People with epilepsy still feel stigmatized
Funding information
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines
Abstract
Objectives
Those affected with epilepsy have long been subject to stigmatization. This may have manifold negative effects, for example social isolation, low self-esteem, reduced quality of life and worsening of seizures.
In Norway educational programs have been arranged at the National Centre for Epilepsy, aiming at reducing stigma and shame associated with epilepsy, and thereby increase the quality of life for those affected and their families. Thus, we wanted to explore the extent of self-reported perceived stigma and experienced discrimination in a Norwegian cohort with epilepsy.
Materials and Methods
We conducted a web-based questionnaire survey in Norway. Participants were asked to provide background and epilepsy-related information. In addition, they were encouraged to answer questions regarding felt stigmatization in different situations and to rate stigma according to the Jacoby stigma scale.
Results
Of 1182 respondents, 56% reported to have felt being stigmatized, and 35% reported to have experienced discrimination solely on the ground of the disease. 70% of respondents reported at least one type of perceived or experienced stigma. After controlling for gender, age, perceived depression and seizure freedom, reports of experienced stigmatization was a statistically significant independent predictor for reduced quality of life.
Conclusions
A considerable proportion of people with epilepsy in Norway feel stigmatized and/or subject to discrimination, which negatively affects their quality of life.
1 INTRODUCTION
Epilepsy is one of the most serious neurological conditions and is characterized by recurrent epileptic seizures. The disease may have a big impact not only on those affected, but also on their families and, indirectly, the community. Historically the condition has been associated with stigmatization and negative attributes.1
Stigma has been defined as an attribute, behaviour, or reputation that is socially discrediting in a particular way by causing an individual to be mentally classified by others in an undesirable, rejected, stereotyped way.2 According to the World Health Organization (WHO), there are two main types of stigma: (a) Felt stigma and enacted stigma. Felt stigma is the experience of being stigmatized and describes the fear of encountering stigmatization and the self-inflicted, internalized, negative self-evaluation produced by such encounters.2 Felt stigma can be reported by the person with epilepsy themselves (b) Enacted stigma is the occurrence of discrimination solely on the basis of the disease.2 Enacted stigma is usually discovered by investigating social prejudices against the person with epilepsy.3 Felt stigma is far more prevalent than enacted stigma and has been shown to be associated with low level of education and knowledge about epilepsy, both in the people with epilepsy feeling stigmatized and in their peers contributing to stigma.2, 4, 5
Studies have also revealed that stigma affects the quality of life more than clinical variables like seizure types and frequency, and side effects of drugs.6
It is important to emphasize that the effects of stigmatization and discrimination may be manifold; social isolation, low self-esteem, poor mental health, reduced quality of life, worsening of seizures, choosing to conceal their disease, increased risk of non-adherence, and adverse effects of anti-seizure medications are all potential consequences.7-12
Many factors may have an impact on the integration of people with epilepsy into society. These include the individual patient's intellectual ability, educational level, mental stability, attitudes, and social support in their family, along with transportation and employment opportunities, and the ability to overcome stigma.13
One of the most important tasks of the Norwegian Epilepsy Association in recent decades has been to reduce the stigmatization of people with epilepsy in Norway. Increased awareness, education and information about epilepsy, better health service and less discrimination of this patient group have been the goal.
Since 2006, targeted educational programs have been arranged at the National Centre for Epilepsy, aiming at reducing stigma and shame associated with epilepsy and thereby increase the quality of life for those affected and their families. Thus, we wanted to explore the extent of self-reported perceived stigma and experienced discrimination in a Norwegian cohort with epilepsy.
2 MATERIAL AND METHODS
2.1 Online questionnaire
This study was a collaboration between the National Centre for Epilepsy and the Norwegian Epilepsy Association (NEA). An online questionnaire was developed and made available on NEA's homepage as a pop-up for all those visiting the page between 1 April 2017 and 5 September 2017.
