Developing a multivariate prediction model of falls among older community-dwelling adults using measures of neuromuscular control and proprioceptive acuity: A pilot study
Abstract
Objective
To examine whether measures of neuromuscular control and proprioceptive acuity were predictive of falls in an older community-dwelling population and to develop a multivariate prediction model.
Methods
Fifty-eight adults aged above 60 living independently in the community were recruited for a prospective falls study. On entry, they undertook a Sensory Organisation Test (SOT) and an Active Movement Extent Discrimination Assessment (AMEDA) and completed a short fall risk questionnaire. Participants were monitored for falls over the subsequent 12 months. Prior to analysis, falls were classified into three categories based on the difficulty of the activity being undertaken and the demands of the environment in which the fall occurred. Logistic regression was used to predict the probability of a fall.
Results
For falls occurring under the least challenging circumstances, the model fitted using the AMEDA score and two of the questions from the fall risk questionnaire, related to balance and confidence, achieved a specificity of 87% and sensitivity of 83%. Falls occurring in more challenging circumstances could not be predicted with any accuracy based on the variables recorded at inception.
Conclusions
This study highlights the importance of considering the heterogeneous nature of falls. Poorer proprioceptive acuity appears to play a role in falls occurring where neither the environment nor the activity is challenging, but not in falls occurring in other circumstances. Falls in the least-challenging circumstances affected 15% of participants, but this group was considerably more likely to have multiple falls, increasing their vulnerability to adverse consequences.
Practice Impact
This study highlights the heterogeneous nature of falls among older community-dwelling adults. Proprioception, as measured by active movement extent discrimination, is found to be predictive of falls in the least challenging circumstances. Conversely, the ability to put on socks while balanced on one leg appears to be protective against such falls. This has implications both for identifying those at increased risk of falls and measuring the effectiveness of interventions.
1 INTRODUCTION
The costs of falls, both financial and non-financial, are well-recognised1 and, with the ageing of populations in many countries, research into the factors that influence the risk of falls has assumed an increasing urgency.2 A large volume of published research has investigated possible contributory factors covering a multitude of domains, ranging from demographics, physical function, disease, medications, mental and cognitive function to lifestyle.3 A review of the literature by Ambrose et al.4 published in 2013 identified impaired balance and gait, polypharmacy and a history of previous falls as major risk factors, together with a host of other less-significant contributory factors.
A systematic review of fall prediction models published in 2021 found that ‘all models exhibited a high risk of bias rendering them unreliable for prediction in clinical practice’.5 Deficiencies have been identified in the falls literature around the definition of falls and recording of falls occurrence6 and attempts have been made to standardise the reporting of outcomes7 and establish protocols for transparent presentation of prediction model results.8 Given that proprioception, specifically ankle proprioception, has been found to be directly associated with two of the factors identified by Ambrose et al. as major risks for falls – balance9 and gait10 – a prospective study examining the role of proprioception in falls that complies with these recommendations around data capture, analysis and reporting is warranted.
Proprioception was described by Sherrington,11 a pioneer in this field, as the perception of the position and motion of the body in space. It is a complex mechanism, relying on a network of mechanoreceptors in the muscle spindles, joint tendons and glabrous skin surfaces, communicating through the afferent and efferent neural pathways, with cognitive function playing a key role in integrating these inputs with other sources of information from the visual and vestibular systems.12 In the context of falls, the evidence suggesting that, relative to young and middle-aged adults, older adults rely more heavily on proprioception rather than visual or vestibular cues in order to maintain postural control13 assumes particular importance.
Attempts to measure proprioceptive skill directly have relied on three broad approaches: joint position replication; time to detection of passive motion; and active movement extent discrimination. Each of these approaches has advantages and disadvantages14 and is thought, to some extent, to be measuring different aspects of proprioception.15 For the current study, we used an active movement extent discrimination assessment (AMEDA) apparatus designed to measure proprioception of the ankle joint with a testing protocol developed for an older population.16 As described in the Appendix S1, the apparatus allows a subject's ankle to be placed in different degrees of inversion and tests their ability to discern the direction of movement between successive inversions. The AMEDA has the advantage of testing skills in a weight-bearing unconstrained stance that is more akin to the situations in which proprioception is exercised in daily life. It has not previously been investigated as a possible predictor of fall risk.
