Long-term follow-up of patients with thyroid eye disease treated with endoscopic orbital decompression
Abstract
Purpose
To evaluate the outcome of endoscopic decompression in a series of patients with thyroid eye disease.
Methods
All 46 patients operated at our institution in the period 2001 to 2011 were invited for re-examination. Thirty-seven patients were included in the study and underwent a general otorhinolaryngological and ophthalmological examination. Nasal endoscopy, autoperimetry and a CT scan of the orbits and paranasal sinuses were performed. Preoperative and early postoperative data were obtained from hospital records. Re-examination was performed from 12 months to 9 years postoperatively. Paired t-test was used to evaluate the change in pre- and postoperative data. Image-guided surgery was used in two patients.
Results
Visual acuity improved from a median value (range) of 0.8 (0.05–1.25) to 1.0 (0.4–1.25) (p = 0.006). Intra-ocular pressure (IOP) was reduced from a median value (range) of 18 mmHg (10–27 mmHg) to 14 mmHg (8–24 mmHg) (p < 0.001). Median (range) Hertel values were 22.5 mm (14–29 mm) preoperatively and 19 mm (11–26 mm) postoperatively (p < 0.001). Mean reduction in proptosis was 4.0 mm. At follow-up, visual fields were normal in 16/37 patients (43%) and with small defects in 12/37 patients (32%). Seventeen patients (46%) had diplopia preoperatively in one or more directions of gaze while 9 (24%) suffered from constant diplopia. After endoscopic decompression, new onset diplopia was seen in seven (19%) individuals, while worsening of diplopia occurred in eight (22%). Impaired motility in abduction and/or elevation was seen in 20 (54%) individuals before decompression and in 23 (62%) after.
Strabismus surgery was performed in 22 patients. On final examination 85% of the study population were totally free of diplopia or experienced diplopia only in the peripheral field of gaze. Three patients developed sinusitis. Of these, endoscopic sinus surgery was performed in two patients, and one patient was conservatively treated. Symptoms resolved in all three patients.
Conclusion
Endoscopic medial orbital decompression including removal of the medial floor of the orbit is a safe and effective procedure for treatment of thyroid eye disease. Navigation can be of valuable help to ensure complete resection of the bony walls. However, the majority of patients will need subsequent strabismus surgery, mainly due to significant increase of esotropia.
Introduction
Decompression of the orbit can be achieved by removing one or several of the orbital walls or by reducing the amount of fat in the orbit. Lateral orbitotomy, developed by Kröhnlein in 1889, was first used for decompression in thyroid eye disease by Dollinger in 1911. Kennedy and co-workers first described endoscopic orbital decompression in 1990 (Kennedy et al. 1990). Since then, endoscopic technique has been widely used in both orbital and optic canal decompressions.
Vision threatening conditions such as optic neuropathy and severe proptosis with exposure keratitis are strong indications for orbital decompression. Decompression is also an option for treating disfiguring proptosis. After decompression, patients frequently experience less ocular discomfort and IOP is reduced.
The procedure to be used for orbital decompression will depend on the manifestations of the disease. Our current practice for patients with thyroid eye disease is to do lateral wall decompression for mild to moderate cases (Hertel values usually 23 mm or less) with no optic nerve involvement, endoscopic medial wall decompression for cases with optic neuropathy and combined endoscopic medial and lateral wall decompressions for more severe cases.
A number of reports have described the outcome of orbital decompressions (Leong et al. 2009; Mourits et al. 2009; Leong & White 2010). Most have focussed on the short-term recovery. There are relatively few reports on long-term outcome, also with respect to endoscopic surgery.
In this study, we have re-examined the patients who had been treated with endoscopic medial wall decompression in the period from 2001 to 2011. From 2011, image-guided navigation has been used in all patients, and we find that this is a helpful tool for peroperative control.
Materials and Methods
Patients
All 46 patients who underwent endoscopic orbital decompression at our institution between 2001 and 2011 were invited to participate in the study. Nine patients could not be enrolled; of these, two were deceased, two had emigrated, two were too old to be called, and three patients were unwilling to participate. The 37 patients who were included signed an informed letter of consent. The study was designated as a quality improvement study by the Regional Committee for Medical and Health Research Ethics, Western Norway, and approved as such by the hospital review board (ref. 2010/1893). The study adhered to the tenets of the Declaration of Helsinki.
Preoperative data and data from the immediate postoperative period were obtained from hospital records. At re-examination, the patients underwent a general ophthalmological and otorhinolaryngological examination. In addition, nasal endoscopy, automated perimetry (Oculus perimeter 900 Pro; Haag-Streit, Köniz, Switzerland, program G2 TOP) and a CT scan of the orbits and paranasal sinuses were performed.