All people with epilepsy visiting the homepage were asked to complete a questionnaire regarding their epilepsy. Questions had been selected following a thorough discussion among colleagues at the National Centre for Epilepsy and staff members from the NEA. Questions included background information such as gender, age, and cohabitation, perceived general and mental health, and quality of life. The epilepsy-related questions included, among other things, seizure type and frequency. As the prime drive behind the project was the NEA's need for information on which it could build member services and health policy initiatives, it was decided to keep the questionnaire short.
In order to evaluate felt stigmatization or discrimination, the participants were requested to answer the following questions: “Have you experienced discrimination related to your epilepsy?” The respondents could answer “yes “or “no”. Those who answered “yes” were asked to describe the situations in which they had experienced discrimination/stigmatization: in the family, at school or work, in daily life, from public administration, or from healthcare providers. In addition, we used the established stigma scale by Jacoby that includes the following questions: “Have you felt that, because of your epilepsy, other people were uncomfortable with you?”; “Have you felt that, because of your epilepsy, others considered you inferior?”, “Have you felt that, because of your epilepsy, other people preferred to avoid you?”14 Respondents could tick more than one possibility. A stigma score was calculated from the number of affirmative answers (0–3).14
Quality of life among respondents was evaluated from a visual analogue scale from 0 (worst possible) to 10 (best possible). Results were used as a continuous variable in further analysis. Feelings of depression in the respondents were evaluated from the question: “To what degree has feeling depressed been problematic for you?” The response categories were: 1 = “not at all”, 2 = “to a lesser degree”, 3 = “somewhat” and 4 = “very much”. The response variables were stratified into 1 = “not feeling depressed” (categories 1 and 2), and 2 = “feeling depressed” (categories 3 and 4).
The study was fully anonymized and consent was assumed if the respondent answered the questionnaire. The study was evaluated and approved by the Regional Ethics Committee (ref.no.:2017/563) prior to implementation.
2.2 Statistics
IBM SPSS Statistics version 25, release 25.0.0.1 (SPSS Inc.,) was used for statistical analyses. A difference of ≥1 point on the 0–10 scale of the QoL scores was considered clinically relevant and a p-value of 0.05 was considered statistically significant. The associations between changes in the QoL rating and the independent factors were estimated with linear regression analysis with confidence intervals (CI) at a level of 95%.
The dependent variable was quality of life, explanatory variables included were feeling depressed, having been seizure free for the previous 12 months, gender, and age. To avoid modelling the effect of age as linear, patients were distributed into four age groups (each representing about 25% of the respondents: “under 30”, “30–41”, “42–52” and “over 52”) and age was represented in the regression model by a set of dichotomized dummy variables.
3 RESULTS
During the study period, 48,249 users visited the website, and 1,182 people with epilepsy participated in the survey and completed the questionnaire, at least partly. All reported results were included in the analysis. Demographic and clinical characteristics of the participants are summarized in Table 1.
| Male gender; n (%) | 372 (32.3) |
| Age in years; mean (range) (SD) | 41.8 (11–93) (14.9) |
| QoL; mean (range) (SD) | 6.5 (0–10) (2.214) |
| Feeling depressed; (n = 1151) n% | 677 (58.8) |
| Seizure free for 12 months; n (%) | 479 (40.6) |
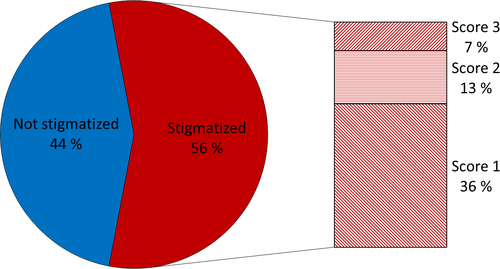
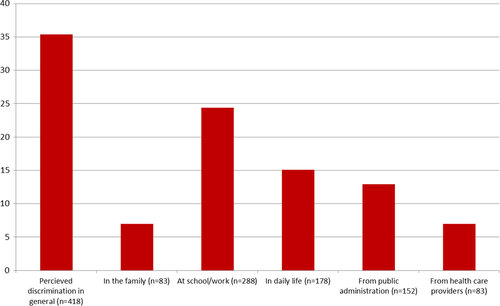
Of the 1,182 respondents, 56% reported that they had experienced at least one stigmatizing situation, and about 20% reported that they had experienced more than one such situation (Figure 1). 36% of the respondents reported being discriminated against due to their epilepsy, with most respondents saying that this happened at school or at work (24%), and to a lesser degree in daily life, from public administration, from healthcare providers, or among the family (Figure 2). 38% (446 respondents) reported having experienced that others were uncomfortable around them, 22% (265 respondents) that others treated them as inferior, and 23% (276 respondents) that others preferred to avoid them. 70% of the respondents had reported at least one type of perceived or experienced stigma.
