Directly Acting Antivirals (DAAs) for the Treatment of Chronic Hepatitis C Virus Infection in Liver Transplant Patients: “A Flood of Opportunity”
Abstract
There is a tide in the affairs of men. Which, taken at the flood, leads on to fortune
(Shakespeare: J Caesar Act 4, scene 3)
Abbreviations
-
- DAA
-
- directly acting antivirals
-
- GT
-
- genotype
-
- HCC
-
- hepatocellular carcinoma
-
- HCV
-
- hepatitis C virus
-
- LT
-
- liver transplantation
-
- PEG-IFN
-
- pegylated interferon
-
- PI
-
- protease inhibitor
-
- RBV
-
- ribavirin
-
- SOF
-
- sofosbuvir
-
- SVR
-
- sustained virological response
Introduction
Chronic hepatitis C virus (HCV) infection is a global epidemic affecting almost 180 million people, with an estimated 3–4 million new infections every year 1, 2. Unfortunately, low treatment uptake combined with an aging HCV-infected cohort effect has resulted in increasing rates of complications. The proportion of the HCV-infected population with established cirrhosis is projected to double over the next decade 3, 4 and numbers with hepatocellular carcinoma (HCC) and liver failure will treble by 2030 5-7. HCV-related liver failure and HCC are already the leading indications for liver transplantation (LT) 8, 9.
In a patient with active HCV infection at the time of LT, infection of the allograft is universal at the time of reperfusion. The natural history of HCV is accelerated following LT with 20–40% progressing to cirrhosis within 5 years 10-12. As a result, graft and patient survival following transplantation for HCV cirrhosis is reduced compared with other elective indications 13.
The increasing demand for transplantation for HCV-related end-stage liver disease, combined with the negative impact of recurrent HCV on patient and graft survival, has made recurrent hepatitis C the biggest unmet medical need facing LT units.
The primary goal in the management of recurrent HCV is prevention of graft loss through delay or prevention of fibrosis progression. Although several baseline viral, donor and recipient factors are associated with more rapid progression of HCV recurrence, few can be prospectively altered (Table 1). The only intervention that has been demonstrated to improve graft and patient outcomes is successful eradication of HCV infection with antiviral therapy either before or after LT 14.
| (a) Pretransplant | (b) Posttransplant |
| Viral factors | Immunosuppression |
| High viral load | Adjuvant therapy for rejection |
| HIV co-infection | Rapid weaning of steroids |
| Host factors | Pattern of recurrence |
| ↓CD4+, CD8+ responses | Cholestatic hepatitis |
| ↓innate NK/NKT responses | Severe inflammation at 1 year |
| Cryoglobulinemia | Persistently elevated ALT |
| IL-28B genotype | Early high HCV RNA levels |
| (c) Donor | |
| Older age | |
| Female donor | |
| DCD donor | |
| Steatosis | |
| Diabetes | |
| Ischemic time | |
| IL-28B genotype | |
- ALT, alanine aminotransferease; HCV, hepatitis C virus; NK, natural killer; NKT, natural killer T cell.
The effectiveness of antiviral therapy against chronic HCV mono-infection has improved dramatically over the past decade, with expected sustained virological response (SVR) rates of almost 75% in previously untreated patients, regardless of genotype. For patients infected with HCV genotype (GT)-2 or -3, the current standard of care is pegylated interferon plus ribavirin (PEG-IFN/RBV) for 24 weeks. For patients infected with HCV GT-1, the addition of one of the two recently approved first-generation protease inhibitors (PIs), telaprevir and boceprevir, to PEG-IFN/RBV for 48 weeks has increased the SVR rate from 45% to 75% and allowed shortened duration of therapy in most patients to 24–28 weeks.
