Bariatric surgery in a public hospital: a 10-year experience
Abstract
Introduction
Obesity is common and adversely impacts quality-of-life and healthcare cost. In Australia, less than 10% of bariatric surgeries are performed in the public sector. This study reports our 10-year experience from a high volume public bariatric service which delivers multi-disciplinary care for primary and revisional procedures with mid- to long-term follow-up.
Methods
A prospectively maintained database of all patients who underwent bariatric surgery from January 2010 to January 2020 at a tertiary metropolitan hospital was analysed. We analysed patient demographics, comorbidities, perioperative outcomes, 2- and 5-year weight loss as well as comorbidities reduction.
Results
A total of 995 patients underwent 1086 (674 primary and 412 revisional) bariatric procedures with mean age of 46.9 years, mean BMI of 49.6 ± 9.1 kg/m2 and 92% patients with ≥1 obesity-related co-morbidity. Length-of-stay was longer for revisional than primary surgery (5.6 vs. 3.5 days). Major complication rate was 4.2%. Overall, % Total body weight loss (%TBWL) for primary surgeries at 2 years was 26.2%, and for revision surgery was 17.4%. At 2 years follow-up, treatment was ceased or reduced in 65% of diabetics, 29% of hypertensive patients and 69% of sleep apnoea patients.
Conclusion
This study confirms that bariatric surgery in Australia can be delivered effectively in resource constrained public health system with outcomes similar to private sector.
Introduction
Obesity incurs physical, psychological and metabolic health consequences. It increases mortality and healthcare cost. In 2019, over 70% of adults in Australia were overweight and over 30% obese.1 These rates are expected to reach 80% by 2025,2 with a bias towards morbid obesity.2, 3
Bariatric surgery results in sustained weight loss, improves obesity-related complications, especially for type 2 diabetes,4 and is cost-effective.5 Despite this, over 90% of all bariatric surgeries in Australia are performed in the private sector, with critically low access in the public health system.6-8 In 2019, The (National) Bariatric Surgery Registry (BSR) recorded 22 public hospitals performing bariatric surgeries but only 10 providing a significant volume (>75 cases/year).9 Therefore, a substantial proportion of patients who may benefit from surgery are unable to access it. As such it is imperative to increase access. However, the delivery of bariatric surgery is complex and requires co-ordinated multidisciplinary care. Resources available in the public health system are often constrained, raising concerns for the capacity of the public health sector to deliver the benefits of surgery successfully.
The outcomes of public bariatric surgery are important in determining its practicality, utility and challenges. Only five reports shed light on public bariatric surgery in Australia.10-13 The largest of these reflects experience predominantly with gastric banding,10 now much less used in bariatric practice, while two other series report a lesser volume of mixed surgery types with medium term follow-up.11, 12
This study advances on that literature reporting our 10-year experience at a high volume public bariatric service offering a full spectrum of primary and revisional procedures with mid to long term follow-up. We describe our service features noting temporal changes and resource constraints. Important observations are made with respect to demography, procedural utilization, outcomes, the burden of revisional surgery and implications for resource management and sustainability in the public sector.
Methods
Study design
Analysis of a prospectively maintained database was performed for consecutive patients who underwent gastric banding (GB), sleeve gastrectomy (SG) or roux-en-Y gastric bypass (RYGB), either as a primary or revisional procedure, from 1 January 2010 to 1 January 2020 at the Austin Hospital. This study and our registry received ethics approval from the Austin Health Human Research Ethics committee (H2012/04731).
Austin bariatric service
The Austin Hospital is a university-affiliated public hospital in Victoria, Australia. Bariatric surgeries are performed over two campuses: the main hospital for complex patients who may require intensive care support and the surgery centre (TSC) suitable for lower acuity patients. Patients are transferred from TSC to the main campus if escalation of care is required. Although our bariatric service has evolved overtime, the cornerstones have been multidisciplinary care, defined selection criteria and dedicated outpatient clinics. Before 2016, the indications for surgery were based on NIH guidelines.14 After 2016, the Edmonton Obesity Staging System, which predicts obesity-related mortality risk,15 was incorporated for patient selection. A structured referral form assists triage. Referred patients identified as eligible for surgery proceed through a group information session and a self-administered 8-week education program before proceeding to individual assessment. Such a process has been shown to improve outcomes.16 Patients deemed to have urgent conditions liable to decompensation may be expedited without the preclinic program. Our service is supported by nurse co-ordinators, dieticians and psychology services of the hospital. A medical weight loss program within the endocrinology department works co-operatively in the global management of bariatric patients.
