniques.5 It can be divided into two subgroups: perinatal stroke, which occurs from 22 weeks gestation until the 28th day of life, and childhood stroke, which occurs after the 28th day of life until 18 years of age.6
Epidemiological studies are essential to gain knowledge of risk factors and ischaemic stroke outcomes in childhood. The Swedish national health registers, recognised worldwide, are of high quality and their national coverage is good.
The Swedish National Patient Register (NPR), for instance, has almost complete coverage (99%) of all Swedish inpatient care, and a primary diagnosis is listed in more than 99% of hospital discharges making the NPR reliable in identifying individuals with different diseases. Registry studies of paediatric cohorts are uncommon, and only a few diagnoses have been validated in the NPR. However, the PPV in most adult diagnoses ranges from 85% to 95%.7
The basis of register studies is high validity in diagnosis. Our main aim was therefore to validate paediatric ischaemic stroke in the NPR.
2 PATIENTS AND METHODS
The PedStroke cohort was created for epidemiological research and consists of all children, from 0 to 18 years of age, registered with ischaemic stroke in the NPR, Medical Birth Register (MBR) and Cause of Death Register between 1969 and 2016. In all, 1606 children were identified with paediatric ischaemic stroke (ICD-10: I63, I64; ICD 8 and 9: 433, 434, 436). To reduce the diagnostic error rate cerebral ischaemia in the newborn (ICD 10: P91.0) and other four-character diagnosis were not used.8 The NPR was established in 1964 with full national coverage of all inpatient care since 1987. Hospital-based outpatient care has been included since 2001. Reporting to the register is mandatory for doctors in both general and private health care while primary care is excluded.9 Diagnoses are based on the Swedish version of the International Classification of Diseases (ICD). The MBR, which includes data on more than 99% of all deliveries in Sweden, was introduced in 1973.10 The Cause of Death Register contains data since 1961 with a loss of only 1%–2% the latter years.11 These registers render data throughout the patient's life and by linkage through the Multi Generation Register12, 13 also on morbidities and mortalities of first degree relatives.
Patients in the PedStroke cohort were chronologically arranged based on the diagnosis date, to validate individuals in proportion to the incidence of the NPR. Every 5th person was selected to gain a sufficient number (n = 300) of cases for validation. After sorting the raw data, seven cases were excluded because they did not meet the criteria as an index patient in the PedStroke cohort. One additional case was ruled out because it was registered in the Cause of Death Register only. Thereafter, 292 individuals remained for validation; 39 of these individuals were also identified in the MBR (Figure 1).
The National Board of Health and Welfare provided the unique personal identification numbers given to all permanent residents of Sweden allowing medical records and radiology reports to be retrieved from the hospitals where the individuals were diagnosed. Administrative personnel in each region or centre were contacted personally, and formal requests were sent by regular mail or telefax. If the medical records were missing or found insufficient, contact was repeated by telephone, e-mail, regular mail, or a combination of these options for at least three times or until complete information was retrieved.
A clinical report form was developed to enable structured medical records analysis. Two researchers, both residents in paediatrics, reviewed the medical records overseen by an experienced paediatric neurologist. Date of birth, sex, symptoms and onset date, radiology reports and dates, ICD diagnosis and date of diagnosis were collected. From radiology reports, the radiologist's conclusion as well as the findings supportive thereof was denoted in the report form.
Paediatric ischaemic stroke was, as proposed by the American Heart Association/American Stroke Association, defined as cerebral cell death caused by ischaemia, confirmed either by (i) imaging or other objective evidence of cerebral insult in a vascular distribution or (ii) symptoms or other clinical signs of cerebral insult lasting ≥24 hours or until death with other aetiologies excluded.5 According to this, three levels of certainty for paediatric ischaemic stroke were defined: (i) Stroke: cerebral ischaemia as confirmed through radiology (MRI, CT or angiography); (ii) Probable stroke: Radiology was not accessible but the clinical course, treatment and judgement at the time of diagnosis were consistent with stroke and no other diagnosis was more likely; and (iii) Possible stroke: A stroke diagnosis noted in the medical records but data were insufficient to confirm or rule out the diagnosis. Stroke and Probable stroke were considered a correct diagnosis.
