Comparison of appendicectomy outcomes: acute surgical versus traditional pathway
Abstract
Introduction
The acute surgical unit (ASU) is an evolving novel concept introduced to address the challenge of maintaining key performance indicators (KPIs) in the face of an increasing acute workload.
Methods
The aim of this retrospective study was to compare the performance of the ASU (from June 2008 to December 2010) at Auckland City Hospital with the traditional model (from January 2006 to May 2008) and benchmark the results against other similar published studies. The analysis was on the basis of KPIs for 1857 appendicectomies, which form a large volume of acute surgical presentations.
Results
Our results show significant improvement in length of stay (2.8 days, 2.6 days, P = 0.0001) and proportion of daytime operations (59.4%, 65.8%, P = 0.004), in keeping with other studies on benchmarking.
Conclusion
The introduction of ASU has led to significant improvements in some KPIs for appendicectomy outcomes in the face of an increasing workload.
Introduction
The constantly increasing acute surgical workload has challenged traditional care delivery models. A range of new models have been developed including the introduction of acute surgical units (ASUs) that aim to focus resources in a timely way on patients admitted acutely.
In the traditional model, the on-call consultant would accept acutely admitted patients under their care and be on-call for emergency operating while engaged in regular elective commitments, including being offsite for clinics or operating lists.
The concept of the ASU was first introduced by the Prince of Wales Hospital, Sydney, in 2005,1 and has since been implemented at other hospitals across Australasia and worldwide.2-4 The ASU has been established at Auckland City Hospital (ACH) since June 2008.
The ASU is consultant-led model in the care of acute surgical patients that aims to optimize resources and improve key performance indicators (KPIs) by keeping the acute surgical workload independent of the elective workload.
The ASU model at ACH
ACH is a metropolitan, tertiary, teaching Hospital in Auckland, New Zealand. The Department of General Surgery at ACH has five sub-speciality teams: Head, Neck, Breast and Endocrine (five consultants), Upper Gastrointestinal (four consultants), Colorectal (four consultants), Trauma (three consultants) and the Acute Surgical Unit (three consultants).
The ASU model at our institution has previously been described by Hsee et al.5 In this model at ACH (Fig. 1), there is a dedicated acute surgeon who remains on site with no conflicting elective commitments (0730–1630), a dedicated team of junior staff (two registrars, one specialist nurse practitioner, one house officer) and a dedicated theatre and theatre staff for acute operating. There are two handovers (0730 and 1630) and two consultant-led ward rounds per day (0800 and 1400), where all ASU admissions and ward referrals are discussed and reviewed by the ASU consultant surgeon. After 1630 on weekdays and on weekends, the on-call consultant takes over responsibility for acute admissions and acute operating.
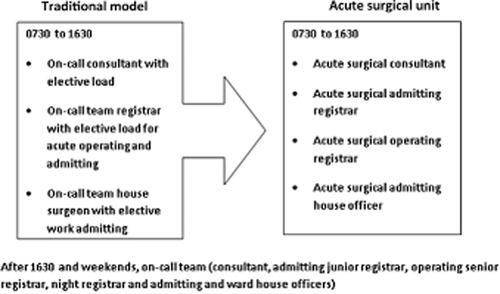
Paradigm shift in the care of acute surgical patients.
Key performance indicators
Surgeons and surgical units reflect on and compare performance using KPIs.6, 7 Previous comparisons of traditional and ASU models of surgical care have included comparison specific KPIs of length of stay (LOS), weekend discharge rates, time from referral to review, time to theatre (TTT) and proportion of daytime operations (Table 1).1-3
|
The aim of this study was to compare the performance of the ASU at ACH (from June 2008 to December 2010) with the historical model (from January 2006 to May 2008) and benchmark the results against other published studies. Appendicectomy is one of the most common acute general surgical procedures performed by the ASU and provided the volumes necessary to compare performance. In this study, the KPIs examined were LOS, TTT, operative duration, proportion of daytime operations, admission to consultation time, trainee as primary surgeon, 30-day re-admission rate, return to theatre and surgical complications.
Methods
Patient selection
A retrospective study was conducted, comparing patients who had appendicectomies acutely in the 29 months prior to and 31 months following the establishment of the ASU at ACH.
A dataset of 1982 patients who had an appendicectomy between 1 January 2006 and 31 December 2010 was acquired from the decision support team, clinical records department at ACH (Fig. 2). Prior to data acquisition, 125 entries were excluded as these entries were either duplicates or other elective procedures. Of the 1857 appendicectomies, 875 appendectomies were in the 29 months prior to the establishment of ASU (from January 2006 to May 2008) and 982 appendectomies in the 31 months following the inception of ASU (June 2008 to December 2010).