Surgical technique
The procedure (Platt et al. 2008) was performed under general anaesthesia in all cases. In three cases, endoscopic septoplasty was performed before commencing orbital decompression due to obstruction of the middle meatus region by a deviated septum.
The standard endoscopic sinus surgery technique was used to expose the lamina papyracea and orbital floor (Fig. 1). A large antrostomy was created to provide access to the orbital floor. Sphenoethmoidectomy was performed and the whole lamina papyracea was exposed (skeletonized). The lamina papyracea was removed superiorly up to the skull base, posteriorly to the anterior wall of the sphenoid sinus and anteriorly to the maxillary line. Care was taken not to extend the maxillary sinus ostium anteriorly beyond the frontal process of maxilla to prevent injury to the nasolacrimal duct. A 30-degree endoscope was used to visualize the infraorbital nerve through the maxillary sinus ostium.
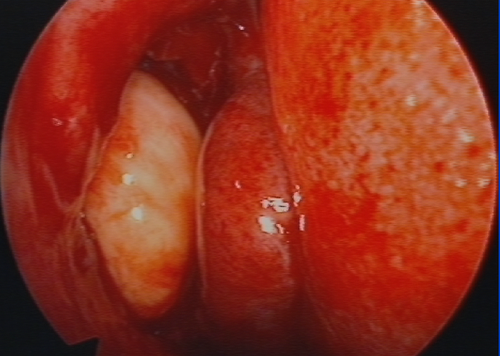
In 31/37 cases the medial portion of the floor of the orbit was removed by downfracturing the bone with a spoon curette. Nasal tamponade was used only in the three patients in whom septoplasty was performed prior to ethmoidectomy and orbital decompression. Incisions of periorbita were placed in a posterior- to- anterior direction. The posterior limit was the anterior wall of the sphenoid sinus.
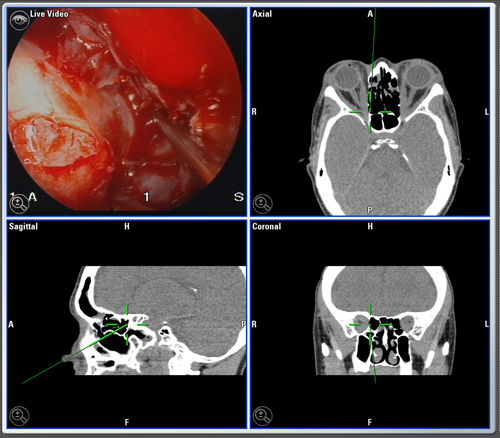
In two patients, the endoscopic surgery was performed with the aid of a Brainlab Kolibri navigation device (Brainlab, Feldkirchen, Germany) (Fig. 2).
Statistical analysis
The data were recorded in an Excel spreadsheet and analysed using the Statistical Package for the Social Sciences (spss Version 21.0; IBM Corporation, Armonk, NY, USA). Paired t-test was used to evaluate the change in pre- and postoperative data. Correlation coefficients were estimated using Spearman rank correlation test.
Results
The median age of the 37 patients who participated in the study was 52 years at surgery, range 23–70 years. 34 were females and three were males. The median follow-up time was 46 months, range 12–108 months.
All patients were euthyroid both at the time of decompression and at re-examination. Treatment of the thyroid disease consisted of only thyreostatic drugs in seven individuals, only radioactive iodine in five, thyreostatic drugs and radioactive iodine in 12, thyreostatic drugs and thyroidectomy in 10, and thyreostatic drugs, radioactive iodine and thyroidectomy in one. Two individuals were euthyroid and did not require any treatment for their thyroid disease.
Additional treatment of the orbitopathy consisted of systemic corticosteroids in nine, systemic corticosteroids and retrobulbar radiotherapy (2 × 10 Gy) in seven, lateral orbitotomy in seven, corticosteroids and lateral orbitotomy in six, and corticosteroids, retrobulbar radiotherapy and lateral orbitotomy in two. Six individuals did not receive any treatment of their orbitopathy before endoscopic decompression. In five and three patients, respectively, corticosteroids or retrobulbar irradiation was started or continued after the decompression. Three of the 15 individuals who underwent lateral orbitotomy did so after the endoscopic decompression.
A total of 66 endoscopic decompressions were carried out, 29 were operated bilaterally and eight were operated unilaterally. One patient was operated twice, one eye at a time. In six patients only the lamina papyracea was removed, while in the remaining patients also the orbital floor was excised. The extent of bone removal was examined by CT scans at follow-up. All patients had been operated posteriorly up to or a few mm anterior to the anterior wall of the sphenoid sinus. Anteriorly, the lamina papyracea had been removed up to the maxillary line.
Three patients developed delayed sinusitis postoperatively. Two were treated with endonasal endoscopic sinus surgery and one patient was managed conservatively. The CT scans did not reveal any additional cases with sinusitis. There were no cases with postoperative bleeding or infection, and we did not observe any CSF leaks. None of the patients had facial pain or signs of infraorbital numbness.
