J point elevation in high precordial leads associated with risk of ventricular fibrillation
Abstract
Introduction
The significance of high precordial electrocardiograms in idiopathic ventricular fibrillation (IVF) is unknown.
Method
This study included 50 consecutive patients (48 men; age, 42 ± 18 years) who had spontaneous ventricular fibrillation not linked to structural heart disease and received implantable cardiac defibrillator therapy. IVF was diagnosed in 35 patients and Brugada syndrome was diagnosed in other 15 patients. Electrocardiograms in high intercostal space were compared between 35 patients with IVF and 105 age- and sex-matched healthy controls (patient: control ratio, 1:3).
Results
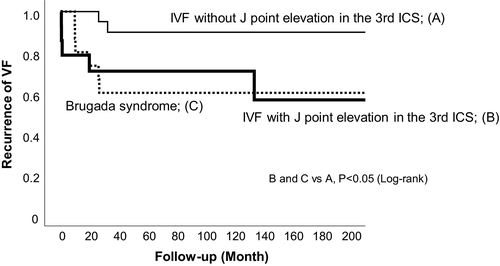
The frequency of J point elevation ≥ 0.1 mV in the 4th intercostal spaces was similar between patients with IVF (14%) and healthy controls (7%). However, the frequency of J point elevation ≥ 0.1 mV in the 3rd intercostal space was higher in patients with IVF (40%) than controls (11%) (p < .01). J point elevation was present only in the 3rd intercostal space but not in the 4th intercostal space in 30% of patients with IVF but only in 6% of controls (p < .01). During follow-up, the recurrence of ventricular fibrillation was higher in patients with IVF who had J point elevation in the 3rd intercostal space (36%) and Brugada syndrome(40%) than those with IVF who did not have J point elevation in the 3rd intercostal space(11%) (p < .05 for both).
Conclusion
J point elevation in the 3rd intercostal space was associated with IVF and recurrences of ventricular fibrillation. Electrocardiogram recordings in the high intercostal space may be useful to identify risk of sudden death.
1 INTRODUCTION
Ventricular fibrillation (VF) is usually associated with structural heart disease. (Huikuri et al., 2001) However, VF also occurs in patients without structural heart disease. (Conte et al., 2017; Waldmann et al., 2018) Early repolarization pattern or J point elevation in the inferior and/or lateral leads of the 12-lead electrocardiogram (ECG) is associated with pathogenesis in idiopathic ventricular fibrillation (IVF). (Haissaguerre et al., 2008; Rosso et al., 2008; Tikkanen et al., 2009) Furthermore, J point elevation in the right precordial leads is also associated with IVF. (Antzelevitch & Yan, 2010).
Brugada syndrome (BrS) is also characterized by J point elevation in the right precordial leads and is associated with risk of ventricular fibrillation. (Brugada & Brugada, 1992) The characteristic ECG pattern is often found only in the right precordial leads placed at second and/or third intercostal spaces (ICS) in BrS. (Savastano et al., 2014) However, the significance of high precordial ECGs is unknown in IVF. In this study, we compared high right precordial ECGs between patients with idiopathic ventricular fibrillation and healthy controls. We also studied the association of J point elevation in high precordial ECGs with risk of VF recurrences.
2 METHODS
2.1 Study population
We enrolled 50 consecutive patients, between 2003 and 2018, who were referred to our institution for resuscitated VF not linked to structural heart disease. IVF was diagnosed in 35 patients and BrS was diagnosed in other 15 patients. During hospitalization, all patients received implantable cardioverter-defibrillator (ICD) therapy. Patients with structural heart disease were excluded using 12-lead ECGs, transthoracic echocardiography, cardiac computed tomography, cardiac magnetic resonance imaging, coronary arteriography including spasm induction, and left ventriculography. Patients with long QT syndrome, short QT syndrome, and catecholamine-induced polymorphic ventricular tachycardia were also excluded. Institutional review board approval was obtained.
All patients without spontaneous type 1 Brugada ECGs received sodium channel blocker test. BrS was diagnosed when type 1 ST-segment elevation was observed either spontaneously or during sodium channel blocker test in at least one right precordial lead (V1 and V2), which was placed in a baseline standard or high (second or third) ICS. (Priori et al., 2015).
Twelve-lead ECGs recorded in the absence of antiarrhythmic drugs were compared between patients with IVF and control subjects who were matched to patients based on gender and age (patient: control ratio, 1:3). Control subjects without cardiovascular disease or medication use were included. Subjects with bundle branch block, intraventricular conduction disturbances, and/or abnormal QT intervals in ECGs were excluded.