Incorrect diagnoses were classified as (i) Diagnostic error: The patient was erroneously diagnosed with stroke and received an ICD diagnosis of stroke in medical notes and the NPR. (ii) Translational error: A correct diagnosis and equivalent ICD code in the medical chart correspond to a different ICD code in the NPR, noting the patient wrongfully in the register as having had a stroke; and (iii): Coding error. A correct diagnosis but an incorrect ICD code was given in the medical notes and transferred to the NPR.7
2.1 Statistical analysis
We estimated that there would be approximately 2950 children with stroke in the Swedish national registers between 1969 and 2016. Based on previous validations of the NPR showing an 85%–95% PPV, we aimed to demonstrate a 90% PPV for stroke with a 95% CI range of 85%–95% (with an alpha of 0.05 and a beta of 0.20). Calculation with EpiTools14 (‘sample size for single proportions’) showed that 139 medical records were needed for validation. We aimed to identify 300 cases due to the expected loss of data.
The main outcome is PPV for the diagnosis of paediatric stroke in the NPR. All calculations were made with IBM SPSS Statistics for Windows, Version 24.0 (Armonk, NY: IBM Corp).
2.2 Ethical approval
The study was approved by the Regional Ethics Committee, Linköping (2017/31-10). Individual informed consent was not required as this is a retrospective study solely including anonymised data.15
3 RESULTS
Of the 292 requested medical records, 277 were retrieved (Figure 1). The others were reported as missing from the medical archives. Of these 277 medical records, 273 had sufficient information for validation, and in 4 cases, there were insufficient data to complete the clinical report form.
The distribution of sex and age at stroke diagnosis was similar in our validated cohort and the PedStroke cohort (Table 1).
|
Validated index individuals in the NPR n (%) |
All index individuals n (%) |
||
|---|---|---|---|
| All | 273 | 1606 | |
| Sex | Male | 151 (55) | 862 (54) |
| Female | 122 (45) | 744 (46) | |
| Age at diagnosis of stroke | Perinatal (≤28 days) | 51 (19) | 367 (23) |
| Childhood (>28 days) | 222 (81) | 1239 (77) | |
| Period of diagnosis | 1969–1986 | 30 (11) | 193 (12) |
| 1987–1996 | 108 (40) | 394 (25) | |
| 1997–2016 | 135 (49) | 1019 (63) |
- Abbreviation: NPR, National Patient Register.
Of the 273 medical records, a stroke diagnosis was confirmed in 242 cases and in 231 of those cases radiological findings supported the diagnosis (Table 2). Among the 231 radiologically confirmed cases, original radiology reports were accessible in 208 cases while for the remaining 23 radiology was quoted or summarised by a doctor in the medical record. Cases confirmed by radiology increased over time for both registers and in correspondence the number of probable strokes decreased over time (Table 3).
| NPR | MBR | ||||
|---|---|---|---|---|---|
| n (%) | PPV (95% CI) | n (%) | PPV (95% CI) | ||
| All | 273 | 38 (14) | |||
| Correct diagnosis | Alla | 242 (89) | 89% (0.85–0.92) | 37 (97) | 97% (0.92–1.0) |
| Stroke | 231 (85) | 85% (0.8–0.89) | 36 (95) | 95% (0.88–1.0) | |
| Probable strokeb | 11 (4) | 1 (3) | |||
| Undecided | All | 0 | 0 | ||
| Possible Strokec | 0 | 0 | |||
| Incorrect diagnosis | All | 31 (11) | 1 (3) | ||
| Diagnostic error | 7 (2) | 0 | |||
| Translation error | 9 (3) | 0 | |||
| Coding error | 15 (6) | 1 (3) | |||
- Abbreviations: MBR, Medical Birth Register; NPR, National Patient Register; PPV, Positive predictive value.
- a Includes all stroke and probable stroke cases.
- b Symptoms, disease course and treatment consistent with stroke but no confirming radiology.
