Allied Health Student-Led Clinics: An Opportunity for Workforce Development
ABSTRACT
Objective
The project evaluated multidisciplinary allied health student placements co-located within a rural general practice clinic.
Methods
Occupational therapy, social work and speech pathology placement students under discipline-specific supervision led an allied health clinic model servicing clients with diverse health needs.
Design
A cross-sectional survey design recording interventions, student and stakeholder experiences and client satisfaction was applied.
Setting
General Practice clinics in MMM 4–6 regions in Queensland.
Participants
Between February and July 2024, 10 students completed placements within the student-led clinic, working with clients.
Main Outcomes Measure
Descriptive statistics were used to summarise clients' demographics, satisfaction and the services provided using SPSS version 29.0. Qualitative survey responses were analysed using Nvivo.
Results
Student-led allied health services co-located within a general practice clinic benefited rural communities by providing increased access to allied health services and a holistic approach to health care. Student-led allied health services alleviated the work burden for general practitioners (GPs) in a rural health care setting.
Conclusion
Multidisciplinary allied health student placements within a rural GP clinic benefited rural and remote communities through increased access to allied health services. Further research is needed to investigate interdisciplinary models of care and sustainable funding streams.
Summary
-
What is already known about this subject?
- ○
Research highlights the reduced access and availability of allied health services in rural areas.
- ○
Multidisciplinary teams provide holistic health care to individuals, leading to better health outcomes. Allied health services can reduce demand experienced by GPs.
- ○
-
What does this study add?
- ○
Student-led allied health services can address the needed gaps that rural communities experience in accessing allied health services. Allied student placements in rural and remote areas provide students with a valuable and diverse clinical placement. Such placements may be used as a workforce strategy to prepare students for rural and remote practice.
- ○
1 Introduction
In Australia, general practitioners (GPs) tend to be the first point of contact for patients seeking health care [1, 2]. Current challenges in primary health care include the ageing population, an increase in chronic health conditions, patients with complex and multiple issues, the prevalence of mental health concerns and inadequate Medicare billing rebates [2-5]. Overall, people living in rural and remote areas are at greater risk of poor health outcomes [4, 6, 7].
Allied health professions can alleviate some of the demand placed on GPs through interprofessional collaboration and patient care [8]. Barriers to multi-disciplinary team care include: GPs and allied health professionals are seldom co-located; practices' lack of capacity to coordinate care with other services; and limited understanding of allied health roles and competencies in health management [9-11].
Multi-disciplinary allied health student-led clinics assist students' understanding of their own profession, other professions' role and scope of practice and interprofessional teamwork [12-14]. Rural student-led allied health care hubs can improve the well-being of people and ‘are generally a ‘good fit” for student learning [15, p. 1179]. This study aimed to evaluate a multidisciplinary allied health student placement model co-located within a General Practice. This model was responsive to the health workforce shortages in rural and remote areas and provided an opportunity to prepare students for rural and remote practice and working in multi-disciplinary teams [16, 17].
2 Methods
The overall aims of this mixed methods research were to develop a model for allied health student-led clinic co-locating within a rural general practice and to evaluate the multidisciplinary allied health student placements and their outcomes. Students were recruited through the statewide university placement allocation process, except social work, whereby students were recruited through expressions of interest to individual universities. Four final year speech pathology (SP), three social work (SW) (one third year undergraduate, one final year undergraduate and one final year masters) and three occupational therapy (OT) (two third year undergraduate and one final placement masters) students completed their placements ranging between 6 and 16 weeks in an Emerald general practice, servicing MMM 4–6 regions in Queensland [18]. Students delivered services to clients by undertaking relevant professional tasks and practices, supported by discipline-specific supervision by qualified practitioners. A placement preparation curriculum, referral guidelines and checklists were created, and four education sessions for the GPs about the different allied health services were provided.
Data collection was via the online survey platform Redcap [19]. Students recorded client demographics and service provision. Clients, stakeholders and students were invited to provide feedback. Qualitative data were organised within NVivo 12.0 [20] and descriptive analysis was applied to the quantitative data using SPSS version 29.0 [21]. The qualitative data was analysed thematically [22]. Initial codes were generated and then categorised into themes and subthemes independently by two of the authors. These were then discussed and further refined through exploration and discussion with all authors [19, 22].
3 Results
3.1 Interventions
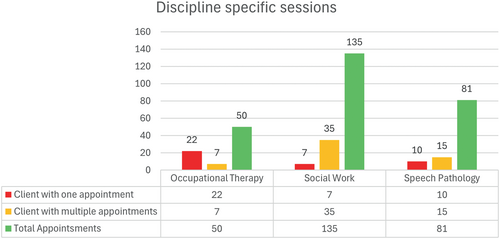
The student-led allied health clinic received 198 referrals February–July 2024. Of these, 94 clients were seen, resulting in 266 appointments. Social work students, in line with the length of their overall placement and type of service provided, had more appointments (n = 135) than OT (n = 50) and SP (n = 81). Encouragingly, students across all disciplines had clients who returned for repeat appointments (see Figure 1).
3.2 Client Satisfaction Survey Feedback
A total of 75 clients completed the client satisfaction survey offered to them at the end of their initial appointment, resulting in an 80% response rate. All respondents selected that they were likely to return to the student-led clinic, with 72 clients identifying they were very satisfied with the services (see Figure 2).