However, these major advances in the treatment of HCV have not delivered a similar impact in the treatment of HCV recurrence. Post-LT patients represent a challenging population with multiple baseline negative predictors for viral response to IFN, including (i) host factors such as non-CC IL-28B genotype which is a negative predictor for response to retreatment with currently licensed; (ii) viral factors such as high prevalence of HCV GT-1 infection and high pretreatment viremia levels 1–2 logs higher than pretransplant, usually exceeding 106 units/mL 12, 15, 16; (iii) direct effects of immunosuppression on IFN efficacy through blunting of HCV-specific T cell immune responses 17, 18. The most negative predictor for viral response is lack of tolerability from PEG-IFN/RBV—more than 80% of patients dose reduce and almost 30% cease therapy because of adverse effects. This reflects the co-morbidity spectrum associated with LT encompassing renal dysfunction, cytopenias and diabetes mellitus.
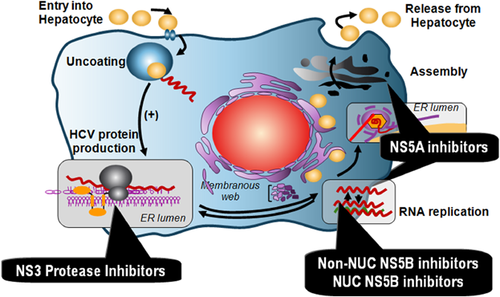
This review focuses on recent advances in antiviral therapy against HCV and their relevance to management of HCV infection before and after LT. We highlight the specific safety and tolerability issues associated with directly acting antiviral agents (DAAs) and summarize the efficacy of these DAA regimens in Phase II studies in these difficult-to-treat patient populations (Figure 1).
Current Therapies
SVR rates achieved with PEG-IFN/RBV in LT recipients with recurrent HCV GT-1 are significantly lower than those in non-LT patients. In the US multicenter PROTECT study, which is the largest open-label study to-date of PEG-IFN/RBV for recurrent HCV infection, only 36/125 (29%) patients achieved SVR following 48 weeks therapy 19. Other studies report SVR rates from 18% to 43% (see Figure 2) 20-22.
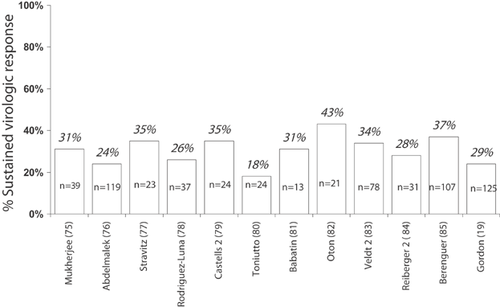
Studies have identified a number of baseline viral and host factors associated with SVR, of which viral genotype non-1 and host IL-28BCC genotype are the strongest predictors (see Table 2). IL-28B encodes for IFN-lambda and modulates host IFN-stimulated gene response to exogenous IFN, with the CC genotype associated with favorable response and SVR. In LT recipients with recurrent HCV, both donor and recipient IL-28B genotypes appear to be important in determining response to PEG-IFN/RBV. The highest rates were achieved when both donor and recipient were matched CC (86%) and lowest SVR rates when both were non-CC (16%) 23, 24.
| 1. Host factors |
| Younger donor age |
| Lack of severe fibrosis |
| Lack of insulin resistance |
| Donor IL-28B genotype CC |
| Recipient IL-28B genotype CC |
| 2. Viral factors |
| Low pretransplant viremia level |
| Low posttransplant viremia level |
| HCV genotype 2/3 |
| Lack of HIV co-infection |
| 3. Treatment-related factors |
| Early on-treatment response |
| Adherence to PEG-IFN and RBV |
| Reduced time since transplant |
| Maintenance cyclosporine |
Timing of commencement of antiviral therapy influences the likelihood of response. Several trials of early “preemptive” therapy prior to the onset of established graft fibrosis have reported very poor efficacy and tolerability due to the presence of renal impairment and cytopenias. In the largest randomized study of early preemptive therapy with PEG-IFN/RBV (the PHOENIX study), the rates of histological recurrence, graft loss and death were similar in the active and control groups 25. Thus, antiviral therapy is best undertaken for established HCV recurrence rather than preemptive therapy. Given the limitations of current therapy, treatment should target those recipients with the greatest chance of response (including HCV GT-2/3 or GT-1/4 with D/R IL-28B CC genotype) and those at highest risk for rapid fibrosis progression, recurrent cirrhosis and graft loss. The most reliable predictor is the presence of moderate histological necroinflammation or fibrosis in the 1-year protocol allograft biopsy 26-28. Measurement of hepatic venous pressure gradient may also be a valuable tool for predicting disease progression—in one study, the presence of hepatic venous pressure gradient of 6 mmHg or greater at 1 year posttransplant was strongly associated with subsequent hepatic decompensation 29.
