Retinal oxygen saturation before and after glaucoma surgery
Abstract
Purpose
This study compared retinal vessel oxygen saturation before and after glaucoma surgery.
Methods
Retinal oxygen saturation in glaucoma patients was measured using a non-invasive spectrophotometric retinal oximeter. Adequate image quality was found in 49 of the 108 consecutive glaucoma patients recruited, with 30 undergoing trabeculectomy, 11 EX-PRESS and eight trabeculotomy. Retinal oxygen saturation measurements in the retinal arterioles and venules were performed at 1 day prior to and at approximately 10 days after surgery. Statistical analysis was performed using a Student's t-test.
Results
After glaucoma surgery, intraocular pressure (IOP) decreased from 19.8 ± 7.7 mmHg to 9.0 ± 5.7 mmHg (p < 0.001). Although oxygen saturation in retinal arterioles remained unchanged before and after surgery (104.7 ± 10.6% before and 105.4 ± 9.3% after surgery, p = 0.58), the oxygen saturation in the venules increased from 54.9 ± 7.4% to 57.4 ± 5.7% (p = 0.01).
Conclusion
Intraocular pressure (IOP) decreases caused by glaucoma surgery had an effect on the retinal venous oxygen saturation.
Introduction
Presently, there has been increasing evidence that dysregulation of the retinal blood flow may very well be an important factor for glaucoma. New developments and advances in spectrophotometric retinal oximeter technology have opened up the possibility of using this device to non-invasively measure the retinal oxygen saturation in glaucoma patients. Studies that examined the oxygen saturation in the venules have reported finding higher saturation in patients with poor visual fields versus those having good visual fields (Olafsdottir et al. 2011) or as compared to healthy individuals (Olafsdottir et al. 2014). Furthermore, studies have also reported finding a positive correlation between the oxygen saturation in retinal venules and the worsening visual field mean defect (Olafsdottir et al. 2011; Vandewalle et al. 2014). We have also examined advanced glaucomatous visual field defects and found that there was an association with the increased oxygen saturation in the venous vessels and the decreased arteriovenous difference in the oxygen saturation (Shimazaki et al. 2016). The results of these studies suggest that there are changes in the oxygen metabolism in the glaucomatous retina and that these changes might possibly be related to retinal ganglion loss. However, there have only been a few reports that have investigated the association between glaucoma treatments and the oxygen saturation of the retinal vessel. The primary aim of glaucoma therapy is to lower the IOP. One of the ways used to achieve this is to perform glaucoma surgery. Therefore, this study examined changes in the retinal vessel oxygen saturation before and after glaucoma surgery.
Materials and Methods
This study was conducted in accordance with the principles outlined in the Declaration of Helsinki and was approved by the Ethics Committee of Kagawa University Faculty of Medicine. All patients provided signed informed consent prior to all surgeries and examinations and after being given an explanation of both the purpose of the study and the procedure that was to be used. This study has been registered at ClinicalTrials.gov (NCT02318641).
Subjects
A total of 116 eyes of 108 consecutive glaucoma patients who underwent glaucoma surgery (trabeculectomy, EX-PRESS shunt surgery, trabeculotomy) at Kagawa University Hospital between January 2015 and September 2015 were enrolled in the study. The EX-PRESS glaucoma filtration device was used in all subjects who had a history of vitreous surgery or had severe vision loss of their fellow eye. Prior to the surgery, all of the patients had been using topical glaucoma drugs. At the time of the postoperative oximetry, none of the patients was using glaucoma drugs. All patients were administered a topical corticosteroid (four times daily) and an antibiotic. If a fundus photograph or a clear enough image could not be obtained to analyse the oximetry, the eye was excluded. Measurements for the IOP and blood pressure (BP) and for the oxymap T1 (oxymap ehf., Reykjavik, Iceland) were performed on the day before and at 10 days after the surgery.
Image acquisition for retinal oximetry
The oxymap T1 device, which is composed of two digital cameras, an image splitter and two narrow band-pass filters, was attached to a fundus camera (TRC-50DX; Topcon, Tokyo, Japan). The oxymap T1 device is able to simultaneously capture two fundus images at two different wavelengths of light (570 nm and 600 nm). Based on the two images that were acquired at the 570 and 600 nm wavelengths, the software algorithm automatically calculated the optical density and the ratio of the optical density for each retinal vessel.
After performing mydriasis using 0.5% of tropicamide and 0.5% of phenylephrine hydrochloride (Mydrin-P; Santen, Osaka, Japan), the eye undergoing surgery was examined by the oxymap T1 device in a dark room. For image acquisition, the flash intensity of the oxymap T1 was set at 50 Ws, with a small aperture and large pupil settings applied to the fundus camera. After centring on the optic disc, 50° fundus images were obtained by the oxymap 1.