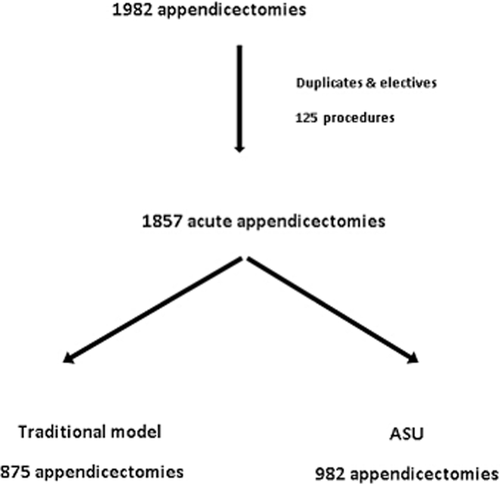
Dataset flow chart.
Sixty-five data points were retrospectively acquired by two independent data collectors according to clear pre-determined category definitions for each data point from patient discharge summaries, blood tests, scan results, operation notes, clinic letters and pathology reports.
Definitions
Length of stay was defined as the duration from time of admission to time of discharge. Time to theatre was the duration from time of theatre booking request to start time of appendicectomy. The Clavien–Dindo system8 was referred to for the classification of complications. Surgical complications analysed were wound infection, intra-abdominal collections and death. Wound infection was defined as any infection of the wound that required antibiotics or surgical management within 30 days of surgery. Return to theatre and re-admission was defined as being within 30 days of the initial procedure. Perforated appendix was taken as pathology report finding of appendicitis with perforation. Diagnostic accuracy was measured as the proportion of appendicectomy specimens that had appendicitis on pathological reporting. The American Society of Anaesthesiologist (ASA) Physical Status Classification System9 entry was included as the objective marker of preoperative co-morbid status. Pathology of the appendix was classified as suppurative, gangrenous, perforated and other (carcinoid, worm, other tumours, lymphoid hyperplasia).
Calculations
All cases of acute appendicitis presenting to ACH in the 29 months prior to and the 31 months after the establishment of the ASU were compared on the basis of KPIs.
Data were analysed using two sample t-test, two proportion t-test, chi-squared test and Mann–Whitney U-test. Statistical analysis was performed in Analyse-it (Microsoft, Redmond, WA, USA) and XL-STAT (Addinsoft, New York, NY, USA), and a P-value of <0.05 was considered statistically significant.
Results
One thousand and fifty-seven patients who underwent appendicectomy were admitted during the study period, with a 12% increase in the post-ASU era.
The two groups were comparable in their demographics (Table 2), with no significant differences with respect to age, gender ratio, ASA and the rate of perforated appendicitis.
| Traditional care pathway (n = 875) | Acute surgical pathway (n = 982) | P-value | |
|---|---|---|---|
| Median age in years (range) | 28.7 (15–100.0) | 27.9 (14.7–88.1) | 0.272 |
| Gender (M : F) | 483:392 | 530:452 | 0.608 |
| ASA ≥ 2 | 27.5% (n = 241) | 25.9% (n = 254) | 0.391 |
| Perforated appendicitis | 11.8% (n = 103) | 13.4% (n = 132) | 0.295 |
| Median time to theatre (h) | 8.2 (0.4–59.6) | 7.5 (0.4–65.1) | 0.775 |
| Duration of operation (min) | 59.0 (18.0–182.0) | 57.0 (6.0–230.0) | 0.139 |
| Proportion daytime operations | 59.4% (n = 520) | 65.8% (n = 646) | 0.004 |
| Mean admission to consultation time (h) | Not available | 2.82 ± 2.72 (n = 626) | — |
| Trainee as primary surgeon | 95.9% (n = 839) | 97.0% (n = 953) | 0.219 |
| Total length of stay (days) | 2.8 (0.7–35.8) | 2.6 (0.8–23.6) | 0.0001 |
| Return to theatre | 1.3% (n = 11) | 1.1% (n = 11) | 0.786 |
| 30-day readmission rate | 5.3% (n = 46) | 6.0% (n = 59) | 0.48 |
| Surgical complications | 7.4% (n = 65) | 6.3% (n = 62) | 0.297 |
| Wound complications | 4.0% (n = 35) | 2.6% (n = 26) | 0.103 |
| Intra-abdominal collection | 3.4% (n = 30) | 3.6% (n = 35) | — |
| Death | 0 | 0.10% (n = 1) | — |
- ASA, American Society of Anaesthesiologist.
The rate of laparoscopic appendicectomy (79.0% (n = 691) versus 87.9% (n = 863); P < 0.0001) and preoperative imaging (24.2% (n = 212) versus 37.1% (n = 364); P < 0.0001) has significantly increased. However, 31.4% (188/598) of scans did not identify the appendix and those who had scans preoperatively had a longer mean preoperative LOS (0.79 ± 0.53 days versus 1.40 ± 0.82 days; p = 0.000). The clinical operative diagnostic accuracy was 78.0% (n = 1448).
Table 2 compares the KPIs for the traditional model with those for the ASU model. There was a significant reduction in the LOS and the proportion of daytime operations. Although there were trends towards improvement in most of the other KPIs, these differences were not statistically significant. There was one death in a co-morbid elderly patient who had severe sepsis at the time of presentation.