The Sensory Organisation Test (SOT) measures proprioception and neuromuscular control in the context of an individual's ability to maintain balance under disruptions to the visual, vestibular and somatosensory systems. It has been used to measure the effectiveness of interventions to mitigate fall risk17 but not as a predictor of falls.
The aim of this study was to establish if there was a relationship between performance on the AMEDA and SOT tasks and subsequent falls. We hypothesised that poorer performance on these tasks would be associated with a higher risk of falls. A secondary hypothesis was that performance would be worse among individuals who fall in the least challenging circumstances. Where relationships were found, we planned to develop a prediction model complying with the TRIPOD guidelines8 that could be further tested in older adults to identify individuals who might be at greater risk of falls, noting that the relatively small number of participants means that the study should be treated as a pilot of the approach and analytic techniques adopted. A completed TRIPOD checklist for the study is included in the Appendix S1.
2 METHODS
2.1 Design and setting
The study was a prospective cohort study with participants undertaking tests on entry and then monitored for falls for at least 12 months. Volunteers were sought from among community-dwelling adults aged above 60 in the Canberra region. The only exclusion factor was peripheral neuropathy.
2.2 Participants
Fifty-nine people met the inclusion criteria and came in for initial testing between June and November 2019. One person was unable to complete the initial testing and was excluded. A further three participants withdrew during the study; two due to worsening health and one for non-health-related reasons. The remaining 55 participants continued to report falls experience for at least 12 months. Figure S1 shows the CONSORT diagram for the study population. There were 44 female (mean age on entry, 72.9, SD 6.0 years) and 11 male (mean age on entry, 73.8, SD 6.5 years) participants. (See Table S1).
2.3 Ethics
The University of Canberra Committee for Ethics in Human Research approved the study (Approval 2019/1929). Before testing commenced, all participants gave informed written consent.
2.4 Sample size
A target sample size of 66 had been determined based on the requirements for an intervention study that had been planned as part of the project. In the event, the outbreak of the COVID-19 pandemic meant that intervention component of the study did not proceed. The implications of the sample size are discussed further in the Limitations section but point to the need to treat the current study as a pilot.
2.5 Data collection
At the initial testing session, participants provided written informed consent, demographic details and completed a short fall risk questionnaire of seven questions.18 Proprioception was assessed using the AMEDA apparatus16 and the SOT.19 Four other tests not reported in the current study were also undertaken. The full testing regime is described in the Appendix S1.
an event which results in a person coming to rest inadvertently on the ground or floor or other lower level.20
If a participant replied that they had experienced a fall, follow-up contact obtained further details on the circumstances of the fall, including where it had occurred and the activity at the time. The falls data collection process is discussed in more detail in Antcliff et al.21
2.6 Data analysis
R22 was used for all data analysis.
2.6.1 Data preparation
Previous research has drawn attention to differences between types of falls. For example, Kelsey et al.23 report on differences between falls occurring inside and outside. As the factors that might lead to a fall are likely to vary with the type of fall, we adopted a method of classifying falls developed and validated in the context of monitoring falls among people suffering from Parkinson's disease.24 The classification system is quite nuanced in that it takes account of the challenges arising from both the environment and the activity being undertaken (see Figure 1). As an example of a Type 1 fall, where both the environment and activity are challenging, one participant fell while walking backwards carrying a roll of fencing wire. By contrast, a Type 3 fall might be one occurring in the participant's home when undertaking a simple activity such as turning to change direction. A typical Type 2 fall might be a trip when walking on an unfamiliar footpath.
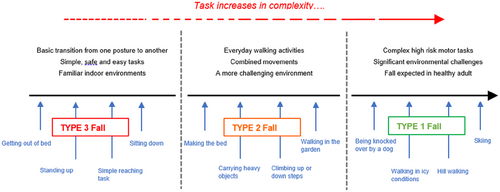
Prior to any analysis, the classification paradigm was applied independently by two of the authors, who were both blinded to the initial test results. A reconciliation process was undertaken for those cases where they had arrived at a different classification, again without any knowledge of the test results.