Surgical management
Surgeries were performed by six surgeons, registrars and fellows. Surgical techniques for GB, SG and RYGB were similar between consultants. Surgical approach was surgeon dependent after assessment for reflux (avoid SG), metabolic burden (prefer RYGB), BMI and revisional surgery (prefer RYGB). Laparoscopic surgery was preferred. For SG, all surgeons used bougie sizes between 32 and 38 Fr and incorporated omentopexy. For RYGB, biliopancreatic and alimentary limb lengths varied between 60–120 cm and 80–100 cm, respectively. The choice of stapling devices, staple line reinforcement and haemostatic agents were at the surgeons' discretion. An enhanced recovery after surgery program was in place since 2016.
Data collection and definitions
Data were collected prospectively. We defined bariatric surgery as any operation for weight loss or treating its metabolic consequences. These may be primary or revisional (corrective, conversion or reversal) in nature. We defined legacy patients as those with an index operation performed prior to entering the Austin bariatric surgical service. For each new operation which altered the weight loss mechanism of the previous procedure, the revisional episode was considered a zero time point for follow-up purposes. Unless otherwise stated, all starting BMI and weight loss parameters were calculated from the maximum preoperative weight. Excess body weight (EBW) is defined as maximum weight minus ideal weight at a BMI of 25 for individual height. Percentage Excess Body Weight Loss (%EWL) is defined as weight lost as a fraction of EBW. Percentage Total Body Weight Loss (%TBWL) is defined as weight lost as a fraction of maximum body weight. Acute complication rates are reported for 30-day post-surgery. Severity of complications were graded by the Accordion score.17 A major complication was defined as an Accordion score ≥ 3.
Statistics analysis
Results are reported as mean (standard deviation) unless otherwise stated. Categorical variables were analysed using Chi-square test. Student's t-test or Mann Whitney's U-test were used to analyse continuous parametric and non-parametric variables respectively. Analysis of variance (ANOVA) was used to compare multiple groups. A two-tailed P < 0.05 was considered statistically significant.
Results
Patient characteristics
In total, 995 (Male: 200, female: 755) patients underwent 1086 bariatric procedures. Their mean (range) age was 46.9 (18–76) years. Over 60 nationalities were registered in our cohort (73% Australian born, 93% English speaking). 38% resided outside the Greater Melbourne Metropolitan region. The mean BMI of our cohort was 49.6 ± 9.1 kg/m2 (Males: 52.5 vs. Female: 48.9 kg/m2). The mean weight was 136.4 ± 29.9 kg. Obesity-related co-morbidities were seen in 915 (92%) patients, with 57% having ≥3 comorbidities (Table 1, Fig. 1).