- c Symptoms, disease course and treatment possibly stroke, not possible from medical data to confirm or discard diagnosis.
|
All n |
Incorrect diagnosis n (%) |
Correct diagnosis | |||||
|---|---|---|---|---|---|---|---|
| Stroke |
Probable stroke n (%) |
||||||
|
Radiology reporta n (%) |
Radiology in medical recordb n (%) |
||||||
| NPR | All periods | 273 | 31 (11.4) | 208 (76.2) | 23 (8.4) | 11 (4.0) | |
| 1997-2016 | (ICD 10) | 135 | 7 (5.2) | 114 (84.4) | 12 (9.0) | 2 (1.5) | |
| 1987–1996 | (ICD 9) | 109 | 20 (18.3) | 77 (70.6) | 7 (6.4) | 5 (4.6) | |
| 1969–1986 | (ICD 8) | 29 | 4 (13.8) | 17 (58.6) | 4 (13.8) | 4 (13.8) | |
| MBR | All periods | 38 | 1 (2.6) | 35 (92.1) | 1 (2.6) | 1 (2.6) | |
| 1997- 2016 | (ICD 10) | 26 | 0 (0) | 26 (100) | 0 (0) | 0 (0) | |
| 1987–1996 | (ICD 9) | 11 | 1 (9.1) | 8 (72.7) | 1 (9.1) | 1 (9.1) | |
| 1969–1986 | (ICD 8) | 1 | 0 (0) | 1 (100) | 0 (0) | 0 (0) | |
- Abbreviations: ICD, International Classification of Disease; MBR, Medical Birth Register; NPR, National Patient Register.
- a Confirmed by radiology report.
- b Confirmed by radiology recounted in the medical record.
The aetiology of stroke was divided into arterial ischaemic (90%), venous infarctions (6%) and anoxic brain damage (4%). The arterial ischaemic cases were caused by or related to thromboembolism, infection, inflammation, ECMO treatment, cardiac catheterisation, cardiac surgery, vascular anomalies, coagulation disorders and, in one case, as a side effect of medication. However, in most cases, no known cause could be identified. For anoxic brain damage, all cases were identified by radiology with an overall ischaemic picture. The ICD diagnosis was assigned to individuals of this group as a brain death diagnosis under Swedish directives.
Most incorrect diagnoses were coding errors (15/31). There were four intracerebral pathologies though not ischaemia-related, three cases of periventricular leukomalacia, two cases with a foreign body in the trachea, two stemming from venous thrombosis and some random errors. In translational error cases (9/31), the diagnosis intended in the medical record had an ICD diagnosis similar to a stroke diagnosis (eg ICD 8 and 9: 463 Tonsillitis). Diagnostic errors were least common (7/31) and most recent, with five of those being diagnosed in 1997 or later. Four of the incorrect diagnoses were given as a preliminary diagnosis of stroke. The other three were given different incorrect diagnoses (see Table S1).
The PPV of paediatric ischaemic stroke in the NPR was 89% (95% CI: 0.85–0.92) when including all cases clinically judged as stroke (Table 2). For cases established by radiology, the PPV was 85% (95% CI: 0.8–0.89). In the MBR, the corresponding PPVs were 97% (95% CI: 0.92–1.0) and 95% (95% CI: 0.88–1.0). When analysing perinatal and childhood stroke in the NPR separately, the PPVs were 96% (95% CI: 0.91–1.0) and 84% (95%CI: 0.79–0.89), respectively (Table 4).
| NPR | MBR | ||||||
|---|---|---|---|---|---|---|---|
|
According to register n (%) |
Only correct diagnoses n (%) |
After validation n (%) |
PPV (95% CI)a |
According to register n (%) |
Only correct diagnoses n (%) |
After validation n (%) |
|
| Perinatal (≤28 days) | 51 (19) | 49 (20) | 56 (23) | 96% (0.91–1.0) | 38 (100) | 37 (100) | 37 (100) |
| Childhood (>28 days) | 222 (81) | 193 (80) | 186 (77) | 84% (0.79–0.89) | 0 (0) | 0 (0) | 0 (0) |
| Total | 272 (100) | 242 (100) | 242 (100) | 38 (100) | 37 (100) | 37 (100) | |
- Abbreviations: MBR, Medical Birth Register; NPR, National Patient Register; PPV, Positive predictive value.
- a Calculated by ‘only correct diagnoses’ and diagnosis ‘according to register’ for perinatal stroke and 'after validation' and diagnosis ‘according to register’ for childhood stroke.
After reviewing the medical records, the number of cases classified as perinatal stroke in the NPR increased from 49 to 56, constituting almost a fourth of the cohort (23%). For cases with first stroke diagnosis in the MBR, all cases were classified as perinatal stroke and remained after validation.