Discussion
There has been a 12% increase in appendicectomies since ASU was formed and a 15.7% increase in the catchment population of ACH (404 619–468 000).10, 11 Studies from other centres have also shown an increase in appendicectomy workload.1, 2 The KPIs in our study have remained the same or improved despite there being no increase in the radiological, theatre or bed resources for this 12% increase.
Until 1981, when Semm performed the first laparoscopic appendicectomy,12 open appendicectomy remained the gold standard. Since then, several randomized control trials and meta-analyses have shown advantages to laparoscopic appendicectomy with less post-operative pain and wound infections and shorter recovery times,13, 14 resulting in a worldwide trend towards an increase in the popularity of laparoscopic appendicectomy,15, 16 similar to that seen in our study and the study by Gandy et al.1
The role of preoperative imaging in appendicitis is still debated. There are studies that show a decrease in the rate of perforation and negative appendicectomy17, 18 and others studies that show no significant differences in outcome and increase in the TTT19-22 as a result of preoperative scanning. In addition to confirming the increase in the preoperative LOS for those patients who have preoperative imaging, our study shows that the rate of detection of the appendix on preoperative scans (68.6%) was lower than the clinical operative diagnostic accuracy (78.0%, n = 1448). The findings of our study do not support the routine use of scans for the diagnosis of appendicitis. There may be a subgroup of patients with atypical presentations for suspected appendicitis in whom preoperative scanning may be useful.23 This study was not designed to investigate the role of radiological investigations in appendicitis and this topic is the focus of further study.
Acute surgical units are considered the future of emergency surgery.24, 25 There are a number of postulated benefits to an ASU model over the traditional model, not all of which can be measured. KPIs are a means to quantify the outcomes of ASU when compared with the traditional model.3 Our study has shown significant improvements in the LOS and proportion of daytime operations. The implication of these improvements in the efficiency of provision of care for appendicectomy patients are as follows: treatment when there is more expertise available during the daylight hours and shorter hospital stays. The decrease in the LOS also provides a direct cost saving to the establishment.
This study is a retrospective, single institution study and has the limitations associated with such a study design. We were unable to study the admission to consultation time as the records for this parameter were not available prior to June 2008. The benefits to training could not be assessed as data regarding the degree of supervision could not be ascertained from the database. It is inherent to the consultant-led ASU model that there is an increase in supervised training and other studies have demonstrated an improvement in training opportunities.3
As the concept of acute care surgery is relatively novel, there are few studies comparing the traditional model with the acute care model.1-3, 26, 27 KPIs have been identified as valuable in the evaluation of performance of ASU.28 However, there is no established standardized approach to the comparison of outcomes following the introduction of an acute surgical model.1 Table 3 is a comparison of the findings of our study with the two similar benchmark studies by Gandy et al.1 and Earley et al.26
| Difference in parameters (ASU minus traditional model) | Our study (NZ) n = 1857 | Gandy et al.1(Australia) n = 402 | Earley et al.26 (USA) n = 294 |
|---|---|---|---|
| Study population (traditional : ASU) | 875:982 | 176:226 | 127:167 |
| Length of stay (days) | −0.2 days (P = 0.0001) | +1 day (NS) | −1.2 (P < 0.001) |
| Proportion daytime operations (%) | +6.4% (P = 0.004) | +13.7% (P = 0.006) | +15% (NS) |
| Surgical complication rate difference (%) | −1.1% (NS) | −4.5 (NS) | −9.7% (P < 0.05) |
| Return to theatre (%) | −0.2% (NS) | — | — |
| Readmission (%) | +0.7 (NS) | −1.96% (NS) | — |
| Time to theatre (h) | −0.7% (NS) | −0.85 (NS) | −4.1 (P < 0.05) |
| Admission to consultation time (h) | — | — | +0.2 (NS) |
| Trainee as primary surgeon (%) | +1.1 (NS) | −2.3% (NS) | +40% (P < 0.05) |
| Duration of operation (min) | −2.0 (NS) | — | — |
- ASA, American Society of Anaesthesiologist; NS, no significant change.
All three studies similarly show improvements in LOS, proportion of daytime operating and with trends towards improvements in other KPIs. The differences between groups are smaller in our study compared with the two previous studies. This may be due to small study effects with the smaller population studies. For some KPIs, there was less scope for improvement given the already favourable baseline parameters in the traditional model at our institution (our study, Gandy et al.,1 Earley et al.26): surgical complications (7.4%, 8.5% and 17.4%), TTT (8.2, 10.5 and 7.6 h) and trainee first operator (95.9%, 68.2% and 30%).
Our study is one of the larger studies comparing ASU and traditional care pathways for appendicectomy outcomes across a wider range of KPIs.
Conclusion
The introduction of ASU to ACH has resulted in a significant improvement in the LOS and proportion of daytime operations for appendicectomy patients. Improvements in other KPIs may be possible with a more detailed analysis of the contributory factors to each KPI.
Acknowledgements
The authors wish to thank Rosemary Pearson, PMP, MHRINZ, MA, acute surgical pathway improvement manager, and Marissa Gordon, data analyst, for their assistance and contribution to statistical analysis and acquisition of the dataset, respectively.