| Comorbidity | Rate |
|---|---|
| Arthritis | 51% |
| Sleep apnoea | 49% |
| Hypertension | 49% |
| GORD | 44% |
| Asthma | 36% |
| Hypercholesterolemia | 32% |
| Diabetes | 27% |
| PCOS | 14% |
| Renal impairment | 1% |
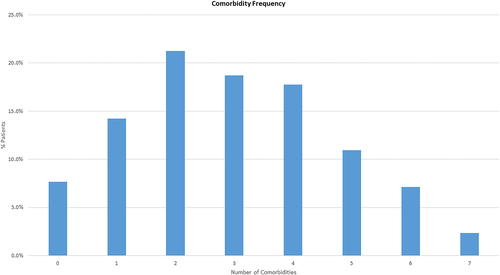
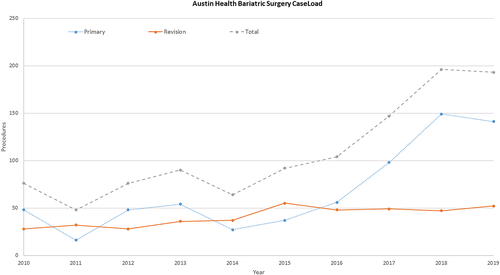
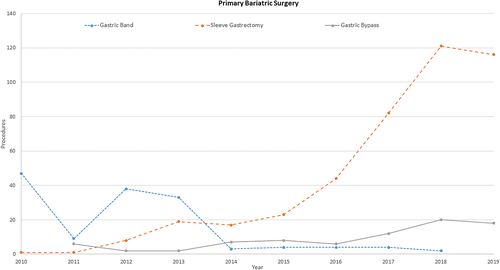
Surgeries
A 260% increase in caseload was seen over the audit period (Fig. 2), particularly since 2016, which coincided with expanded access to surgical beds at TSC. The majority of primary surgeries (674 cases, 62%) were SG (64%), RYGB (12%) and GB (21%). A small number (3%) of single anastomosis gastric bypass and intra-gastric balloon insertion were also performed. The change in predominant procedure type from GB to SG as primary procedures is highlighted in Fig. 3. A total of 412 (38%) revisional procedures were undertaken with their indications being complications of previous surgeries and/or poor weight loss. Of these, 77% came from legacy patients. The revision rate of primary surgeries performed at the Austin Hospital was 14% (94/674 patients). The majority of revisional procedures were GB reversals (27%), port revisions (26%), RYGB (25%), GB (11%), SG (3%) and vertical band gastric stapling reversal (3%), (5% miscellaneous). The most common primary operation requiring revision was GB (84%), followed by gastric stapling (7%), RYGB (5%) and SG (4%).
Length of stay
Table S1 describes the length-of-stay following GB, SG and RYGB. Overall, length-of-stay was significantly longer for revisional than primary surgery (5.6 ± 9.7 vs. 3.5 ± 1.8 days, P = 0.020). Perioperative HDU/ICU admission occurred in 8.2% of cases with a mean (SD) stay of 1.9 ± 1.4 days. Additionally, length-of-stay reduced over time. Comparing the time periods 2010–2014 to 2015–2019, length-of-stay reduced from 5.2 ± 2.1 to 3.5 ± 1.5 days (P < 0.010) following SG and from 6.5 ± 2.1 to 4.8 ± 1.4 (P = 0.010) following RYGB.
Complications
The overall complication rate in our cohort was 7.3% (Table 2), with a major complication rate of 4.2%. Of primary procedures, RYGB had the highest overall (11.1%) and major (4.9%) complication rate. Complications were also higher in revisional (10.9%) than primary (5.0%) surgeries (P < 0.001). This was observed across GB, GS and RYGB. SG as a revisional procedure had a particularly high complication rate (23% major, 31% overall) albeit small case numbers (n = 13). We classified (i) bleeding requiring endoscopic, operative or transfusion interventions, (ii) anastomotic or staple line leak, and (iii) 30-day mortality as key adverse events. No bleeding or leak occurred in GB. For primary procedures, rates of bleeding and leak were comparable between SG and RYGB (Bleeding 1.4% vs. 2.5%/Leak 0.5% vs. 2.5%). For revisional cases, rates of bleeding and leak were higher in SG compared with RYGB (Bleeding 7.7% vs. 2.0%/Leak 15.4% vs. 4.0%). However, due to low numbers this was not significant. One perioperative mortality was recorded in a revisional RYGB secondary to sepsis following a leak.
| Procedure | All complications | Major complications | ||||||
|---|---|---|---|---|---|---|---|---|
| Overall (%) | Primary (%) | Revision (%) | Primary versus revision P-value | Overall (%) | Primary (%) | Revision (%) | Primary versus revision P-value | |
| Gastric band | 4.7 | 2.8 | 10.6 | 0.030 | 3.7 | 1.4 | 10.6 | 0.003 |
| Sleeve gastrectomy | 5.6 | 4.9 | 30.8 | 0.001 | 2.9 | 2.3 | 23.1 | 0.001 |
| Gastric bypass | 19.2 | 11.1 | 25.7 | 0.010 | 9.9 | 4.9 | 13.9 | 0.040 |
| Port revision | 3.7 | NA | 3.7 | NA | 2.8 | NA | 2.8 | NA |
| Reversal gastric band | 2.7 | NA | 2.7 | NA | 1.8 | NA | 1.8 | NA |
| Reversal gastric stapling | 25.0 | NA | 25.0 | NA | 25.0 | NA | 25.0 | NA |
| Overall | 7.3 | 5.0 | 10.9 | 0.001 | 4.2 | 2.4 | 7.3 | 0.001 |
- NA, not applicable.