Finally, the choice of maintenance immunosuppression may impact on the outcome of HCV antiviral therapy. Several studies have reported higher SVR rates in patients receiving cyclosporine than in those receiving tacrolimus because of a lower risk of relapse 30, 31. The proposed mechanism is thought to be from a direct antiviral effect of cyclosporine through inhibition of NS5B binding to cyclophillin B 32. This effect, however, is small, and currently, there is no firm evidence base to recommend switching patients to cyclosporine prior to commencing antiviral therapy 33.
The development of robust models of HCV replication has driven the development of new classes of therapeutic agents termed DAAs, which are rapidly moving into the clinical arena. Importantly, rapid advances with new DAAs in the clinical trial environment utilizing combinations of different classes seem destined to deliver effective efficacy (approx. 90%) and allow shorter exposure, or indeed no exposure, to PEG-IFN. Since 2011, for patients with HCV GT-1infection, first-generation PIs, telaprevir and boceprevir, in combination with PEG-IFN/RBV is the standard of care in non-LT HCV, offering further improvements in SVR from 40% to 70–75% with shortened viral response guided duration 34-37.
Initial large clinical trial data sets have now been supplemented by real-life experience in patients with advanced HCV cirrhosis and portal hypertension. The CUPIC (Compassionate Use of Protease Inhibitors in Viral C Cirrhosis) cohort demonstrated a higher rate of serious adverse events (49% telaprevir; 38% boceprevir) and a high rate of discontinuation due to severe adverse events (15% telaprevir; 7% boceprevir) 38. Grade 2 anemia (hemoglobin [Hb] <10.0 g/dL) occurred in approximately 20% of patients receiving telaprevir or boceprevir, while Grade 3/4 anemia (hemoglobin [Hb] <8.0 g/dL) occurred in 10% of patients, despite liberal use of growth factor support and blood transfusion; 71% of patients on telaprevir and 61% of patients on boceprevir had undetectable HCV RNA after 16 weeks of treatment 39. However, the final SVR rates (40–41%) are sobering and reflect the complexity of PI-based, PEG containing triple therapy in this advanced population with the significant risks of sepsis, hepatic decompensation and death.
At present, the use of PI-based triple therapy cannot be recommended in patients' evidence of borderline decompensation due to a significant additive toxicity profile, with those having an albumin of <30 g/L and platelet count of <100 000/m3 demonstrating a 50% risk of decompensation with PI-based triple therapy.
PI-based triple therapy might play a limited role in patients listed for LT with HCC and compensated HCV cirrhosis. One study, reported in abstract form, treated 20 patients who were awaiting LT with predominately telaprevir, demonstrating 44% had undetectable HCV viral load at 4 weeks rising to 71% at 12 weeks 40. Triple therapy was discontinued early in 25% of patients and 10% decompensated on treatment but 6/8 remained HCV negative at 12 weeks post-LT, inferring a lack of allograft infection.
Given the increasing impact of recurrent hepatitis C and lack of efficacy of PEG-IFN/RBV, it is not surprising that PI-based triple therapy has been attempted in this post-LT “population of need.” Small case series and real life experience have preceded clinical trial data in this population, with SVR efficacy outcomes now reported in predominantly abstract form. Early pharmacokinetic data tempered expectations in the post-LT group. Data on the use of telaprevir in healthy volunteers resulted in a significant increase in cyclosporine (fivefold) and tacrolimus levels (70-fold) due to the inhibition of the cytochrome P450 3A metabolic pathway 41. Drug–drug interactions remain a significant clinical issue and concern regarding toxicities and risk of rejection given the use of first-generation PIs with PEG-IFN/RBV mandated a cautious approach for clinicians. The required reduction in tacrolimus dosing (80–95%) is greater than that for cyclosporine (50–75%) 42-44.