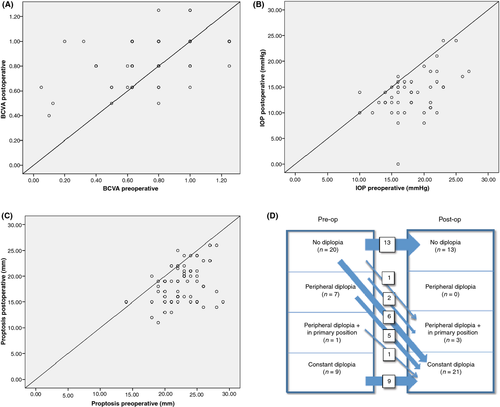
Prior to endoscopic decompression, signs of optic nerve involvement were present in 31 patients. Visual acuity below 0.5 was present in seven patients (eight eyes), and between 0.5 and 0.8 in 12 patients (17 eyes) (Table 1). At re-examination, visual acuity improved by more than one line in 14 eyes, remained unchanged in 48 eyes and worsened by more than one line in three eyes (Fig. 3A). Median value for best corrected visual acuity (BCVA) preoperatively was 0.8 (0.05–1.25), and at follow-up 1.0 (0.4–1.25). The difference is statistically significant (p = 0.006). There was no correlation between BCVA preoperatively and Hertel values or IOP preoperatively.
| Before first decompression | Before strabismus surgery | After strabismus surgery (last exam) | |
|---|---|---|---|
| Horizontal deviation | % (n = 37) | % (n = 36) | % (n = 35) |
| 0–10 PD eso | 79 | 44 | 86 |
| 10–19 PD eso | 12 | 17 | 11 |
| 20–30 PD eso | 6 | 8 | 3 |
| >30 PD eso | 3 | 31 | 0 |
| Vertical deviation | |||
| <5 PD | 74 | 58 | 83 |
| 5–10 PD | 6 | 22 | 14 |
| >10 PD | 20 | 20 | 3 |
| Motility | % (n = 22)a | % (n = 31) | |
| Normal | 5 | 65 | |
| Limited abduction | 27 | 3 | |
| Limited elevation | 13 | 13 | |
| Limited abduction and elevation | 55 | 19 | |
| Diplopia | % (n = 37) | % (n = 37) | % (n = 33) |
| No diplopia | 54 | 35 | 67 |
| Diplopia only peripherally (not in PP or reading position) | 19 | 0 | 18 |
| Diplopia peripherally + in PP | 3 | 8 | 3 |
| Diplopia peripherally + in reading position | 0 | 0 | 6 |
| Diplopia in all fields of gaze | 24 | 57 | 6 |
- PD = prism diopters; PP = primary position.
- a Data for those who underwent strabismus surgery.
Visual fields recorded at follow-up were normal [mean defect (MD) > −1.5] in 16 patients (43%) while smaller defects (−4 > MD > −1.5) were seen in 12 (32%) and larger defects (MD < −4) were seen in four (11%). We were unable to identify any common features for the four individuals with larger visual field defects.
Intra-ocular pressure above 21 mmHg was present in seven patients before the operation and in one patient postoperatively (Fig. 3B). Median (range) IOP decreased from 18 mmHg (10–27 mmHg) to 14 mmHg (8–24 mmHg) (p < 0.001). There was a weak correlation between IOP preoperatively and preoperative Hertel values (R2 = 0.12, p = 0.014).
Proptosis of more than 21 mm was seen in 30 individuals (52 eyes) preoperatively and in 13 (20 eyes) at re-examination (Fig. 3C). Median (range) Hertel value before the surgery was 22.5 mm (14–29 mm) and 19 mm (11–26 mm) after (p < 0.001). Mean reduction in proptosis was 4.0 mm. Minimal to low degree of papilledema [grade I-II (Frisén 1982)] which was seen in 11 patients preoperatively, resolved in all patients. Retrobulbar pain was present in 22 patients before the operation and in seven patients postoperatively.
Median value for lid aperture was 12 mm both preoperatively and at 6 months postoperatively. Lagophthalmos was seen preoperatively in 24% and postoperatively in 13%.
Seventeen patients (46%) had diplopia preoperatively in one or more directions of gaze while 9 (24%) suffered from constant diplopia. After endoscopic decompression, new onset diplopia was seen in seven (19%) individuals, while worsening of diplopia occurred in eight (22%) (Fig. 3D). Impaired motility in abduction and/or elevation was seen in 20 (54%) individuals before decompression and in 23 (62%) individuals after.