- the AMEDA score, derived as described in Antcliff et al.16 A score of 1 corresponds to the average performance, with a score of less than 1 indicating poorer performance and, conversely, a score of more than 1 indicating superior performance.
-
the SOT composite score, calculated as:
- the answers to the yes/no questions in the fall risk questionnaire as shown in Table S3.
2.6.2 Missing data
Partway through the initial testing of participants, we discovered that the force plate in the computerised posturography machine used for the SOT was faulty and that the measures that had been taken for the first 27 participants were impacted. The affected participants were all retested within 4 months. However, SOT scores have been found to improve on retesting25 and this was seen to be the case for those not affected by the equipment malfunction. To adjust for this improvement, we used the second reading for those whose initial reading was affected, adjusted down by the average learning effect observed in the unaffected group.
One participant was unable to undertake the SOT test because the harness could not be fastened and another was unable to maintain their balance in the final segment of the SOT test, which precluded the calculation of their composite score. These two participants were excluded from the data used for the t-tests for the SOT composite score. The logistic regression model fitting process restricts the analysis to complete cases and thus these two participants were also excluded from the models that included the composite score. All participants were included in other analyses.
2.6.3 Model selection and validation
Our model selection process was guided by an examination of the relationships between the predictor variables and the relevant outcome variable using t-tests for the two proprioception measures and chi-square tests for the questions in the fall risk questionnaire. For each of the outcome variables, we determined whether a logistic model using the variables found to be associated with an increased risk of falls showed any power to predict those falls. For the purposes of evaluating model performance, we used a likelihood ratio test, three pseudo-R2 measures, balanced accuracy and the area under the curve (AUC). In deciding whether to include an additional predictor variable in the model, we had regard to the Akaike information criterion (AIC).
As we did not have sufficient data to implement a standard cross-validation approach, the models were fit on the entire dataset, but the sensitivity of the results was tested using leave one out cross validation (LOOCV) and bootstrapping, with predictions generated from the fitted model using the ‘predict’ function in R.
3 RESULTS
3.1 Number and classification of falls
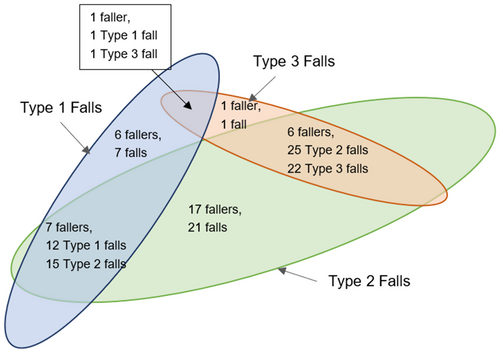
A total of 38 (69%) of the 55 participants who completed at least 12 months in the study experienced at least one fall within their first 12 months after entry into the study (see Figure 2 for the breakdown by fall type), with 105 falls being recorded in total.
3.2 Association between predictor variables and falls occurrence
Table 1 shows the mean and standard deviation of the AMEDA and SOT composite score by falls category together with the effect size and p-value (both unadjusted and adjusted using multiple comparisons using the Benjamini and Hochberg method26) of the variable for each category.
| Measure | No falls | Any fall | Type 2/3 falls | Type 3 falls |
|---|---|---|---|---|
| AMEDA score | ||||
| Mean | 0.920 | 0.859 | 0.845 | 0.755 |
| Standard deviation | 0.082 | 0.145 | 0.146 | 0.106 |
| Effect size | 0.47 | 0.62 | 1.18 | |
| p-Value | .11 | .03 | <.005 | |
| Adjusted p-value | .31 | .15 | .02 | |
| SOT composite score | ||||
| Mean | 73.4 | 71.3 | 70.9 | 68.1 |
| Standard deviation | 4.1 | 6.0 | 6.4 | 8.4 |
| Effect size | 0.39 | 0.44 | 0.85 | |
| p-Value | .19 | .12 | .03 | |
| Adjusted p-value | .31 | .24 | .06 | |
- Note: For the purposes of calculating the effect size (Cohen's d) and p-value, the results for each group are compared in group to those not in that group: that is, ‘Any Fall’ group is compared to those who did not experience a fall; the ‘Type 2/3 Falls’ group is compared to those who either did not fall or had only a Type 1 fall; and the ‘Type 3 Falls’ group is compared to those who either did not fall or had only a Type 1 or Type 2 fall. The adjusted p-value makes a correction for multiple comparisons using the Benjamini and Hochberg method.