An early report demonstrated significant drug–drug interactions between calcineurin inhibitors and boceprevir in five patients post-LT. Reduction in cyclosporine dose of 50% and up to 80% reduction in tacrolimus dose were required, steady levels being achieved by 4 days. Follow-up was limited to treatment week 12 but all patients achieved a virological response (≥2 log drop) during this time. Anemia was the more frequent side effect with all patients requiring erythropoietin. Although the numbers are small, this study demonstrated “proof of concept” that the newer DAAs can be used safely with encouraging on-treatment virological response rates.
- PI-based therapy has only been utilized in HCV patients with established recurrence. Parallel to the non-LT experience, outcomes and safety seem better in those without advanced HCV recurrence. Similarly, toxicity is similar to that reported in non-LT cohorts but with additive anemia, additive complexity in management, increased discontinuation rates and poor tolerability. Increased incidence of sepsis, requirement for dose adjustment and hospitalization is demonstrated. Two multicenter observational reports (US CRUSH-C Group and the European LT Group) both report SVR12 rates of approximately 50% in GT-1 HCV patients 42, 43. Discontinuation rates were observed in 23% of CRUSH-C and 40% European series (which comprised a higher proportion of recipients with more advanced HCV recurrence). Blood transfusion was required in 46% and 35% of patients, respectively. Additionally, mortality associated with sepsis and hepatic decompensation in advanced recurrent HCV post-LT was reported.
- Switching patients to cyclosporine appears to be common due to smaller variations in dosing, although tacrolimus-based immunosuppression levels appear to be manageable 46, 48. Meticulous management of immunosuppression with PI-based therapy avoids graft dysfunction and rejection.
- The use of a lead in phase with PEG-IFN/RBV informs patient and graft tolerability prior to the additive introduction of PI is widespread.
- The number of patients being treated is small. No data are currently available regarding the development of viral resistance and its impact in the post-LT period.
A Phase IIIb study of the use of telaprevir (REPLACE) in stable, noncirrhotic LT patients with GT-1 disease is currently ongoing and will report in early 2014 49.
Overall, evidence is accruing that PI-based, PEG-IFN containing antiviral therapy is feasible and can deliver SVR, albeit at the price of significant toxicity and requiring intensive and meticulous on-treatment management. Although more effective and better tolerated IFN-free therapies are being developed, at this time, PI-based triple therapy should still be considered for those patients who are at greatest risk of graft loss and who have baseline predictors of response.
Combination DAA Therapy to Treat Established Recurrent Hepatitis C
The poor safety and efficacy of IFN-containing regimens in patients with end-stage liver disease and in LT recipients have hastened the development of IFN-free strategies for the prevention and treatment of recurrent HCV infection.
The HIV treatment paradigm suggests that combining DAAs, which target different steps of viral replication, should provide additive and possibly synergistic antiviral potency, prevent the emergence of DAA resistance and consequently remove the need for IFN. The first IFN-free DAA combinations against HCV consisted of a PI and a non-NUC-NS5B inhibitor—both DAA classes with low barriers to resistance 50-52. Unfortunately, rapid emergence of dual resistance resulted in high rates of virological breakthrough and relapse, especially in patients infected with HCV subtype 1a and prior null responders to IFN-based therapy.
Fortunately, the addition of a third DAA, an NS5A inhibitor, to a PI and non-NUC NS5B inhibitor (ABT-267/ABT-333-r/ABT-450; daclatasvir/asunaprevir/BMS-791325) prevents the emergence of resistance and improves efficacy to over 90% across all HCV GT-1 patient populations, including those infected with subtype 1a and prior null responders 53, 54. These triple DAA regimens are now in Phase III registration studies for treatment of patients with chronic HCV infection GT-1. However, before they can be used to treat transplant recipients with recurrent HCV infection, extensive drug–drug interaction studies with the calcineurin inhibitors are required because both the PIs and the non-NUC NS5B inhibitors are substrates and inhibitors of CYP-3A4 and Pg-p metabolic pathways.
