Determining the optimal radiologic wrist and forearm position to visualize screw protrusion in scaphoid fixation
Abstract
Background
Surgical fixation of scaphoid fractures may result in unrecognized screw protrusion and subsequent cartilage damage to the adjacent joints. The purpose of this study was to use a three-dimensional (3D) scaphoid model to determine the wrist and forearm positioning that will allow intra-operative fluoroscopic visualization of screw protrusions.
Methods
Two 3D scaphoid models, with the wrist in neutral and 20° ulnar deviated, were reconstructed from a cadaveric wrist using the Mimics software. The scaphoid models were divided into three segments and further divided into four quadrants in each of the three segments along the scaphoid axes. Two virtual screws, with a 2 and 1 mm groove from the distal border, were placed so that the screws protrude from each quadrant. The wrist models were rotated along the long axis of the forearm and the angles at which the screw protrusions were visualized were recorded.
Results
One-millimetre screw protrusions were visualized at a narrower range of forearm rotation angles compared to 2 mm screw protrusions. One-millimetre screw protrusions in the middle dorsal ulnar quadrant could not be detected. Visualization of the screw protrusion in each quadrant varied with forearm and wrist positioning.
Conclusion
In this model, all screw protrusions, except 1 mm protrusions in the middle dorsal ulnar quadrant, were visualized with the forearm in pronation, supination or in the mid-pronation position and with the wrist in neutral or 20° ulnar deviated.
Introduction
The scaphoid bone is the most fractured carpal bone and is affected in 60% of all carpal bone fractures.1 Surgical fixation is recommended for displaced, non-united scaphoid fractures and unstable scaphoid fractures.2-4 Early surgical fixation of scaphoid fractures can lead to satisfactory functional recovery.5 However, undetected screw protrusions into the intercarpal or radiocarpal joint can cause cartilage wear and subsequently pain, requiring further surgery to remove metalware.6 Surgical fixation of scaphoid fractures is complicated by the complex three-dimensional (3D) structure of the scaphoid, making two-dimensional (2D) intraoperative fluoroscopic assessment of screw protrusion challenging, as a screw that has protruded beyond the scaphoid surface may appear to be appropriately located within the bone.7 The purpose of this study was to use a 3D scaphoid model to determine the wrist and forearm positioning that will allow intra-operative fluoroscopic visualization of screw protrusions in scaphoid fracture fixation.
Methods
A fresh-frozen cadaveric wrist of a 63-year-old female with a radiographically normal wrist was used for this study. Radio-opaque marker triads were implanted into the scaphoid, lunate, capitate, third metacarpal and radius of the cadaveric wrist. Computed tomography (CT) scanning of the cadaveric wrist was then performed and the resultant CT scan images were segmented using Mimics software (Materialize, Leuven, Belgium) to allow reconstruction of a 3D computer-generated wrist model.
To obtain an accurate neutral alignment of the wrist, a custom-built dynamic wrist simulator apparatus (DWSA)8 was utilized to actively move the wrist into its neutral position. The DWSA used in this study was calculated to demonstrate a level of accuracy with a root-mean-square error (RMSE) of less than 0.18° in both flexion-extension and radial-ulnar planes. Biplanar radiographs of the cadaveric wrist were then obtained using a custom biplane fluoroscopy setup with an inter-beam angle of 72°. Using an open-source software, XMALab,9 roentgen stereo-photogrammetry analysis (RSA) was performed to calculate the position of the radio-opaque markers embedded within the carpal bones. The CT scan data obtained was then calibrated by virtually re-arranging the volumetric model of the carpal bones according to the position of the markers, to create a 3D wrist model in neutral position based on the alignment of the third metacarpal and radius (Fig. 1a). A similar process was used to align the wrist at 20° of ulnar deviation to the long axis of the radius (Fig. 1b).
