Modified iliotibial band tenodesis versus lateral extracapsular tenodesis, to augment anterior cruciate ligament reconstruction: a 2-year randomized controlled trial
Abstract
Background
Residual instability following anterior cruciate ligament (ACL) reconstruction is associated with disruption of the anterolateral complex (ALC). Our goal was to conduct a randomized controlled trial comparing the effectiveness of modified Iliotibial tenodesis (MITBT) versus lateral extracapsular tenodesis (LET) to correct this residual instability.
Methods
Group 1 underwent MITBT, Group 2 LET, added to the ACL reconstruction. Outcomes of interest were Tegner activity Scores (TAS), international knee documentation committee score (IKDC), knee osteoarthritis outcome score (KOOS), ACL related quality of life (ACL QoL), recurrent ACL rupture and meniscal tears. Follow-up was 2 years. Statistical analysis used chi-squared tests, frequency statistics and generalized linear models. We have followed the guidelines outlined in the CONSORT statement.
Results
A total of 164 patients were randomized, 84 to Group 1, 80 to Group 2. Group 1 had higher TAS than Group 2, at 2 years (median 8, range 7–10 vs. median 7, range 5–9, P<0.001). Group 1 had higher ACL QoL scores at 1 and 2 years post-surgery (82.1, SD2.7 vs. 67.9, SD 4.0, P< 0.001 and 82.5, SD 2.6 vs. 68.8, SD 3.8, P<0.001, respectively), and higher KOOS Sport/recreation subscale at both 1 and 2 years (91.5, SD4.3 vs. 78.3, SD7.9, P<0.001 and 91.8, SD4.8 vs. 80.4, SD 9.5, P<0.001). Risk of recurrent ACL rupture (0% vs. 5%, P = 0.040–0.05) and medial meniscal tear (2.4% vs. 14%, P = 0.007–0.02) were lower in Group 1.
Conclusion
Augmentation of ACL reconstruction with the MITBT, rather than the LET, was associated with improved outcomes, and lower risks of recurrent ACL rupture and medial meniscal tears.
Introduction
The pivot shift test used to diagnose anterolateral rotatory instability of the knee (ALRI) is the most clinically useful test for diagnosing anterior cruciate ligament (ACL) ruptures, is the result of damage to both the ACL and other stabilizing structures and correlates with the risk of recurrence and clinical outcome.1 Anatomic ACL reconstruction has been shown to correct even a severe pivot shift, when damage is primarily to the ACL.2, 3 However, some damage to the anterolateral soft tissues of the knee has been reported on MRIs in close to 90% of ACL ruptures.4 Significant damage to this anterolateral complex (ALC) of soft tissues may be responsible for the inability of ACL reconstruction to completely correct the pivot shift with inferior outcomes.5-7 A number of anterolateral soft tissue procedures have been used to correct this damage to the ALC, but the relative efficacy of the various techniques and the indications for their use remain uncertain.8 Both the lateral extracapsular tenodesis (LET) and the modified iliotibial band tenodesis (MITBT) have been shown to improve clinical outcome and reduce the risk of recurrence when combined with an ACL reconstruction, but there is no data comparing these techniques.9, 10 The goal of the current study was to compare the clinical outcomes and risk of recurrence, when either the LET, or the MITBT, was used to augment ACL reconstruction. Our null hypothesis was that there would be no difference in outcomes between these techniques.
Materials and methods
Patients presenting to the main author satisfying the inclusion criteria in Table 1, were invited to take part in the study. The baseline data are shown in Table 2.
| Inclusion criteria | Exclusion criteria |
|---|---|
| ACL rupture (diagnosed on MRI and at arthroscopy) | Other ligament injury greater than grade 1 or reparable meniscal tear |
| Skeletally mature | Previous ACL injury in either knee |
| Non-contact ACL injury | Unwilling to be randomized to either treatment group |
| Involved in twisting/pivoting sport | More than 6 weeks post ACL injury |
| ACL reconstruction performed within 6 weeks of injury | Not fit for general anaesthetic |
| Pivot shift at least one grade higher than contralateral knee on completion of the ACL reconstruction | Not willing to provide consent to take part in the study |
- ACL, anterior cruciate ligament.