In contrast to the other DAA classes, the nucleotide polymerase inhibitors (NUCs) appear ideally suited for use following LT. Because these agents do not undergo hepatic metabolism, NUCs do not require dose adjustment in patients with allograft dysfunction and do not interact with calcineurin inhibitors. NUCs are chain terminators of HCV RNA synthesis. The target is the highly conserved catalytic site of the RNA-dependent RNA polymerase, thereby conferring pan-genotypic antiviral potency and a very high barrier to resistance. The uridine-based NUC sofosbuvir (SOF) was recently approved by the US Food and Drug Administration for the treatment of chronic HCV infection GT-1/2/3/5 55. In Phase III studies in non-LT patients, 24 weeks of SOF plus RBV achieved SVR in 97% patients infected with HCV GT-2 and 85% infected with GT-3 56-58. This same regimen achieves SVR12 in 55–84% patients with HCV GT-1 infection. No specific toxicities have been observed in more than 3000 patients treated to date.
The addition of an NS5A inhibitor (either daclatasvir or ledipasvir) to SOF increased the SVR rate to 100% across different patient populations including cirrhotic and prior nonresponders to both PEG-IFN/RBV and triple therapy with telaprevir or boceprevir 59-62.
The efficacy and safety of IFN-free SOF-based regimens in LT recipients with recurrent HCV were confirmed in the published case report of successful rescue of an LT recipient with cholestatic HCV following 24 weeks treatment with SOF plus daclatasvir—an NS5A inhibitor 63. At the time of treatment initiation, this patient had advanced allograft failure (jaundice, encephalopathy and refractory ascites with Model for End-Stage Liver Disease score of 24). Rapid viral suppression was accompanied by resolution of ascites and recovery of liver synthetic function, and at the time of writing, the patient remains well with normal allograft function and undetectable HCV RNA, more than 2 years posttreatment. Following this remarkable rescue of what had previously been a universally fatal condition, Gilead Sciences instituted a compassionate access program of SOF/RBV for LT recipients with allograft failure from severe recurrent hepatitis C 64. In the first 44 patients (almost half with fibrosing cholestatic hepatitis C), on-treatment viral suppression was achieved in 78% and SVR in 69%. Virological response was associated with resolution of clinical signs of decompensation. Eight patients died during this study from complications of liver failure, reflecting the severity of liver disease at study entry.
In the first open-label Phase II study, 40 LT recipients with compensated recurrent hepatitis C (all HCV genotypes) were treated with SOF/RBV for 24 weeks 65. All patients achieved RVR (undetectable HCV RNA at 4 weeks) and 77% achieved posttreatment SVR4.
It is expected that the addition of a second DAA will improve efficacy and shorten the duration of therapy to 12 weeks. Therefore, in the larger follow-on study, 300 patients with both compensated and decompensated recurrent hepatitis C will be randomized to either 12 or 24 weeks of the fixed dose combination of SOF plus the NS5A inhibitor ledipasvir plus RBV 66. This study is actively recruiting and primary efficacy results are expected in late 2014.
In another open-label Phase II study, 30 LT recipients with compensated recurrent hepatitis C (HCV GT-1 only) are being treated with the AbbVie triple DAA regimen combined with RBV for 24 weeks 67. Careful adjustment of the calcineurin inhibitor dose will be required because of the inhibition of CYP-3A4 by the ritonavir-boosted PI ABT-450. This study is fully recruited and primary efficacy results are expected in mid-2014.
In the latest open-label Phase II study, 40 patients with compensated recurrent hepatitis C (HCV subtype 1b only) will receive daclatasvir (NS5A inhibitor), combined with simeprevir (PI recently approved by the US Food and Drug Administration in combination with PEG-IFN/RBV) and RBV for 24 weeks 68. This study has not yet commenced recruitment and primary efficacy results are expected in mid-2015.
Combination DAA Therapy to Prevent Recurrent Hepatitis C
Universal prophylaxis before or at the time of transplant to prevent HCV infection of the allograft is the ultimate goal. SOF-based regimens seem ideal for this purpose because of the excellent tolerability and lack of hepatic metabolism. In a recent landmark study, SOF plus RBV was administered to LT candidates listed with compensated HCV cirrhosis and HCC for 48 weeks or until the day of LT (whichever occurred earlier) 69. Of the 41 who have been transplanted, 65% have remained free from recurrence at least 6 months post-LT. The best predictor of freedom from HCV virological recurrence was the length of time that serum HCV RNA target was not detectable by sensitive PCR assays (target not detected [TND]) prior to transplant. HCV recurred in only 1/24 patients with TND for 30 days and in none if TND for 90 days.