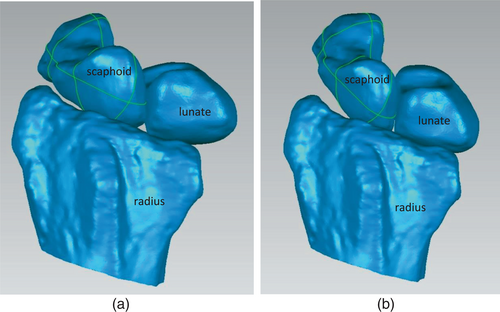
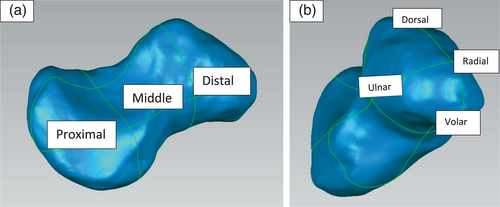
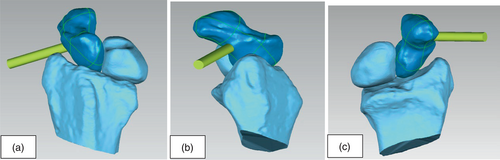
Based on the Mayo classification of scaphoid fractures,10 the volumetric model of the scaphoid was divided into three segments: distal, middle, and proximal, using Geomagic Studio software (3D Systems, South Carolina, USA) (Fig. 2a). The scaphoid axes were determined based on the moment of inertia11 and both the neutral positioned and ulnar deviated scaphoid models were then divided into 12 quadrants, which consisted of four quadrants in each of the distal, middle and proximal scaphoid segments, along the principal, secondary and tertiary scaphoid axes (Fig. 2b).
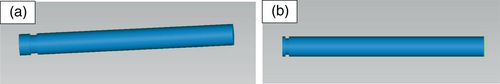
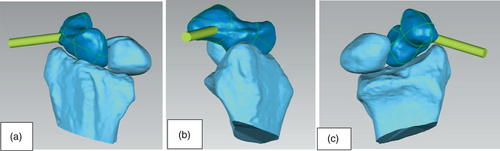
Two virtual screws were created – one with a groove 2 mm from its most distal border (Fig. 3a), and another, 1 mm from its most distal border (Fig. 3b). The two screws were then placed so that the screws protrude out of the 12 quadrants at 2 mm (Fig. 4a) or 1 mm (Fig. 4b) beyond the scaphoid cortex to simulate screw protrusions beyond the cortical surface of the scaphoid and are not representative of commonly used surgical techniques. Both the neutral positioned and ulnar deviated wrist models were then rotated along the long axis of the forearm, mimicking forearm pronation and supination and in the Billiard view position, with the forearm 45° pronated with ulnar deviation,12, 13 which is commonly performed during intraoperative fluoroscopic checking of screw position. The angles at which the screw protrusions were visualized were recorded by two assessors independently. In the event of a discrepancy in the angles measured, a third assessor was used.

Results
One-millimetre screw protrusions were visualized at a narrower range of forearm rotation angles compared with 2 mm screw protrusions. The range of forearm rotation that allowed visualization of the screw protrusion varied with the wrist in neutral or 20° ulnar deviated (Table 1).