| Group 1 (MITB) | Group 2 (LET) | P-value | |||
|---|---|---|---|---|---|
| Number | 84 | 80 | – | ||
| Male, number (%) | 39 (46.5) | 38 (47.5) | 0.51 | ||
| Mean | SD | Mean | SD | ||
| AGE (years) | 22.5 | 5.3 | 23 | 4.3 | 0.24 |
| BMI kg/m2 | 21.4 | 1.8 | 21.3 | 1.7 | 0.667 |
| PTS | 9.9 (median 10) | 1.3 (range 8–12) | 9.8 (median 10) | 1.4 (range 8–12) | 0.751 |
| Beighton score, 0–9 | 3.3 (median 3) | 1.0 (range 2–5) | 3.5 (median 3) | 1.2 (range 2–5) | 0.264 |
| TTS (days) | 17.7 | 9.3 | 18.9 | 9.9 | 0.413 |
| Operative limb dominance, n (%) | 40 (48%) | 39 (49%) | 0.92 | ||
| TAS pre-injury | 8 (median 8) | 0.9 (range7-10) | 8.4 (median 8) | 0.94 (range 7–10) | 0.13 |
| Graft diameter (mm) | 8.3 (median 8) | 1.2 (range 7–10) | 8.4 (median 7) | 1.1 (range 7–10) | 0.95 |
| Menisectomy, n (%) | 14 (17%) | 13 (16%) | 0.94 | ||
| Medial, n (%) | 7 (8%) | 5 (6%) | 0.6 | ||
| Lateral, n (%) | 7 (8%) | 8 (10%) | 0.71 | ||
| Meniscal repair, n (%) | 20 (24%) | 16 (20%) | 0.55 | ||
| Medial, n (%) | 6 (7%) | 6 (7%) | 0.93 | ||
| Lateral, n (%) | 14 (17%) | 10 (12%) | 0.45 | ||
- BMI, body mass index; CI, confidence intervals; PTS, posterior tibial slope; TAS, Tegner activity score; TTS, time to surgery.
Surgical procedure
The standardized pivot shift test was performed on both knees by the same surgeon with the patient under general anaesthesia, and graded as 0 (none), 1 (glide), 2 (clunk) or 3 (gross).11 The ACL reconstruction was then performed after which the pivot shift test was repeated. If the grade of the pivot shift was one or more grade greater than the contralateral knee, the patient was randomly allocated to Group 1 (to undergo the MITBT) or Group 2 (to undergo the LET). Randomization was performed using computer generated random numbers.
ACL reconstruction technique
The technique used has been shown to correct the pivot shift in cases of isolated ACL rupture, with both suspensory and screw fixation on the femoral side, and screw fixation on the tibial side.12 The screws used were made of poly-L-lactic acid-hydroxyapatite (PLLA-HA) material (BioRCI-HA; Smith & Nephew, MA, USA).
Group 1: MITBT procedure
This procedure was performed as described by Porter et al. (Fig. 1a).13 A 1 cm strip of the ITB is harvested, preserving its distal attachment, and passed from superficial to deep, around the proximal lateral collateral ligament before being passed into a bone tunnel deep to the ITB attachment on the tibia. This technique allows the tension in the looped graft is to be increased by pulling on the lead suture, adjusted until the grade of the shift is the same as that in the uninjured contra-lateral knee and secured in its tunnel with a third BioRCI-HA interference screw (Smith & Nephew, MA, USA) with the knee at 30° flexion and neutral rotation.
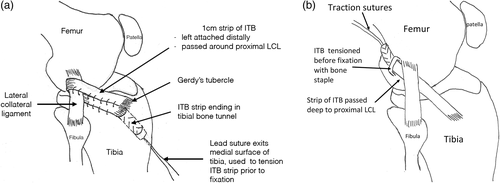
Group 2: LET
The LET is performed as described in the literature (Fig. 1b).9 The 1 cm strip of ITB is harvested in a similar manner to the MITBT, with a whip stitch attached to the end of the graft. The ITB graft is passed deep to the LCL and then fixed to the surface of the femur immediately anterior to the lateral intermuscular septum and proximal to the femoral attachment of the LCL using a Richards staple (Smith & Nephew, MA, USA). The graft is ‘hand tensioned’ before fixation with the knee at 60–70° knee flexion, and neutral rotation.