It is hoped that successful HCV eradication in patients with decompensated HCV will rescue many patients from the need for transplantation, analogous to the impact of oral antiviral therapies in decompensated chronic hepatitis B 70. The rapid viral suppression to undetectable and normalization of alanine aminotransferease observed in the Phase II and III programs of SOF/RBV would suggest that this treatment in patients with decompensated HCV cirrhosis will improve liver synthetic function and remove the need for LT. An ongoing study is now evaluating the safety and efficacy of SOF/RBV in patients with decompensated HCV cirrhosis 71.
Like NUCs, the NS5A inhibitors have an excellent safety profile and do not undergo hepatic metabolism and both seem ideally suited for use in patients with end-stage liver disease. A study with the fixed dose combination of SOF plus ledipasvir is currently under way 66. It seems possible that the increased antiviral potency of this combined DAA regimen will improve the likelihood of rescue from transplantation in patients with decompensated cirrhosis.
Although widespread uptake of effective combination DAA therapy should reduce the demand for transplantation for HCV-related liver failure, this may be offset by increasing demand for HCV-related HCC because: (i) there already exists a large population with established cirrhosis at risk for this complication; and (ii) DAA therapy will dramatically reduce end-stage liver disease deaths in this cirrhotic population, thereby increasing the number of patients with cirrhosis who remain at risk for HCC 72. Longer follow-up of DAA studies in HCV cirrhosis will determine whether successful treatment will result in fibrosis regression and reduction in life-time risk of HCC, as has been observed with hepatitis B virus therapy 73, 74.
Conclusions
HCV cirrhosis remains the leading indication for LT and this demand is projected to double in the next decade. Unfortunately, HCV infection of the allograft is universal and associated with accelerated disease progression with reduced graft and patient survival compared to other transplant indications.
Current antiviral therapy, with a PEG-IFN/RBV component, has limited applicability peri- and post-LT because of poor tolerability and efficacy in these patient populations. The improved efficacy of first-generation PIs, boceprevir and telaprevir, in the treatment of recurrent hepatitis C is offset by increased toxicity in LT recipients, especially anemia, and significant drug–drug interactions, especially with tacrolimus.
In contrast, the NUC-NS5B inhibitors and the NS5A inhibitors lack toxicity and significant drug interactions with either cyclosporine or tacrolimus and seem ideally suited for post-LT treatment of recurrent HCV infection. Recent clinical studies of SOF plus RBV therapy confirm the safety and efficacy of IFN-free DAA therapy before and after LT. Subsequent studies of DAA combinations (SOF plus ledipasvir, or ABT-450/ABT-333/BT-267) are expected to achieve almost 100% response with shorter duration of therapy.
In summary, chronic hepatitis C is both the leading indication for LT and the leading cause of posttransplant graft loss. The poor tolerability of IFN-based therapy in decompensated liver disease has limited pretransplant treatment to well-compensated patients listed for HCC. The primary goal of IFN-based antiviral therapy was to improve posttransplant outcomes through delayed treatment of patients with established recurrence in the allograft. The superior efficacy and tolerability of direct antiviral agents should move the primary goal of antiviral therapy to universal pre-LT prophylaxis in all patients listed with HCV cirrhosis, thus abrogating the impact of HCV allograft infection and improving long-term graft and patient survival. Finally, combination DAA therapy may salvage patients presenting with decompensated HCV cirrhosis, thereby reducing both the demand for LT and the need for re-LT.
Disclosure
The authors of this manuscript have conflicts of interest to disclose as described by the American Journal of Transplantation. EJG acts as speaker/advisor for Janssen, Merck, Gilead, AbbVie, BMS, BI, Astellas and Novartis. KA acts as speaker/advisor for Janssen, Merck, BMS, Gilead, AbbVie, Astellas and Novartis.