Table 2 shows the equivalent information for the questions on the fall risk questionnaire.
| Question | No falls | Any fall | Type 2/3 falls | Type 3 falls |
|---|---|---|---|---|
| Q1. Fell in previous 12 months? | ||||
| Percentage answering yes (%) | 35 | 58 | 62 | 62 |
| Effect size | 0.21 | 0.27 | 0.10 | |
| p-Value | .16 | .06 | .69 | |
| Adjusted p-Value | .31 | .15 | .79 | |
| Q2. Cross street without resting at median strip? | ||||
| Percentage answering yes (%) | 100 | 100 | 100 | 100 |
| Effect size | — | — | — | |
| p-Value | — | — | — | |
| Adjusted p-Value | — | — | — | |
| Q3. Walk 1 km without stopping? | ||||
| Percentage answering yes (%) | 100 | 95 | 97 | 88 |
| Effect size | 0.13 | 0.03 | 0.20 | |
| p-Value | .56 | 1.00 | .27 | |
| Adjusted p-Value | .64 | 1.00 | .43 | |
| Q4. Put socks on while standing on one leg? | ||||
| Percentage answering yes (%) | 53 | 39 | 31 | 0 |
| Effect size | 0.13 | 0.29 | 0.36 | |
| p-Value | .39 | .06 | .02 | |
| Adjusted p-Value | .53 | .15 | .05 | |
| Q5. Admitted to hospital in previous 12 months? | ||||
| Percentage answering yes (%) | 12 | 29 | 28 | 38 |
| Effect size | 0.19 | 0.12 | 0.13 | |
| p-Value | .19 | .53 | .36 | |
| Adjusted p-Value | .31 | .71 | .48 | |
| Q6. Ever had a stroke? | ||||
| Percentage answering yes (%) | 6 | 13 | 12 | 12 |
| Effect size | 0.11 | 0.06 | 0.02 | |
| p-Value | .67 | .69 | 1.00 | |
| Adjusted p-Value | .67 | .79 | 1.00 | |
| Q7. Afraid of falling? | ||||
| Percentage answering yes (%) | 0 | 21 | 19 | 50 |
| Effect size | 0.28 | 0.14 | 0.41 | |
| p-Value | .09 | .46 | .01 | |
| Adjusted p-Value | .31 | .71 | .04 | |
- Note: The effect size is calculated as , where χ2 is the chi-square statistic and n is the number of observations (=55). The p-values have been computed using Monte Carlo simulation with the r function χ2. As with Table 1, the effect size and p-values have been calculated by comparing members of category with those who are not in that category, and the adjusted p-values are corrected for multiple comparisons using the Benjamini and Hochberg method.
3.3 Model development
We discuss each of the three categories in turn. Note that an individual who has experienced falls of different types will appear in each of the relevant categories.
3.3.1 All faller
Thirty-eight people had at least one fall of any type over the 12 months. While on most measures they tended to have slightly worse performance than the group who had not experienced a fall, the differences were not statistically significant, and it was not possible to fit a logistic model with any power to predict falls.
3.3.2 Population with a Type 2 or Type 3 fall
A lower AMEDA score was associated with a higher probability of experiencing a Type 2 or Type 3 fall and had a medium effect size (Cohen's d = 0.618). However, the balanced accuracy for a logistic model with AMEDA score as the independent variable had a balanced accuracy rate of 0.6, misclassifying more than half of those who did not fall. The bootstrapped 95% confidence interval for the AUC is [0.51, 0.81], indicating that the model performed poorly in discriminating between faller and non-faller.