The most common symptoms of perinatal stroke were seizures, followed by altered consciousness and one case of paresis. The most common symptom in childhood stroke was hemiparesis, followed by seizures, altered consciousness, headache and impaired speech (Table 5). Onset symptoms did not differ regardless of arterial, venous or anoxic aetiology.
| Symptom |
Perinatal strokea n = 56 (%) |
Childhood strokea n = 186 (%) |
|---|---|---|
| Hemiparesis | 1 (2) | 132 (71) |
| Central facial palsy | 0 (0) | 75 (40) |
| Other cranial nerve palsies | 1 (2) | 21 (11) |
| Seizures | 48 (86) | 53 (28) |
| Headache | 0 (0) | 51 (27) |
| Altered consciousness | 20 (36) | 89 (48) |
| Impaired speech | 0 (0) | 49 (26) |
| Vertigo | 0 (0) | 25 (13) |
| Ataxia | 0 (0) | 5 (3) |
| Impaired balance | 0 (0) | 16 (9) |
| Loss of vision | 0 (0) | 10 (5) |
- a Stroke categories according to medical chart review.
4 DISCUSSION
After validation by review of medical charts, we demonstrated a PPV of 89% for paediatric ischaemic stroke in the NPR.
Only a handful paediatric diagnoses have been validated in the NPR before our study. Recently, the diagnosis of intussusception was found to have a PPV of 87%.16 This PPV agrees with our study and is consistent with findings reported in adult diagnoses in which the PPV ranges between 85% and 95% in the NPR.7 Stroke in adults has been shown to have a PPV of 88%. However, this number includes both ischaemic and haemorrhagic stroke.17
Separately analysing perinatal and childhood stroke in the NPR revealed PPVs of 96% and 84%, respectively. Upon verification, seven (3.6%) cases with childhood ischaemic stroke in the NPR were in fact perinatal. The diagnoses in medical records and later in the national registers are not made at the time of stroke but at discharge or at a similar event. Thus, having only register-based data makes it difficult to discern perinatal stroke cases from the childhood stroke group.10
As a substantial number of cases were first registered with ischaemic stroke in the MBR, we choose to analyse these separately. Analyses showed the MBR surpassing the NPR with a PPV of 97%, although only a small number of cases were validated. Not surprisingly, all strokes were classified as perinatal and remained so after verification, which confirms its high validity, although the MBR probably contains only a fraction of all stroke cases.
Radiology was decisively the highest diagnostic level of certainty. Even in the early years, 84% of the correct diagnoses were radiologically confirmed, increasing numbers over time to 98% after 1997, implicating increased accessibility and use of CT and MRI. All children diagnosed after 1997 underwent radiology; however, in a few cases, it was not confirmative or conclusive but did neither rule out ischaemia; therefore, clinical information and other investigations led to a final diagnosis. In our material, absence of radiology reports was not a cause of diagnostic error. Time from onset of the disease until diagnostic radiology was not an outcome in our study, but it is obvious to the researchers that there is a delay in radiology compared to Swedish national guidelines for acute stroke management in children.18 If suspicion of stroke is low or moderate, radiology examination may be abstained or postponed in children as MRI often requires sedation. Poor sensitivity for acute-phase ischaemia on CT scans and that not all Swedish hospitals have access to round-the-clock MRI make up part of the explanation, although, in centres with all the necessary facilities the diagnosis is also known to be delayed. In one study, only one fifth of the cases was diagnosed within 6 hours, that is within the time limit for acute intervention, and several studies report long delay to radiology.18-20
For cases with sufficient data for validation, no cases were left undecided regarding a potential diagnosis of ischaemic stroke. The gravity of a stroke diagnosis probably leads to continued diagnostics until confirmed or ruled out in most cases. In addition, there is an advantage in the retrospective review, which yields information over an extended period. Late effects and investigations well beyond the acute setting can be used to confirm an earlier diagnosis.
Two of the four-character diagnoses in our definition of ischaemic stroke are also used for brain death diagnosis (ICD-10; I63.8, I63.9), according to Swedish clinical directives.21, 22 Hence, anoxic brain damage is included in the material but only in a few cases (9/242). However, exclusion of these four-character diagnoses would lead to a substantial loss of stroke cases.