2.2 ECG analysis
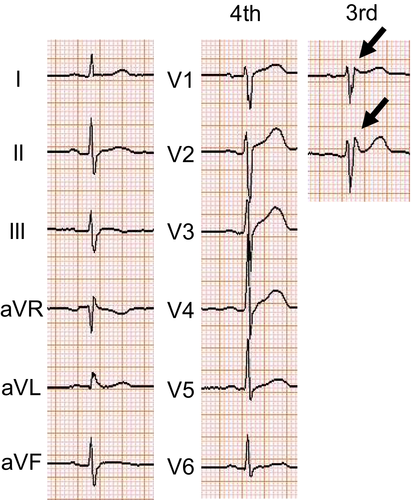
We evaluated ECGs recorded in the 3rd and 4th ICSs in the absence of antiarrhythmic drugs during sinus rhythm in all study subjects. J point elevation in the right precordial leads was defined as upward/downward notching or downward slurring with an amplitude ≥ 0.1 mV at the end of QRS to early ST segment in any of the right precordial leads (V1 and V2) in the 3rd or 4th ICS (Figure 1). Inferolateral early repolarization (ER) was defined as the presence of a positive J wave, which is a slurring or notch at the QRS terminal that is ≥ 0.1 mV above the isoelectric line in ≥ 2 contiguous leads in any of the inferior leads (II, III, and aVF), the lateral leads (I, aVL, and V4–V6), or both. (Haissaguerre et al., 2008) All ECGs were manually evaluated separately by two independent cardiologists who were blinded to the patient status (VF patients or healthy controls).
2.3 Clinical data
The medical records of all VF patients were investigated for age at VF development, sex, family history of sudden death at ≤ 45 years, patient's activity at the onset of VF, and medications. Activity status at the onset of VF was classified as sleep if VF occurred during sleeping, arousal at rest if VF occurred when the patient was awake without body movement, or physical effort if VF occurred during exertion. Electrophysiologic studies were performed on 27 patients.
After ICD implantation, all patients visited the outpatient clinic every 3–6 months for ICD interrogation. During the follow-up, patients were considered to have VF recurrence if VF was documented by ICD interrogation. An electrical storm was defined as three or more VF events recorded within 24 hr. The beginning of the observation period was the day of ICD implantation. ECGs were recorded in the 3rd and 4th ICSs at clinic visits; however, none of the patients diagnosed with IVF showed type 1 Brugada ECGs during the follow-up.
2.4 Data analysis
The statistical analyses were performed with SPSS version 25 (IBM Inc., Armonk, NY). Data were expressed as the mean ± SD or number (percentage). Differences in parameters between patients with IVF and control subjects were analyzed using Student's t test for continuous variables and by the Fisher's exact test for categorical variables. Survival curves were constructed by the Kaplan–Meier method and were compared using the log-rank test. A two-sided p < .05 was considered statistically significant.
3 RESULTS
3.1 Comparisons between patients with IVF and healthy controls
The clinical and ECG characteristics in 35 patients with IVF and 105 age- and sex-matched controls are shown in Table 1. Patients with IVF included 33 men (94%), and the mean age was 42 ± 18 years. The control group included 105 healthy individuals who were matched to patients with IVF based on sex and age (patient:control ratio, 1:3). The frequency of J point elevations ≥ 0.1 mV in the 4th ICS was similar between patients with IVF (14%) and healthy controls (7%) (p = .17). However, the frequency of J point elevation ≥ 0.1 mV in the 3rd ICS was higher in patients with IVF (40%) than controls (11%) (Odds ratio [OR], 5.2; 95% confidence interval [CI], 2.1–12.8; p < .01). Furthermore, the frequency of J point elevation ≥ 0.2 mV in the 3rd ICS was higher in patients with IVF (26%) than controls (3%) (OR, 11.7; 95% CI, 3.0–46.6; p < .01). J point elevation was present only in the 3rd ICS but not in the 4th ICS in 30% of patients with IVF and only in 7% of controls (p < .01). The frequency of inferolateral early repolarization and the other ECG parameters were not different between the two groups.