Post-operative protocol
Patients followed the same standard post-operative protocol. Weight bearing was permitted as tolerable immediately following surgery and a brace only used if a meniscal repair was performed. The early emphasis was on achieving full knee extension and quadriceps control, and range of motion was progressed as tolerable. Closed kinetic exercises were progressed as guided by pain, swelling and function, but no twisting or pivoting was permitted until 6 months post-surgery. Typically patients were using a stationary bike within 3–4 weeks of surgery, and running in straight lines at 3 months. Competitive pivoting sports were allowed at 9–12 months as long as the knee was symptom-free and the strength, balance, proprioception, jumping and landing techniques was similar on both sides.
Outcomes of interest
The study was granted approval by the hospital ethics committee, where the surgery was performed (Barton Private Hospital, ACT, Australia). The research is a registered randomized controlled trial (ACTRN12621000782831). There was no external funding for this research. The study has been performed in accordance with the ethical standards contained within the Declaration of Helsinki with preservation of patient anonymity.
Statistical analysis
Data entry was performed on Micosoft Excel and statistical analysis was performed using SPSS version 26.
The male: female ratios and operative limb dominance were compared using frequency statistics, cross-tabulations and chi-squared tests. PTS, Beighton scores and pre-injury TAS were assessed using both parametric and non-parametric approaches, while mean age, BMI and time to surgery (TTS) relied on analysis of variance (ANOVA). For meniscal tears treated at the time of surgery with partial menisectomy or meniscal repair, and the presence of GLL, the groups were compared using chi-squared tests.
The changes in TAS scores over time were compared using frequency statistics, cross-tabulation, parametric and non-parametric analysis. Changes in the KOOS total score and subscales, ACL related QoL and IKDC were compared using generalized linear models (GLMs) for repeated measures, and multivariate dependant GLMs for absolute change over the 2-year period, with Bonferroni adjustments to P-values.
The recurrence rate of ACL rupture, rate of contra-lateral ACL rupture, and rate of meniscal tears from aggregated findings were compared using chi-squared tests, with Yates correction for small cells numbers.
All statistical tests considered two-sided P-values <0.05 as significant.
Power analysis
Using data from published research,10 the minimum size of the study needed was 140 patients to detect a difference in total KOOS scores, and each subscale, with a minimal clinically detectable value of 10, IKDC (minimal detectable value of 5), TAS (minimal detectable value of 1), and ACL related quality of life (minimal detectable value of 10) with a power of 80% and a 5% risk of a type 1 statistical error. Recruitment was scheduled to discontinue when 10% more than the minimal number had been recruited.
Results
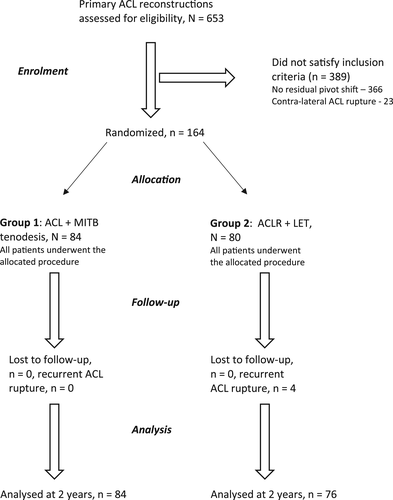
Between 1 July 2017 and 31 August 2019, out of 653 primary ACL reconstructions performed, 164 (25%) patients were enrolled in the study. No patient refused to take part in the study. Eighty-four were randomized to Group 1 (MITB) and 80 to Group 2 (LET). No patients were lost to follow-up and the data was analysed on an ‘intention-to-treat’ basis.
There were four recurrent ACL ruptures, all in Group 2, and the data for these patients were included in the analysis until recurrence.
Figure 2 is a patient flow chart, accounting for all patients enrolled in the study.