After controlling for gender, age, perceived depression, and seizure freedom, experienced stigma was shown to be a statistically significant predictor of the respondent`s quality of life (Table 2).
| Variable | b | 95% Confidence interval | p |
|---|---|---|---|
| Stigma | 0.49 | 0.35–0.62 | <0.001 |
| Feelings of depression | 1.62 | 1,39–1,85 | <0.001 |
| Not seizure free for 12 months | 1.07 | 0.84–1.30 | <0.001 |
| Gender | 0.23 | −0.02–0.47 | 0.067 |
| Age (29–41) | 0.32 | −0.27–0.34 | 0.837 |
| Age (42–52) | 0.05 | −0.26–0.37 | 0.739 |
| Age (≥53) | 0.18 | −0.14–0.51 | 0.270 |
4 DISCUSSION
The main findings in this study were that even in a high-income country like Norway, and even in an epilepsy population in which 40% had been seizure free for at least one year, 56% of respondents claimed that they had experienced stigmatization. Among these, 7% had a score of 3 on the Jacoby stigma scale meaning that they reported experiencing that due to their epilepsy people were uncomfortable with them, considered them inferior, and preferred to avoid them. 36% reported that they had experienced discrimination solely due to their disease. Perceived stigma influenced the respondents' quality of life even after control for age, gender, being seizure free and feeling depressed.
In a study by Baker et al.7 based on 5211 respondents, the Jacoby Stigma Scale was employed. The majority of the participants were recruited from France, Germany, The Netherlands and the United Kingdom, while the rest came from other European countries. They found that 51% reported experienced stigmatization and 18% had a Jacoby stigma scale score of 3.
Our figures are lower than those from a study in China, where about 90% of people with epilepsy reported having felt stigma,15 and about 50% considered epilepsy a “terrible condition”, especially young males in rural areas. In another Chinese study, most key informants considered concealment of epilepsy understandable. While the attitudes towards epilepsy were mostly negative in China, those with a more positive attitude had a medical background. Nevertheless, even among health professionals, in China epilepsy was considered as worse than other serious diseases.16
Psychiatric co-morbidities are common in people with epilepsy.17 Although three quarters of our cohort claimed to be in good health, about 60% stated that they had experienced symptoms of depression. It should be noted that patients suffering from both epilepsy and a psychiatric condition may be subjected to double stigmatization.18
Some older studies have revealed that stigma is positively associated with impaired self-esteem, self-efficacy, sense of mastery, perceived helplessness, increased somatic symptomatology, increased rates of anxiety and depression, and reduced life satisfaction.19-21
Baker et al.22 undertook a systematic review on this topic in North and South America, Europe, and Australia and found, from the 33 papers from 25 studies, that being married was associated with lower levels of experienced stigma. This supports our finding that living alone is associated with increased experienced stigma. However, in contrast to our findings, Baker et al. found that the level of stigma was higher among younger patients than among elderly patients. In Norway, with a good public-health system, younger epilepsy patients may receive better care, including more and better information about epilepsy than in some other countries, as the Norwegian Epilepsy Association has the last years put considerable emphasis on informing and educating adolescents with epilepsy.