| IVF (N = 35) | Control (N = 105) | P-value | |
|---|---|---|---|
| Male sex, N (%) | 33 (94%) | 99 (94%) | - |
| Age, years | 42 ± 18 | 42 ± 18 | - |
| J point elevation in right precordial leads | |||
| in the 4th ICS, N (%) | |||
| ≥0.1mV | 5 (14%) | 7 (7%) | 0.17 |
| ≥0.2mV | 3 (9%) | 2 (2%) | 0.10 |
| in the 3rd ICS, N (%) | |||
| ≥0.1mV | 14 (40%) | 12 (11%) | <0.01 |
| ≥0.2mV | 9 (26%) | 3 (3%) | <0.01 |
| J point elevation only in the 3rd ICS but not in the 4th ICS, N (%) | |||
| ≥0.1mV | 9/30 (30%) | 6/98 (6%) | <0.01 |
| ≥0.2mV | 4/30 (13%) | 2/98 (2%) | 0.03 |
| ER pattern in inferior leads, N (%) | 5 (14%) | 7 (7%) | 0.17 |
| ER pattern in lateral leads, N (%) | 2 (6%) | 3 (3%) | 0.60 |
| ER pattern in inferolateral leads, N (%) | 1 (3%) | 1 (%) | 0.44 |
| ECG parameters | |||
| Heart rate, bpm | 65 ± 12 | 64 ± 9 | 0.73 |
| PR intervals, ms | 166 ± 18 | 167 ± 26 | 0.84 |
| QRS duration, ms | 100 ± 12 | 96 ± 13 | 0.12 |
| QT interval, ms | 379 ± 39 | 392 ± 22 | 0.54 |
| Corrected QT intervals, ms | 410 ± 23 | 404 ± 23 | 0.24 |
3.2 Comparisons between patients with IVF and those with BrS
The clinical and ECG characteristics of 35 patients with IVF and 15 patients with BrS are shown in Table 2. The ECGs were obtained an average of 12 ± 6 times per person. Among patients with IVF, J point elevation ≥ 0.1 mV in the 3rd ICS was present in 14 patients. In 2 of them, J point elevation in the 3rd ICS sometimes disappeared in the ECGs recorded repeatedly in the outpatient clinic. All of other 21 patients without J point elevation ≥ 0.1 mV in the 3rd ICS did not have J point elevation during the follow-up. VF developed during physical efforts more often in IVF patients without J point elevation in the 3rd ICS than BrS patients (p < .05). There was no difference in activity status at the onset of VF between IVF patients with and without J point elevation in the 3rd ICS. There was no difference in other clinical characteristics and ECG findings among three groups. The frequency of inferolateral ER was similar in three groups. There was no difference in ECG findings except for Brugada ECG in three groups.
| IVF with J point elevation in the 3rd ICS (N = 14) | IVF without J point elevation in the 3rd ICS (N = 21) | BrS (N = 15) | P value | |
|---|---|---|---|---|
| Male sex, N (%) | 13 (93%) | 20 (95%) | 15 (100%) | 0.60 |
| Age, years | 44 ± 19 | 41 ± 15 | 42 ± 17 | 0.81 |
| Family history of sudden death, N (%) | 2 (14%) | 2 (10%) | 3 (20%) | 0.67 |
| Activity at initial cardiac event, N (%) | ||||
| Sleep | 3 (21%) | 2 (10%) | 6 (40%) | 0.09 |
| Arousal at rest | 8 (57%) | 8 (38%) | 8 (53%) | 0.48 |
| Physical effort | 3 (21%) | 11 (52%) | 1 (7%) | 0.01 |
| Inducible ventricular fibrillation | 5/10 (50%) | 6/11 (55%) | 4/6 (67%) | 0.81 |
| Inferolateral ER, N (%) | 3 (21%) | 3 (14%) | 2 (13%) | 0.81 |
| ECG parameters | ||||
| Heart rate, bpm | 63 ± 12 | 66 ± 12 | 63 ± 6 | 0.61 |
| PR intervals, ms | 158 ± 17 | 168 ± 18 | 178 ± 24 | 0.40 |
| QRS duration, ms | 102 ± 10 | 100 ± 12 | 104 ± 18 | 0.63 |
| Corrected QT intervals, ms | 409 ± 24 | 410 ± 20 | 407 ± 25 | 0.73 |
- Abbreviations: BrS, Brugada syndrome; ER, early repolarization; ICS, intercostal space; IVF, idiopathic ventricular fibrillation.
3.3 Clinical outcome
The follow-up period after ICD implantation in the IVF group with J point elevations in the 3rd ICS, the IVF group without, and the BrS group was 118 ± 80 months, 109 ± 61 months, and 105 ± 70 months, respectively. Two patients in BrS group were treated with bepridil. None of patients with IVF received antiarrhythmic drugs.
During a follow-up of 110 ± 69 months, the recurrence of VF was observed in 5 of 14 IVF patients with J point elevation in the 3rd ICS (36%), 2 of 21 IVF patients without J point elevation in the 3rd ICS (10%), and 6 of 15 BrS patients (40%). The frequency of VF recurrences was higher in IVF patients with J point elevation in the 3rd ICS and Brugada syndrome than IVF patients without J point elevation in the 3rd ICS (p < .05 for both). Electrical storm was observed in one of IVF patient (7%) with J point elevation in the 3rd ICS, none of IVF patient without J point elevation in the 3rd ICS, and one of BrS patient (7%). None of the patients died during the follow-up.