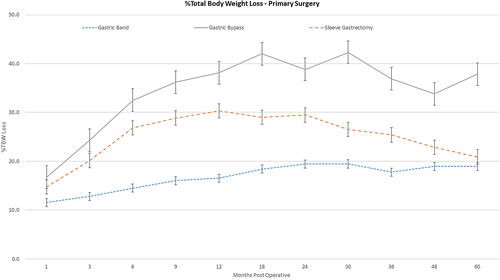
Weight loss after primary surgery
At 2 years follow-up, weight loss was significantly greater for RYGB and SG compared with GB (Table 3). At 5 years, this difference persisted for RYGB (P < 0.05) but was indifferent between SG and GB (Fig. 4). We noted that at 5 years, attendance by SG (50, 56%) patients were lower than GB (170, 71%).
| Procedure | 2 Years | 5 Years | ||||
|---|---|---|---|---|---|---|
| %EWL | %TBWL | Weight loss (kg) | %EWL | %TBWL | Weight loss (kg) | |
| Gastric band | 41.4 ± 22.2^ | 19.4 ± 10.5^ | 26.1 ± 16.3^ | 40.2 ± 28.0 | 18.9 ± 12.7 | 25.9 ± 18.9 |
| Sleeve gastrectomy | 58.8 ± 29.1# | 29.5 ± 12.8# | 43.1 ± 19.7# | 39.3 ± 29.1# | 20.9 ± 10.7# | 32.4 ± 20.3# |
| Gastric bypass | 80.1 ± 23.0* | 38.8 ± 10.1* | 55.6 ± 20.9* | 84.6 ± 24.9* | 39.4 ± 12.9* | 52.5 ± 23.4* |
| Overall | 53.9 ± 28.5 | 26.2 ± 13.3 | 37.1 ± 21.3 | 43.7 ± 29.0 | 21.1 ± 13.4 | 29.5 ± 20.8 |
- *P < 0.05 comparing RYGB versus GB, #P < 0.05 comparing RYGB versus SG, ^P < 0.05 comparing GB versus SG or RYGB.
- All data mean ± SD. 2 year: GB (n = 94), SG (n = 241), RYGB (n = 34), 5 year: GB (n = 92), SG (n = 27), RYGB (n = 11).
Weight loss after revisional surgery
At 2 years (47% follow-up), mean (SD) %TBWL was 17.4% (10.8%), 31.4% (13.5%) and 31.8% (12.0%) for revision to GB, SG and RYGB respectively. Meaningful data beyond 2 years was limited by small numbers.
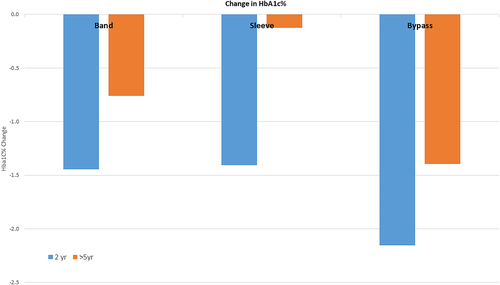
Diabetes
In total, 199 patients with diabetes underwent primary surgery. Of these preoperative insulin use was 27%. At 5 years (82.2% follow up), diabetic medication was ceased or reduced in 65.0% of patients. Concurrently, HbA1c fell from a preoperative mean (SD) of 7.8 ± 1.8% to 6.8 ± 1.4% (P < 0.001). Fall in HbA1C was greatest after RYGB than SG or GB (Fig. 5, Table S2). This was despite the RYGB group having greater preoperative disease reflected in insulin use (RYGB 29%, GB 23%, SG 17%) and HbA1c (RYGB 8.3%, GB: 7.8%, SG: 7.5%).