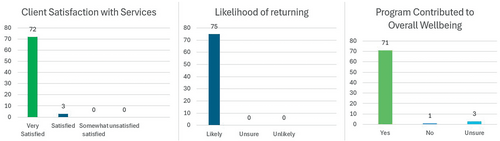
Clients were asked to consider the program's contribution to their wellbeing. Seventy-one highlighted that the student-led allied health clinic contributed to their overall wellbeing, with one selecting no and three being unsure.
3.3 Key Stakeholder Feedback
Seven GPs, two Practice Managers fully completed and one reference group member partially completed the stakeholder survey. Of the 10 respondents who ranked the question “The Allied Health Student Clinic co-locating with the GP practice is a model that is beneficial for rural communities”, six strongly agreed with the statement and one agreed. Three themes were identified in the data: access to health care, importance of collaboration and concern about standard of care.
3.3.1 Access to Health Care
Overall, the support for the model was very positive. Stakeholders noted that clients accessed previously unavailable services, found it easily accessible, received positive feedback, increased engagement in their healthcare and supported GPs in collaborative care, as reflected in the following comment: “Allows access for patients who have previously had no access, supports GPs in caring for their patients, increases patient engagement in their healthcare” [GP].
I have been able to give my patient's accessible comprehensive multidisciplinary care. Access that they have not had before. [GP]
I have increased the number of GP Management plans to assist in comprehensive care, now that patients can receive appropriate care. [GP]
This clinic has made an incredible difference to my patients and I hope that the university continues this program and expands this to enable more of our community to access the exemplary services. Well done to the team in and the initial rounds of students for making this happen! [GP]
3.3.2 Importance of Collaboration
Conversation with the GP to understand referral needs, case review together. Need to promote a health care team approach. [GP]
Improve avenues of communication that students have with GPs to better enable students to feel supported by GPs. [GP]
Making more time for GPs to feedback via case discussions to the students so they get feedback on the benefits their work is providing. [PM]
3.3.3 Concern About Standard of Care
Normalises below standard care for rural patients. Students are not a substitute for standard care. [GP]
4 Discussion
The research aims were to evaluate the multidisciplinary allied health student placements co-locating within a General Practice and their outcomes. Although this is a small cohort of students, the positive reception of the student-led services by key stakeholders highlighted that such clinics contribute to addressing allied health gaps in rural communities. It is recommended that allied health student-led clinics should be considered a workforce strategy to prepare students for rural and remote practice. Students on placement were supervised by qualified professionals and involved in interdisciplinary education sessions and engaged in reflective practice throughout their placement. This supported students in developing the necessary clinical skills for their discipline and rural practice [10, 15]. Students were able to see a range of clients in the clinic, highlighting that allied health student placements in rural and remote areas provide students with a valuable and diverse clinical placement [15].
Nevertheless, critique of some key stakeholders needs to be noted. An implicit assumption in the stakeholder feedback that allied health students may not be briefed in the same ways as medical students for placement suggests the need for further engagement of allied health and medical students during residencies and medical training [10]. It is imperative that allied health students are clearly communicating their competencies to minimise risk and to provide appropriate care to clients [10] and that programs, collaboration and communications are well planned and implemented [15].
Although there was an overall appreciation of the student-led clinic in offering access to allied health services for clients who previously did not have access, it reinforces the need for an innovative solution to address workforce shortages in primary health care [4]. Although students might not provide complex care services, they provided services that otherwise would not have been available under the supervision of qualified practitioners. Considering the prevalence and complexity of chronic health and mental health conditions in rural and remote areas and the absence of appropriate services when living remotely [4, 6, 7], the student-led clinics offered a valuable service. Allied health student placements reflect a commitment by universities to improve access to allied health services in rural areas and ensure that graduates are work ready for rural employment [16]. These programs need to be carefully evaluated to identify the quality of service delivery and outcomes for the community [15]. Moreover, the concern that the services provided should not replace fully qualified allied health care is valid, and appropriate health provision for rural and remote regions needs to be pursued.
Author Contributions
Taegen Pascoe: writing – review and editing, formal analysis, investigation, conceptualization, methodology, data curation, validation. Asmita Mudholkar: conceptualization, investigation, methodology, writing – review and editing, formal analysis, data curation, visualization, project administration. Stephanie Burke: conceptualization, investigation, methodology, writing – review and editing, formal analysis, data curation, validation. Kehinde Obamiro: conceptualization, investigation, methodology, writing – review and editing, formal analysis, data curation, visualization, validation. Ines Zuchowski: writing – original draft, investigation, conceptualization, methodology, writing – review and editing, formal analysis, data curation, validation.
Acknowledgements
The authors would like to thank the Emerald Medical Group who generously offered their rooms for the operation of the student-led allied health clinics. We would like to thank all the allied health students for their hard work and tenacity while working at the student-led clinic as part of their placement. This study was supported by the Rural Health Multidisciplinary Training (RHMT) program of the Australian Government Department of Health. Open access publishing facilitated by James Cook University, as part of the Wiley - James Cook University agreement via the Council of Australian University Librarians.
Ethics Statement
This study protocol was reviewed and approved by the James Cook University Human Research Ethics Committee, approval number H9224.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.