Most diagnostic errors were made in later years, largely because diagnoses were decided too quickly. Although the investigations revealed a different diagnosis, the stroke diagnosis remained, still indicating a stroke incorrectly. Because diagnoses are rarely removed from medical records, the best option is to abstain from making a diagnosis until further diagnostics can be performed. Meanwhile, a symptom diagnosis could be applied. It can be challenging to use the coding system correctly but it is vital for both the patient and the registers to maintain high quality. Instructions on how to code and why it is important should be taught in and after medical education.
Most errors leading to an incorrect diagnosis are coding errors, in our material as well as the National Board of Health and Welfare's analysis of the NPR performed in 1990. Overall, paediatric diagnoses had an error rate of 15% in 1990, making paediatric ischaemic stroke one of the more reliable paediatric diagnoses.8 The reason is probably that stroke is a severe condition often managed by paediatricians specialising in neurology. It has been shown that validation of stroke in adults registered in neurology departments have a higher PPV than if registered in other departments.23
Coding and translational errors are due to administrative- and register-related issues. From 1969 to 1980, most of the regions used manual forms for data transcription from each hospital discharge.24 Technical improvements and implementation of electronic medical records have improved these issues significantly.
Symptoms at stroke onset, described in the medical records, confirmed the different presentations of perinatal and childhood ischaemic stroke. Most perinatal ischaemic strokes had seizures at onset as expected6 and a third altered consciousness but there were almost no other onset symptoms in this group. The onset symptoms of childhood stroke are more diverse.25 The three most common symptoms in our material were hemiparesis, altered consciousness and central facial palsy as expected. However, other less common onset symptoms are probably underestimated in medical records. The severe and apparent first symptoms may undervalue more subtle neurological symptoms, even though noted later in the diagnostic process.
Unfortunately, we do not have detailed data on stroke aetiology since the retrieval of complete medical records is difficult and we strived to achieve a small loss of patients over detailed data on just a few.
The greatest strength of the study is that over 90% of the requested medical records were retrieved. The loss is minor in comparison with the analysed material. A unique cohort was used for this validation as it is population-based and dates back to 1969. A sizeable percentage of the stroke cases could be confirmed by radiology over the years, consolidating the correct diagnosis.
We identified, however, far fewer individuals with paediatric ischaemic stroke than expected. Calculating from incidence rates in other studies, we estimated that we would identify approximately 2 950 paediatric ischaemic stroke cases.25, 26 One reason for this discrepancy might be the NPR's low coverage until 1987 when national coverage was reached. From 1983, 85% of all somatic diagnoses were registered.8 This rate is compatible with our material with very few cases in the earlier years. Meanwhile, health care also developed owing to improved diagnostics as well as knowledge and attention to paediatric ischaemic stroke diagnosis.
Our reviewing researchers worked in close collaboration with frequent discussions, and in all unclear cases, consensus decisions were made. Hence, an inter-rater evaluation could not be done. Nevertheless, 95% of the diagnoses were supported by radiological findings considerably decreasing the room for disagreement regarding the stroke diagnosis.
A weakness of all register-based research is the dependence on ICD codes and its correct use in medical records. To reduce the error rate, we choose to use ICD codes on a three-character diagnosis category level (eg ICD-10: I63 cerebral infarction).8 Unfortunately, this approach denies the possibility of including ICD diagnosis of the four-character category level, capturing more specific cases (eg cerebral ischaemia in the newborn, ICD 10: P91.0). Therefore, some perinatal strokes are not identified, underestimating this group in our material. However, excluding the diagnosis prevents the material from being diluted by false-positive cases which could lead to smaller differences between groups in case-control studies. Moreover, the number of unknown cases cannot be assessed. It is difficult to know the reason why unretrievable medical records could not be identified, although diagnoses were missing from eight regions in Sweden, making systematic error less likely. However, false-negative cases may only have a marginal effect because paediatric stroke is rare.
With our definition of the PedStroke cohort, we have achieved a group of children with a large true-positive diagnosis that we deem most important for reliance on further research of the material. These results enable studies of a disease to rare to gather large material through prospective inclusion although common enough to bear a significant burden of disease.27
We conclude that the Swedish national health registers have been found to identify paediatric ischaemic stroke accurately and are therefore an extremely valuable research tool.
ETHICS APPROVAL
This project (2017/10-31) was approved by the Research Ethics Committee in Linköping, Sweden on 23 January 2017.
CONFLICT OF INTEREST
None of the authors have anything to declare.