The results of the statistical analysis are detailed in Tables 2, 3 and 4 with P-values and 95% confidence intervals (CI) for normative data. Yates correction was used to adjust for the low cell number in Table 4.
| Group 1 | 95% CI | Group 2 | 95% CI | P-value | |||
|---|---|---|---|---|---|---|---|
| TAS | Mean | SD (range) | – | Mean | SD (range) | – | |
| TAS pre-injury | 8 (median 8) | 0.9 (7–10) | – | 8.4 (median 8) | 0.94 (range 7–10) | – | 0.134 |
| TAS 2 years | 8 (median 8) | 0.6 (6–10) | – | 7.3 (median 7) | 0.9 (range 5–9) | – | <0.001 |
| ACL QoL | |||||||
| baseline | 44.3 | 3.8 | 43.5–45.1 | 45.7 | 2.7 | 45.1–46.3 | 0.12 |
| 1 year | 82.1 | 2.7 | 81.5–82.7 | 67.9 | 4.0 | 67.0–68.8 | <0.001 |
| 2 years | 82.5 | 2.6 | 81.9–83.1 | 68.8 | 3.8 | 67.9–69.6 | <0.001 |
| KOOS 1 year | |||||||
| pain | 87.7 | 3.9 | 86.8–88.5 | 86.6 | 3.4 | 85.8–87.3 | 0.061 |
| symptoms | 67.2 | 5.9 | 65.9–68.5 | 69.0 | 6.6 | 67.5–70.5 | 0.069 |
| ADLs | 93.7 | 2.9 | 93.1–94.3 | 91.1 | 4.5 | 90.1–92.1 | <0.001 |
| sport/rec | 91.5 | 4.3 | 90.6–92.4 | 78.3 | 7.9 | 76.6–80.0 | <0.001 |
| QoL | 80.1 | 6.8 | 78.6–81.5 | 75.6 | 4.8 | 74.5–76.7 | <0.001 |
| total | 84.0 | 2.3 | 83.5–84.5 | 80.1 | 2.42 | 79.6–80.6 | <0.001 |
| KOOS 2 years | |||||||
| pain | 89.5 | 3.3 | 88.8–90.2 | 87.4 | 3.9 | 86.5–88.3 | 0.12 |
| symptoms | 70.5 | 6.2 | 69.2–71.8 | 72.3 | 5.3 | 71.1–73.5 | 0.09 |
| ADLs | 92.8 | 3.2 | 92.1–93.5 | 92.3 | 4.1 | 91.4–93.2 | 0.365 |
| Sport/rec | 91.8 | 4.8 | 90.7–92.8 | 80.4 | 9.5 | 78.3–82.5 | <0.001 |
| QoL | 81.9 | 7.0 | 80.4–83.4 | 75.8 | 4.6 | 74.8–76.8 | <0.001 |
| total | 85.1 | 2.4 | 84.6–85.6 | 81.7 | 2.8 | 81.1–82.3 | 0.002 |
- ACL QoL, ACL related quality of life; ADLs, activity of daily living; CI, confidence interval; KOOS, knee osteoarthritis outcome score; PRO, patient reported outcomes; Sport/rec, sport and recreation; TAS, Tegner activity score.
| Group 1 | Group 2 | P-value | Yates correction | |
|---|---|---|---|---|
| MM tear | 2 | 11 | 0.007 | 0.02 |
| LM tear | 1 | 2 | 0.53 | 0.53 |
| Recurrent ACL tear | 0 | 4 | 0.04 | 0.05 |
| Contra-lateral ACL tear | 3 | 2 | 0.69 | 0.95 |
- ACL, anterior cruciate ligament; LM, lateral meniscus;
Summary of statistical analysis outcome
The patient characteristics and baseline TAS and PROs were similar in the two groups.
TAS scores were higher and clinically relevant in the MITB group at 2 years post-surgery, P<0.001.
The ACL-related QoL was higher and clinically relevant in the MITB group at both 1 and 2 years post-surgery, P<0.001).
Of the KOOS scores, only Sport/Rec was higher and clinically relevant in the MITB group at 1 year (P<0.001), and at 2 years (<0.001).
Over the 2 year follow-up the risk of recurrent ACL tear was lower in the MITB group (P = 0.04), as was the risk of medial meniscal tear (P = 0.007). The risk of contra-lateral ACL tear (P = 0.95), and LM tear (P = 0.96) were similar in both groups.
There were no complications that required readmission to hospital or repeat surgery, other than those for recurrent ACL rupture or meniscal tear.