Hypertension and sleep apnoea
At 2 years, anti-hypertensive agents (74.3% follow-up) had ceased or reduced in 29% of patients, while CPAP use (72.2% follow-up) had ceased in 69% of patients. At 5 years, CPAP cessation (84.9% follow-up) was maintained at 68% but anti-hypertensive cessation (82.2% follow-up) had fallen to 18%.
Discussion
The benefits of bariatric surgery in treating obesity is well documented. Despite this, its availability within the Australia public hospital system is very limited. Based on 2019/2020 data from the BSR, only 6.2% of procedures were performed in a public hospital.7
There are likely to be substantial differences between public and private bariatric services. Previous studies suggest that public patients are larger and more comorbid than private patients.7, 10, 11, 13, 18 Socioeconomic, demographic, and motivational differences, as well as disparity in perioperative and outpatient resources, may also affect treatment efficacy. Given the stress on the (public) health dollar, it is important to establish the ongoing efficacy of bariatric surgery in the public system.
There are five studies examining the outcomes of public bariatric surgery in Australia.10-13, 18 These have all made valuable contributions historically to suggest efficacy of public bariatric surgery and encourage its establishment. Yet there are now gaps in published data due to evolution of bariatric practice involving more complex procedures. One from NSW reports an initial experience with a small (n = 65) pilot program and short follow up.12 Another reports low volume experience with GB,13 which has since been largely abandoned in that service. The same group has recently published their data on GB revision to RYGB, demonstrating feasibility and good early outcomes.18 Clough et al.11 described medium-term outcomes of 230 patients comparing GB, SG and RYGB, while the largest study by Burton et al.10 focussed predominantly on GB, now lesser used. Nonetheless, all these studies have demonstrated good outcomes and supports public bariatric surgery in Australia. Our study is important by being only the second report of a significant number of procedures (>1000) in an Australia public hospital with longer term follow-up, and describes a full spectrum of contemporary procedures including GB, SG, RYGB and revisional surgery demonstrating efficacy, safety and sustainability (10-year service).
Consistent with previous reports, our public patients are older, larger and more comorbid than private patient data in the BSR.7 Despite these differences, our safety outcomes for primary (major complication rate, Austin: 2.4% vs. BSR: 2.1%) and revisional (major complication rate, Austin: 7.3% vs. BSR: 9.3%) surgeries were comparable to national benchmarks.7
It is often feared that bariatric surgical patients require a disproportionate volume of inpatient resources. We have found this not to be the case. Mean length-of-stay for primary surgery was short (3.5 days) with only 8% admission into HDU/ICU for a mean of 1.9 days. This shortened significantly with institutional experience, formation of operative and perioperative teams, as well as care pathways. Currently, it is unusual that primary surgery patients stay longer than 2 nights (data not presented).
Our weight loss outcomes were comparable to national data at 2 years for all procedural type (7). However, while weight loss for RYGB and GB remained stable at 5 years, there was a curtailing for SG to 21% TBWL. The cause of this reduction is not clear. Follow-up rates in SG patients (53%) were significantly lower than for RYGB (72%) or GB (79%) and follow-up compliance has been previously demonstrated to affect outcome in bariatric surgical patients.19, 20 This phenomenon of SG patients being less likely to attend follow-up has been anecdotally reported and is now supported by our data. Reasons for this are unclear and worthy of further investigation. In any event, both the tendency to weight regain and the lower attendance rate is an interesting finding that may have some import when considering procedure choice for public bariatric surgical services.
Revisional surgery constituted 38% of the workload which is similar to that found for public surgery in the National Registry (36%) and is significantly higher than in the private sector (24%). Many patients having primary surgery in the private sector may be self-funded or use insurance only for the index surgery and not renew. For these patients, the cost of revisional surgery in private may be preclusive, thus placing disproportionate demand on the few public services available. This may divert resources away from treating new patients. In our own service, we were able to exponentially expand the number of primary procedures performed by creating protocols, including patient selection parameters,21 supported by the ANZMOSS National Bariatric Framework (21), thus allowing surgery to occur safely at our lower acuity surgical centre. This approach may have broad applicability in other centres. Nonetheless, revisional surgery is an inevitable part of managing obesity, as it is a chronic disease. Bariatric surgical units need to develop strategies to provide both primary and revisional needs. Appropriate triaging is crucial but challenging. In our service, revisional surgery is triaged in order of: life-threatening complications of previous surgery, complications causing significant symptoms, weight regain causing exacerbation of obesity-related comorbidities, and finally isolated weight regain.