Regarding factors that may predict felt or enacted stigma, Baker et al.22 identified culture, demography, and psychosocial health. We found that living alone was one such predictive factor and that this may be associated with poor psychosocial health. However, we did not find any correlation between depression and experienced stigma. In a recent study in patients who had recently had seizures, Blixen et al.23 found a strong correlation between depression and stigma and that stigma had additional negative health effects. In our study, in contrast, many patients were seizure free and thus probably had less severe epilepsy and lower disease burden. This may explain the discrepancy.
About 25% of our respondents had experienced stigmatization or discrimination at school or at work. Assuming that attitudes towards epilepsy in the workplace are a reflection of attitudes towards epilepsy in society in general, our finding can be interpreted as implying that one out of four Norwegian patients with epilepsy experiences prejudices or negative attitudes towards epilepsy. One of our respondents reported that: “It is difficult to live with unpredictable seizures, but to experience my fellow workers’ reactions to hearing that I have epilepsy is even worse”.
About 7% of the respondents reported having been stigmatized by health personnel. In our experience, and also that of others,24 there are still many misconceptions regarding epilepsy, even among healthcare providers.
Our study has limitations. Social factors like income level, employment state, and level of education can probably influence felt stigma and quality of life. Unfortunately, we do not have information about these factors among our respondents. Only about 2.5% of the almost 50,000 visitors to the homepage participated in the survey. As 50,000 visitors constitute about 1% of Norway's population, more than the assumed number of people with epilepsy 0.65% (37.500); it is possible that during the study period, searches for “epilepsy” on the Norwegian Google site, resulted in the homepage of the NEA being listed first. Thus, everybody in Norway looking for information about epilepsy, not only patients and family members, may have visited the homepage of the NEA during the study period. As we do not have information about those visitors who chose not to participate in our survey, we cannot exclude a selection bias. For example, patients who do not feel that they have been exposed to stigmatization or discrimination may have less inclination to complete such a survey. Or on the contrary, people who feel stigma might be more willing to respond.
The stigma scale by Jacoby has been found to be internally consistent (α coefficients = 0.82 20 and 0.7725), but the other questions used have not been tested for reliability or validity even if they have face validity.
All information was provided anonymously. While this has definite disadvantages as we are not able to control information for example seizure type, it can also make respondents more inclined to answer.
The large sample size of over 1000 respondents strengthens our study.
The proportion of seizure-free patients (41%) was lower than expected in a representative sample of the Norwegian epilepsy population, and this may indicate that our study cohort is biased towards those with more severe epilepsy.
5 CONCLUSION
More than half of this large Norwegian cohort of people with epilepsy reported that they had been stigmatized, and more than one third had experienced discrimination solely on the basis of the disease. Thus, there is still a need for increased awareness and knowledge in the community regarding “the sacred disease”, even in high-income and high education countries like Norway. We believe the dissemination of evidence-based knowledge is the best prescription for fighting misconceptions and prejudices.
ACKNOWLEDGEMENTS
We are grateful to the Norwegian Epilepsy Association (NEA), which is the Norwegian branch of the International Bureau for Epilepsy, especially Henrik Peersen (Secretary General) and Therese Ravatn (Political advisor) for their valuable collaboration in this study. Thanks to Professor Lucy Robertson for critical reading and linguistic help and to Professor Dag Hofoss for critical reading and statistical help.
CONFLICT OF INTEREST
Oliver Henning has received speaker's honoraria from Eisai, UCB and Livanova. Morten I. Lossius has been paid for talks given in meetings arranged by Eisai and UCB, and for participation in expert panels for the same firms. Karl O. Nakken has received payment for lectures given in meetings directed by Eisai, UCB and Roche. Charlotte Buer has no conflicts of interest to disclose.
Open Research
DATA AVAILABILITY STATEMENT
Data available on request from the authors.