4 DISCUSSION
We directly compared ECG findings in the high ICS in IVF patients and generally healthy individuals. The frequency of J point elevation in high precordial leads was higher in patients with IVF than healthy controls, although the frequency of J point elevation in standard precordial leads was similar between two groups. Furthermore, J point elevation in high precordial leads was associated with risk of VF recurrences in patients with IVF.
4.1 Frequency of J point elevation in high intercostal spaces
There have been several reports on ECGs in high right precordial leads in healthy individuals. In a study from South Korea including 225 healthy men, J point elevation > 0.2 mV was observed in the 4th ICS in 0% of subjects and was observed in the 3rd ICS in 1.3%. (Shin et al., 2005) In a report from Turkey including 504 healthy men, J point elevation ≥ 0.2 mV was observed in the 4th ICS in 3% of subjects, whereas the prevalence increased to 5% in the 3rd ICS (Hunuk et al., 2013). In a report from Japan including 206 men, the prevalence of J point elevation ≥ 0.2 mV increased from 1.5% in the 4th ICS to 5.8% in the 3rd ICS (Hisamatsu et al., 2004). In this study, the prevalence of J point elevation ≥ 0.2 mV in healthy control group (1.9% of in the 4th ICS and 2.9% in the 3rd ICS) was similar to those in the previous studies.
The frequency of J point elevation in the 3rd ICS ≥ 0.1 mV was higher in patients with IVF than healthy controls, and the difference became more pronounced when limited to J point elevation ≥ 0.2 mV. There have been few previous studies investigating ECGs in the high ICS in IVF patients. In a study by Kamakura et al., (2016) including 32 patients with early repolarization syndrome, J point elevation ≥ 0.1 mV was observed in the 4th ICS in 8 patients (25%) and was observed in the high ICS in 13 patients (41%). The frequency of J point elevation in right precordial leads seems similar between the previous study and this study, although there were only 17% of patients with early repolarization syndrome in this study.
In the previous studies, day-to-day variation of the J wave and ST-T change was observed in the patients with Brugada syndrome and those with early repolarization syndrome. (Abe et al., 2010; Kitamura et al., 2017) In our study, 2 of 35 patients with IVF showed day-to-day variations in J point elevation in the 3rd ICS.
4.2 Characteristics of IVF patients with J point elevation in the 3rd intercostal space
There is a strong male dominance in IVF, early repolarization syndrome, and BrS. (Benito et al., 2008; Kamakura et al., 2013) Similar to these diseases characterized by risk of VF unassociated with structural heart diseases, majority of patients with J point elevation in the 3rd ICS were men (93%). In this study, VF occurred less frequently during exercise in IVF patients with J point elevation in the 3rd ICS than those without J point elevation in right ICS, suggesting that increased vagal tone is associated with risk of VF in patients with J point elevation in the 3rd ICS. In BrS, VF is associated increased vagal tone and often develops at rest and during sleep. (Matsuo et al., 1999; Mizumaki et al., 2004) The characteristic J point and ST-segment elevation is often pronounced in the 3rd and 2nd ICS in BrS. Although Type I Brugada ECG was not observed in patients with J point elevation in the 3rd ICS at rest and during sodium channel blocker test, IVF with J point elevation in the 3rd ICS and BrS share clinical and electrophysiological characteristics, suggesting the presence of common arrhythmogenic substrate between two disorders.
Kamakura et al., (2013) reported that the frequency of VF recurrences is higher in ERS patients with J point elevation in standard and/or high right ICS (58%) than those without J point elevation in right ICS (11%). In this study, the frequency of VF recurrences was also higher in IVF patients with J point elevation in high right ICS (36%) than those without J point elevation in right ICS (11%). Taken together, J point elevation in 3rd ICS may be an electrographic risk factor for VF recurrence in patients with VF unassociated with structural heart diseases.
4.3 Study limitations
This study had some limitations. This was a retrospective analysis at a single center. The small number of IVF patients may have influenced our interpretation of the results, despite the number being comparable to other previous studies. (Kamakura et al., 2013, 2016) There is a need for a large prospective study.
5 CONCLUSION
Our study found that the prevalence of J point elevation in the 3rd ICS was high in patients with IVF. J point elevation in the 3rd ICS may be a risk factor for VF recurrence in patients with IVF. Electrocardiogram recordings in high ICS may be useful to identify risk of sudden death.
Disclosures
None declared.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.