Oxygen saturation measurement from acquired images
All acquired fundus images were processed by the built-in oxymap Analyzer software (version 2.4.2, oxymap Ehf). This software uses two wavelengths (570 nm and 600 nm) to calculate the optical density of the retinal vessels. The optical density ratio for these two wavelengths exhibits an inverse and approximately linear relationship with the oxygen saturation.
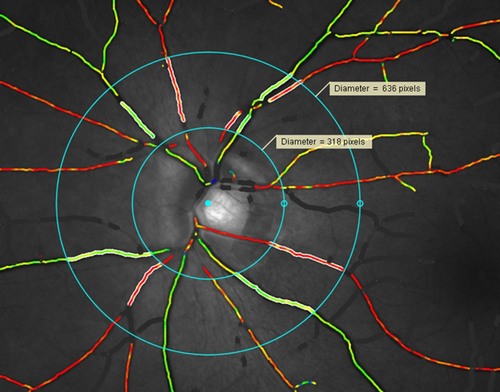
All of the major retinal arteries and veins that were more than six pixels in vessel width within the measurement zone were analysed for oxygen saturation. Each of the sections that were measured had to have a length of more than 50 pixels. A standardized method was used by all of the evaluators when analysing the vessel segments. After centring the disc within a 1.5–3-disc diameter area to avoid uneven retinal background reflections near the optic disc margin, vessel selection was then performed (Fig. 1). For each analysis, we manually excluded all branches and vessels that crossed within the measurement area. Once the vessel sections were determined for the analysis, the oxymap Analyzer automatically measured the oxygen saturation levels. The image quality was measured with the latest oxymap software (version 2.5.1). The image quality was evaluated by three categories: overall, contrast and focus. For all images, it was necessary to have an overall image quality that was >5 in order to be used in the present analysis.
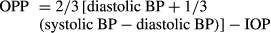
Calculation of ocular perfusion pressure
Statistical analysis
All of the statistical analyses were carried out using spss Statistics version 21 (spss Inc., Chicago, Illinois, USA). Data collected before and after the surgery were compared using a paired t-test. p values <0.05 were considered significant.
Results
Table 1 summarizes the baseline characteristics. After the exclusion of 67 eyes from the analysis due to the poor optical quality of the eye caused by cataract, we enrolled 49 eyes of 49 patients in the study. The image quality is shown in Table 2. The image quality did not change with surgery. Of this group, 39 patients underwent trabeculectomy, 11 underwent EX-PRESS shunt surgery and eight underwent trabeculotomy.
| Total number of patients | 49 |
| Gender (male/female) | 21/28 |
| Age (years) | 64.6 ± 11.6 |
|
Mean deviation (dB) Glaucoma diagnosis |
−14.9 ± 8.1 |
| POAG | 20 |
| NTG | 16 |
| Secondary glaucoma | 7 |
| Exfoliation glaucoma | 4 |
| Steroid glaucoma | 1 |
| Developmental glaucoma | 1 |
| Glaucoma medication | |
| PGA | 44 |
| β blocker | 45 |
| CAI | 38 |
| Brimonidine | 27 |
| ROCK inhibitor | 10 |
| Glaucoma surgery | |
| Trabeculectomy | 30 |
| EX-PRESS | 11 |
| Trabeculotomy | 8 |
- POAG = primary open-angle glaucoma, NTG = normal-tension glaucoma, PGA = prostaglandin analog, CAI = carbonic anhydrate inhibitor, ROCK = Rho-associated kinase.
| Before | After | p value | |
|---|---|---|---|
| Overall | 6.25 ± 1.05 | 6.13 ± 0.95 | 0.54 |
| Focus | 8.03 ± 0.70 | 7.79 ± 0.66 | 0.06 |
| Contrast | 6.81 ± 0.98 | 6.81 ± 0.84 | 0.97 |
After the glaucoma surgery, the mean IOP decreased from 19.8 ± 7.7 mmHg to 9.0 ± 5.7 mmHg (p < 0.001), while the mean OPP increased from 44.2 ± 11.0 mmHg to 49.8 ± 10.4 mmHg (p = 0.002; Table 3). No changes were observed for the oxygen saturation in the retinal arterioles before (104.7 ± 10.6%) and after (105.4 ± 9.3%) the surgery (p = 0.58). In the venules, the oxygen saturation increased from 54.9 ± 7.4% to 57.4 ± 5.7% (p = 0.01) after the glaucoma surgery (Table 4). Although the diameter of the artery did not change after the surgery, the diameter of the vein increased from 152.2 ± 12.7 μm to 162.2 ± 19.5 μm (p = 0.001) after the glaucoma surgery (Table 4).