| Quadrants | 2 mm | 1 mm | ||
|---|---|---|---|---|
| Neutral | Ulnar deviated | Neutral | Ulnar deviated | |
| Distal dorsal radial | 0–90, 120–180 | 0–180 | 0–70, 150–180 | 0–90, 140–180 |
| Distal dorsal ulnar | 30–150 | 70–160 | 60–140 | 100–150 |
| Distal volar radial | 0–60, 170–180 | 0–70, 170–180 | 0–40 170–180 | 0–50 170–180 |
| Distal volar ulnar | 50–140 | 60–140 | 70–130 | 90–140 |
| Middle dorsal radial | 80–160 | 50–140 | 70–120 | 60–130 |
| Middle dorsal ulnar | 150–170 | 0–40, 180 | NONE | NONE |
| Middle volar radial | 0–30 150–180 | 0–50, 150–180 | 0,150–180 | 0–30 160–180 |
| Middle volar ulnar | 70–130 | 50–130 | 110–120 | 90–110 |
| Proximal dorsal radial | 40–130 | 30–140 | 90–120 | 50–120 |
| Proximal dorsal ulnar | 0–80, 160–180 | 0–80, 170–180 | 0–60 160–180 | 10–60 180 |
| Proximal volar radial | 0, 110–180 | 0, 120–180 | 130–180 | 140–180 |
| Proximal volar ulnar | 0–60, 150–180 | 0–20 150–180 | 10–30, 160–180 | 0–10, 170–180 |
Distal segment
Screw protrusions in each quadrant of the distal segment of the scaphoid were visualized at a wider range of forearm rotation compared to similar quadrants in the middle or proximal segments. Screw protrusion in the distal radial quadrant was visualized in a greater range of forearm rotation with the wrist placed in 20° ulnar deviation than in the neutral position. However, screw protrusions in the distal ulnar quadrant were visualized in a greater range of forearm rotation with the wrist joint in a neutral position.
Middle segment
Two-millimetre screw protrusion in the middle dorsal ulnar quadrant of the scaphoid was detectable in the smallest range of forearm rotation compared to other quadrants. One-millimetre screw protrusion in this quadrant was not detectable in either neutral or ulnar deviated wrist models. Ulnar deviation of the wrist increased the range of forearm rotation in which screw penetrations in this segment could be detected.
Proximal segment
One and two-millimetre screw protrusions in the proximal dorsal radial quadrant could be visualized with the forearm in the mid-pronation position. Screw protrusion in other quadrants could all be visualized with the forearm in supination.
Discussion
Surgical fixation is indicated for acute displaced scaphoid waist or proximal pole fractures, chronic non-unions and unstable scaphoid fractures.1, 4 Though central placement of the screw is important biomechanically14 and clinically,15 malpositioning of the screw resulting in protrusion of the screw head can damage adjacent articular cartilage or soft tissue.16 Furthermore, central placement of screws might not always be possible.17 Guo et al. in 2014 showed that the central zones of the three scaphoid segments (proximal, waist and distal) are not continuous due to the irregular anatomy of the scaphoid bone and that it might not be possible to insert a screw that passes through the central zones of all three segments.18
Quan et al. in 2017 acknowledged the possibility of iatrogenic perforation of the scaphoid cortex especially if the screws appear close to the scaphoid cortex.7 We are not aware of any publications describing the thickness of the articular cartilage surrounding the scaphoid. However, assuming a similar thickness to the articular cartilage of the scaphoid fossa of 0.7 mm,19, 20 screw protrusion 1 mm beyond the cortical surface would be sufficient to cause damage to adjacent articular cartilage with carpal motion. The presence of screw penetration and prominence is best recognized intraoperatively with fluoroscopy so that the screw length or malpositioning can be corrected immediately. Screw protrusion can still occur despite intraoperative fluoroscopy.6 The unique shape of the scaphoid and the presence of adjacent bones make identification of screw protrusion difficult. The model used in this study showed that screw protrusions in different segments and quadrants can be recognized in different ranges of forearm rotation and whether the wrist is in neutral or ulnar deviated.
In this model, all screw protrusions, except 1 mm protrusions in the middle dorsal ulnar quadrant, were visualized with the forearm in pronation, supination or in the mid-pronation position and with the wrist in neutral or 20° ulnar deviated. One-millimetre screw protrusions in the middle dorsal ulnar quadrants were not detected as they were obscured by the concavity of the scaphoid waist (Figs 5 and 6). However, when screws are passed between the proximal and distal poles of the scaphoid, the site of protrusions in the middle segment are more likely to involve the volar quadrants rather than the dorsal quadrants due to the concave shape of the scaphoid in its sagittal plane. Hence, screw protrusions in the middle dorsal ulnar quadrants might not be clinically relevant except when using a scaphoid plate. Although screw placement from the standard starting point and longitudinal trajectory is common in scaphoid fracture fixation, several studies favoured fixations that were perpendicular to the fracture plane and recommended changing the screw starting point and trajectory to enable this. Kupperman et al. in 2018 and Faucher et al. in 2015 showed that perpendicular fixation of scaphoid fractures allowed the use of shorter screws and better fracture compression.21, 22 Therefore, screw protrusion within the middle segments is of increasing relevance as we deviate from the standard starting point and central placement of screws in scaphoid fracture fixation. Several studies have also recommended radiographic evaluation of the scaphoid using the Billiard view, with the forearm 45° pronated and wrist ulnar deviated.12, 13 In this study, the Billiard view position could not detect all screw protrusions.