Due to manifest strabismus, restricted motility and diplopia, strabismus surgery was performed in 22 individuals after the decompression surgery. Twenty of these patients had their surgery performed in our hospital, whereas two were operated elsewhere. A total of 37 operations were performed on these 20 patients. Nine patients had only one operation, while 11 underwent more than one procedure. Twenty operations were done in topical anaesthesia with adjustable sutures, 11 had retrobulbar anaesthesia, while six of the patients had to be operated in general anaesthesia. In 16 of these 20 cases (80%), the surgery was performed on either the inferior rectus muscle, or the medial rectus muscle, or a combination of both. Follow-up data on 33 patients from the total study population (mean follow-up time 51 ± 35 months) show that 28 patients (85%) became either totally free of diplopia or experienced only diplopia in peripheral fields of gaze. Further details on strabismus and ocular motility are given in Table 1.
Discussion
Endoscopic orbital decompression is a well-established technique, but few long-term follow-up studies exist (Jernfors et al. 2007). Most previous studies are based only on hospital records or questionnaires. In the present study, we have re-examined 37 individuals treated with endoscopic orbital decompression. We confirm that improved visual acuity, reduced IOP, reduced proptosis and reduction in retrobulbar pain can be achieved. In the majority of patients, a stable situation was seen within the first 6 months after the operation. However, in some, additional treatment with retrobulbar irradiation or systemic corticosteroids was necessary.
Visual acuity remained unchanged or improved in most eyes (Table 1). However, at re-examination, visual acuity below 0.8 was still present in 14 eyes, and various degrees of visual field defects were seen in nearly half of the individuals examined. This indicates that thyroid eye disease can be a serious threat to visual function and that signs of optic nerve involvement may persist despite adequate decompression and anti-inflammatory treatment. It also underscores the importance of complete removal of bone in the posterior part of the orbit where there is little room for the optic nerve. In a review of previous series, Leong & White (2010) estimated that a mean difference of approximately 0.1 Snellen decimals was achieved after endoscopic decompression. Our results are thus within the range of other studies. Reduction in visual acuity by more than one line was seen in three individuals. Worsening of visual acuity after endoscopic decompression has also been reported by others (Neugebauer et al. 1996; Jernfors et al. 2007; Leong & White 2010).
Mean reduction in proptosis in the present series was 4.0 mm. Pooling data from several series, Leong & White (2010) found that mean reduction in proptosis following endoscopic decompression was 3.5 mm (SD = 0.51 mm). Although the reduction in proptosis that was achieved is above average, in more severe cases, endoscopic decompression must be combined with lateral wall removal to obtain sufficient reduction in proptosis.
A significant reduction in IOP was observed after decompression, and only one of seven individuals had IOP above 21 mmHg postoperatively. In thyroid eye disease, both decompression [(Norris et al. 2012) and references therein] and recession of the inferior rectus muscle (Gomi et al. 2007) may contribute to reduction in IOP. The most likely mechanism is a reduction in retrobulbar and episcleral venous pressure.
In previous series of endoscopic orbital decompressions, new onset or worsening of preexisting diplopia has been reported to occur anywhere from 15 to 45% of patients (Michel et al. 2001; Kasperbauer & Hinkley 2005; Malik et al. 2008; Platt et al. 2008). Balanced decompression (Graham et al. 2003; Kacker et al. 2003), preservation of an orbital sling (Metson & Samaha 2002), or the strut in cases where the floor is removed (Wright et al. 1999), have been advocated to reduce the risk of diplopia. Preservation of an orbital sling seems to be the most promising alternative (Metson & Samaha 2002; Jimenez-Chobillon & Lopez-Oliver 2010). Among the seven with new onset diplopia, three had been treated with decompressive lateral orbitotomy before endoscopic decompression indicating that combined medial and lateral decompression may not be the most efficient way of reducing diplopia postoperatively. Most of the patients in our series had signs of optic nerve involvement, and to achieve maximal decompression, preservation of an orbital sling or the strut was therefore not attempted (Swartz et al. 2011). The outcome after strabismus surgery was favourable, but as in other studies (Michel et al. 2001; Roberts et al. 2003), several procedures were often required.
Computer assisted image-guided systems were introduced in orbital surgery 20 years ago (Klimek et al. 1993) and have been used also in endoscopic decompression surgery (Camara et al. 2001; Dubin et al. 2008; Kent et al. 2010). We find it to be a helpful tool particularly when removing the bone close to the outlet of the optic canal. It still remains to be shown, however, that the use of image guidance improves outcome (Dubin et al. 2008).
Conclusions
The endoscopic procedure provides excellent visualization of key landmarks and allows complete medial wall removal and removal of the medial portion of the orbital floor with minimal risk of haemorrhage, visual impairment or infection. In thyroid eye disease, improved visual acuity and reduced proptosis and IOP is achieved together with reduction in retrobulbar pain. Patients must be informed about the risk for worsening or new onset of diplopia and the need for subsequent strabismus surgery.