| Before | After | p value | |
|---|---|---|---|
| IOP (mmHg) | 19.8 ± 7.7 | 9.0 ± 5.7 | <0.001 |
| BP (mmHg) | |||
| Systolic | 128.2 ± 16.5 | 121.2 ± 17.3 | 0.013 |
| Diastolic | 79.9 ± 11.7 | 71.7 ± 12.5 | <0.001 |
| OPP (mmHg) | 44.2 ± 11.0 | 49.8 ± 10.4 | 0.002 |
- IOP = intra ocular pressure, BP = blood pressure, OPP = ocular perfusion pressure.
| Before | After | p value | |
|---|---|---|---|
| SaO2 (%) | |||
| Arterioles | 104.7 ± 10.6 | 105.4 ± 9.3 | 0.58 |
| Venules | 54.9 ± 7.4 | 57.4 ± 5.7 | 0.01 |
| Vessel diameter (μm) | |||
| Artery | 113.5 ± 15.9 | 115.9 ± 18.2 | 0.20 |
| Vein | 152.2 ± 12.7 | 162.2 ± 19.5 | 0.001 |
Discussion
As the purpose of this study was to investigate the influence of the IOP on the retinal vessel oxygen saturation, we combined data of three different surgeries. Oxygen saturation in the arterioles remained stable and exhibited no changes after glaucoma surgery. However, an increase in the oxygen saturation in the venules was observed in conjunction with the lowering of the IOP that was related to the surgery. Kuerten et al. (2015) recently demonstrated that the significant improvement in the retinal blood flow after trabeculectomy appeared to be related to the decrease in the IOP and the subsequent increase in the OPP. A previous study additionally reported that the amount of oxygen that could be delivered was dependent upon the blood flow and the arteriovenous difference in the oxygen saturation (Grieshaber & Flammer 2005). Thus, the oxygen extraction from the retinal circulation to the tissue should be dependent on the retinal blood flow. Berisha et al. (2005) previously examined glaucoma patients and reported that trabeculectomies improved the ocular blood flow. Therefore, increases in the retinal blood after surgery would be expected to lead to a decrease in the oxygen extraction from the retinal circulation.
Hardarson et al. (2009) examined glaucoma filtration surgery and found that it had no effect on retinal vessel oxygen saturation. The discrepancy between our study patients and those for the Hardarson et al. (2009) study may be related to the different populations examined and the use a different oximeter. Several investigators have recently examined deeper glaucomatous visual field defects and reported finding an association with higher retinal oxygen saturations in the venules (Olafsdottir et al. 2011, 2014; Vandewalle et al. 2014). Furthermore, the results of other studies have suggested that retinal oxygen saturation in the venules might also be affected by ageing (Geirsdottir et al. 2012; Mohan et al. 2015). The previously noted differences between our current study and the Hardarson et al. (2009) study might additionally indicate that the oxygen saturation levels in the venules before a surgery can affect the postsurgical results.
There were some limitations with regard to our current study. First, the blood flow velocity was not measured in this study. If, in addition to the oximetry, we had also performed direct measurements of the blood flow, this could have helped us achieve a better understanding of how the oxygen saturation in the venules is affected after a reduction of the IOP. In addition, we have also combined data from several types of glaucoma, which may differ in the pathogenesis, and data from different surgical techniques. Thus, this might limit the general applicability of the results. Another potential limitation involves the glaucoma drug treatment and the postoperative drug treatment. All patients were administered a topical corticosteroid and an antibiotic after surgery. Therefore, we cannot ignore the possibility that these medications might have influenced the oxygen saturation. As our patients were receiving glaucoma drug treatment before but not after the surgery, there is a chance that this also could have influenced the oxygen saturation. Moreover, several medications are known to influence the retinal blood flow, which can lead to an effect on the retinal oxygen saturation (Siesky et al. 2008; Traustason et al. 2009). In addition, while the majority of our patients were using ocular β-blockers before surgery, these were not used after the surgery. Therefore, the cessation of this medication could have increased the BP after surgery. However, BP was decreased after surgery in our patients. It should also be noted that we measured the retinal oxygen saturation only at 10 days after the surgery. Thus, we cannot deny the possibility that the increased oxygen saturation that we observed in the venules after surgery could have been a temporary phenomenon. In future, we will need to undertake additional studies that perform evaluations of the long-term effect of glaucoma surgery on the retinal vessel oxygen saturation. And finally, approximately 60% of the eyes were excluded because of poor imaging quality. Therefore, it might be possible that those exclusions could have biased our results.
In conclusion, the lowering of the IOP by glaucoma surgery results in increased retinal oxygen saturation in the venules. Although the effects of the changes in the retinal blood flow are uncertain, the current results do indicate that an increased oxygen saturation results in a decreased oxygen extraction from the retinal circulation.