Intra-operatively, radiographic evaluation of screw protrusion at the insertion sites, either proximal scaphoid, if a dorsal approach is used or distal scaphoid, if a palmar approach is used is unnecessary as screw protrusion at the insertion site of the headless compression screw (HCS) can be assessed by direct visualization. Fluoroscopic assessment is important for the evaluation of the distal end and shaft of the headless compression screw (HCS). The position of the screw and presence of screw penetration is generally evaluated with posteroanterior, lateral, and supinated and pronated oblique views or continuous fluoroscopy.23 However, ulnar deviation of the wrist will extend the scaphoid24 allowing better visualization of the waist and distal scaphoid in the posteroanterior view.
Detection of screw protrusion may commence initially by fluoroscopy of the scaphoid with a lateral and posteroanterior (PA) view to determining the quadrant of interest and the likely site of protrusion of the distal screw head. A PA view will determine whether it is placed radial or ulnar on the scaphoid and a lateral view will determine its dorsal or volar placement. That quadrant should then be evaluated fluoroscopically with the forearm in full pronation, mid-pronation and full supination and with the wrist in neutral and 20° ulnar deviated as our model demonstrated that all screw protrusions, except 1 mm screw protrusions in the middle dorsal ulnar quadrant, could be detected in these positions, without the need for continuous fluoroscopy.
The limitations of this study include the use of a single scaphoid model. As there are gender17 and racial25, 26 differences in size of the scaphoid and more than one kinematic pattern of scaphoid motion,27 the sample size required for a representative study and the variability of the angles measured are unlikely to produce results that will have a practical application. The use of screw trajectories for the computer visualization model which are not used in normal scaphoid compression screw fixation may limit the clinical usefulness of the measured angles in detecting screw prominence. Additionally, as only the radius, carpal scaphoid and lunate were retained in this 3D model, in clinical use, one or more other carpal bones including the radius and ulna might obscure visualization of the screw protrusion. Although scaphoid fractures are more common in young male patients and a cadaveric wrist specimen of a 63-year-old woman was used in this study, we are not aware of any evidence to suggest that the anatomy and carpal alignment, in wrists without injury or pathology, alters with age. Additionally, we have not validated these findings clinically using fluoroscopy.
The detection of screw protrusion is imperative intraoperatively so that its correction should prevent damage to the adjacent chondral surfaces that occur with carpal motion. The quadrant of interest is first identified, and fluoroscopic assessment for screw protrusion should be performed with the forearm in pronation, supination and in the mid-pronation position and with the wrist in neutral or 20° ulnar deviated positions.
Acknowledgements
Dr. Melanie Amarasooriya: Clinical fellow Victorian Hand Surgery Associates, Fitzroy 3065 Australia. Open access publishing facilitated by The University of Melbourne, as part of the Wiley - The University of Melbourne agreement via the Council of Australian University Librarians.
Author contributions
Melodi Yong: Conceptualization; data curation; formal analysis; investigation; methodology. Edward Liu: Data curation; investigation; writing – review and editing. Richard Tee: Methodology; writing – review and editing. Xin Zhang: Conceptualization; methodology; writing – review and editing. stephen tham: Conceptualization; investigation; methodology; project administration; supervision; visualization; writing – review and editing.
Conflict of interest
None declared.