Like other series, we found follow-up of patients difficult and this is a limitation of the study. Overall, 65% of ‘due’ review timepoints were attended by patients. This does not necessarily reflect simple patient noncompliance. Outpatient resources in the public system are constrained. Our service is limited to two half-day sessions per month and follow-up demand can outgrow this. Greater clerical and logistical support for patient tracking and recall would be beneficial. Funding for allied disciplines such as dietetics and psychology are departmentally based rather than service specific. Nonetheless, good outcomes have been attained and the service proven sustainable over 10 years. The nature of obesity as a chronic disease and the need for long-term multidisciplinary follow-up in bariatric surgery deserves special consideration when considering service planning and funding. Dedicated funding in this area would enhance service delivery and provide greater access to surgery. Indeed, recently the service has been able to secure purpose specific funding in these areas to enhance overall patient care. Moreover, establishment of more bariatric services across health care networks and networking between services would reduce the potential burden to a single service. Creative use of technology platforms could also be explored to enhance follow up for patients.
When considering optimal procedure choice in the public setting, important considerations include efficacy, durability, safety, follow-up burden and cost. While GB has been associated with the best safety profile for index surgery, follow up burden and revisional frequency have been concerns. Burton et al.10 described excellent results in a public bariatric service predominantly utilizing GB. In contrast, Clough et al.11 found outcomes with GB to be poor. Our data suggest GB is less effective than the other procedures with respect to weight loss and comorbidity impact at 2 years. At 5 years RYGB continues to be superior while SG and GB approximate. These lesser outcomes with GB may reflect differences in resources for follow-up with Burton et al. describing a service with up to two clinics per week compared with lesser availability in the series by Clough et al. and our own. These factors, as well as the improved safety profile and shortened hospital stay of resectional procedures have reduced the attractiveness of GB as an optimum procedure over resection in a public service. SG is attractive as it offers a better safety profile and less complexity than RYGB with lesser follow-up burden. Of concern however, our results suggest a tendency to weight regain at 5 years after SG. At this time point %TBWL remains equivalent to GB, but questions durability. Further investigation into improving this is warranted. This weight loss comparison however is to be interpreted cautiously. Sleeve follow up rates were significantly less than the other procedures – a weakness and limitation of such comparison – so true durability remains speculative.
Conclusions
Our study demonstrates medium to long-term outcomes of bariatric surgery in over 1000 procedures in a public hospital service with good outcomes. It confirms, along with previous studies that bariatric surgery in Australia can be delivered in public hospitals safely and efficaciously with similar outcomes to the private sector. The paucity of services nationally means that many patients currently are unable to access care yet could benefit greatly. It is imperative that provision of public bariatric surgery services be increased urgently and appropriate resourcing for follow-up care be supported.
Acknowledgement
We would like to thank Amanda Dalyell, Ian Michell, Kiron Bhatia and Chek H Tog for their contribution to this manuscript. Open access publishing facilitated by The University of Melbourne, as part of the Wiley - The University of Melbourne agreement via the Council of Australian University Librarians.
Conflict of interest
None declared.
Author contributions
Ahmad Aly: Conceptualization; formal analysis; investigation; methodology; project administration; supervision; visualization; writing – original draft; writing – review and editing. Calista Spiro: Conceptualization; data curation; formal analysis; investigation; writing – review and editing. David S. Liu: Data curation; formal analysis; methodology; visualization; writing – original draft; writing – review and editing. Krinal Mori: Conceptualization; formal analysis; methodology; writing – review and editing. Hou K. Lim: Conceptualization; data curation; formal analysis; methodology; writing – review and editing. Ruth Blackham: Conceptualization; investigation; methodology; writing – review and editing. Raymund J. Erese: Conceptualization; formal analysis; methodology; writing – review and editing.
Ethical approval
This study was approved by the Austin Health Human Research Ethic Committee. Individual patient consent was waived for this study.