Discussion
This is the first randomized controlled trial (RCT) comparing the clinical outcomes following two different ALC augmentation techniques, combined with ACL reconstruction. It demonstrated that in comparison with the use of the LET, the addition of the MITBT to a knee with a residual pivot shift following ACL reconstruction resulted in clinically relevant higher TAS at 2 years following surgery, and patient-reported ACL QoL and KOOS Sport/Rec scores at both 1 and 2 years following surgery, with lower risk of recurrent ACL rupture and medial meniscal tear. Used in this manner the MITBT yielded superior outcomes and a lower risk of recurrence, and therefore we reject our null hypothesis.
Both the LET and the MITBT attempt to restore the role of the ALC. As described in the literature the LET uses ‘hand tensioning’ of the tenodesed ITB, fixed at 60–70° knee flexion.9 The final tension of the MITB is determined by the correction of the pivot shift, the most useful test for ALRI, and it is secured at 30° of knee flexion, the angle at which the pivot shift movements commences.3 The ability to adjust the tension of the tenodesis until the pivot shift is similar to that of the opposite knee, demonstrates the stabilizing role that the MITB is playing, and this may be responsible for its superior outcomes. The authors could have used similar end points for tensioning in both techniques but the goal of the study was to compare the two techniques as they have been described in literature.
The pivot shift is the manifestation of multiple factors, including damage to both the ACL (‘central’) and the ALC (‘peripheral’) structures and their relative contributions are likely to vary in vivo following ACL injury.6, 19 A residual pivot shift following ACL reconstruction has been shown to negatively correlate with clinical outcome and therefore we use failure of the ACL reconstruction to completely correct the pivot shift as the indication to add the MITBT. Our objective is to reduce the overall risk of ACL rupture, and over the 26-month period of our study 653 primary ACLs were performed by the same surgeon with 19 recurrences (4.4%). The incidence of contra-lateral ACL rupture in these patients was 4%. Akmese et al. used a similar surgical algorithm based on the pivot shift, with similarly low recurrence rate of less than 2% over a period of 2 years.20
The LET has also been shown to reduce rotatory laxity, but its use is described as protecting the ACL graft rather than correcting the pivot shift.9, 21 The large multi-centre, multi-surgeon, RCT performed by Getgood et al. has demonstrated that the LET, used to augment ACL reconstruction can reduce the rate of graft rupture and persistent rotatory laxity.21 Although the addition of the LET to ACL reconstruction resulted in a relative risk reduction of 0.38, the recurrence rates in their study were considerably higher than ours (25% in the ACLR + LET group, 40% in the ACLR group), which is consistent with the results of our study. We believe that the primary indication to perform an anterolateral augmentation procedure should be failure to correct the pivot shift to a grade similar to the contra-lateral uninjured side, rather than on presence of pre-determined risk factors. Using this algorithm results in an overall yearly risk of recurrence similar to the risk of a contra-lateral ACL rupture.
Na et al. performed a systematic literature review and concluded that ‘the general control of rotation and the protective effect on the graft’ is more important than the specific procedure used to augment the ACL reconstruction.22 Procedures reconstructing other components of the ALC, such as the ALL of the knee, have also been shown to be effective in improving control of the pivot shift.23 This may be the case even if the anterolateral procedure is added as second procedure in patients who present with persistent rotatory instability following previous ACL reconstruction whether perform anatomically,24 or a non-anatomically.25
There are a number of weakness in our study. All surgery was performed by a single, sub-specialized sports orthopaedic surgeon, which limits external validity but the study was adequately powered to compare the outcomes of interest, without introducing the potential confounding influences of different surgeons. There is a subjective component to the performance and interpretation of the pivot shift, but this was minimized by the same surgeon performing all pivot shift tests. The 2-year follow-up is relatively short, but the study is ongoing.
Conclusions
In the presence of a residual pivot shift following an anatomically positioned ACL reconstruction, augmentation with the MITBT results in better clinical outcomes, and a lower risk of recurrent ACL rupture or meniscal tears relative to augmentation with LET, at 2-year follow-up.
Conflict of interest
None declared.
Author contributions
Mark Porter: Conceptualization; data curation; formal analysis; investigation; methodology; writing – original draft; writing – review and editing. Bruce Shadbolt: Conceptualization; data curation; formal analysis; methodology; validation; writing – original draft; writing – review and editing.