3.3.3 Population with a Type 3 fall
The SOT and AMEDA scores were both associated with Type 3 falls and had large effect sizes (Cohen's d > 0.8), with the AMEDA score having the largest effect size at 1.18. Two of the questions from the fall risk questionnaire—Q4 (Can you put your socks on while standing on one leg?) and Q7 (Do you have a fear of falling?)—both had a moderate effect size (0.3 < w < 0.5) and unadjusted p-values of less than 0.02. None of those who experienced a Type 3 fall could put their socks on while standing on one leg and 50% had a fear of falling compared with less than 10% of those who did not have a Type 3 fall.
We fitted logistic models using the AMEDA score and various combinations of the SOT composite score, Q4 and Q7, to predict the relative risk of falls (see Table S4 for a summary of the model fits). The model including the AMEDA score, Q4 and Q7, had the same Aikaike information criterion (AIC) as the model that also included the SOT composite score and is to be preferred on the grounds of parsimony. Table 3 summarises the fit of the logistic regression model.
| Predictor | β | SE β | Wald's χ2 | df | p | e β |
|---|---|---|---|---|---|---|
| Intercept | 4.232 | 2.970 | 68.861 | |||
| AMEDA score | −7.178 | 3.770 | 3.625 | 1 | .057 | 0.001 |
| Question 4 (Y)* | −18.617 | 3421.992 | 0.000 | 1 | .996 | <0.001 |
| Question 7 (Y) | 1.966 | 1.047 | 3.529 | 1 | .060 | 7.145 |
| Model evaluation | χ 2 | df | p | |||
|---|---|---|---|---|---|---|
| Likelihood ratio test | 18.899 | −3 | .0003 | |||
| Pseudo R2 | ||||||
| McFadden R2 | 0.414 | |||||
| Cox and Snell R2 | 0.291 | |||||
| Nagelkerke R2 | 0.516 | |||||
| Balanced accuracy | ||||||
| In sample | 85% | |||||
| Leave one out cross validation | 78% | |||||
| Area under the curve | ||||||
| In sample | 0.907 | |||||
| Bootstrapped 95% confidence interval | [0.829, 0.984] | |||||
- Note: * Note that the binary variable for Question 4 (Can you put your socks on while standing on one leg?) had the value ‘N’ for all eight participants with a type 3 fall, but also for 23 of those who did not have a type 3 fall. This leads to the p-value of almost 1, suggesting no predictive power. However, inclusion of this variable reduces the AIC and improves the model outcomes. The very large negative co-efficient for this variable means that anyone who can put their socks on while standing on one leg will be predicted to not have a type 3 fall.
4 DISCUSSION
The main hypothesis was supported in that proprioceptive function, as measured by the AMEDA, was significantly associated with Type 2/3 falls and the most significant predictor of Type 3 falls. This is not surprising: a lower AMEDA score indicates poorer ankle proprioception which has been found to be associated with impaired balance10 and Type 3 falls are defined by the absence of any challenges arising from the environment or the activity. That is, they are fundamentally related to poor intrinsic balance. The question from the fall risk questionnaire, eliciting information on balance confirms this; none of those who experienced a Type 3 fall reported being able to put on their socks while standing on one leg. Fear of falling was also clearly important with none of the non-faller having a fear of falling and a noticeably higher percentage of Type 3 faller having a fear of falling relative to the other two fall categories. This is likely to be a two-way relationship, with a fear of falling increasing the risk, and falls themselves leading to a well-founded fear of falling.
Participants reporting Type 3 falls represented only 15% of the cohort and only 20% of those who experienced a fall (see Figure 2). However, they were much more likely to have multiple falls, including Type 1 and Type 2 falls. Of the 30 participants who had either a Type 1 or Type 2 fall, but not a Type 3 fall, 19 had only one fall in total. By contrast, all but one of the participants who had a Type 3 fall had multiple falls. In total, the eight participants with a Type 3 fall accounted for 50 of the 105 falls. Thus, predicting those with an increased risk of Type 3 falls could be expected to identify those who are at greater risk of all types of falls and, given the greater number of falls, an increased likelihood of a fall with adverse consequences.
While we observed lower SOT scores for those with Type 2 and Type 3 falls, the difference was insufficient to achieve significance at the 5% level once an adjustment was made for multiple comparisons, and we found no benefit from including the composite score in the logistic model. The problems with the apparatus which affected the reliability of the initial measurement would also support the exclusion of this variable. A previous study comparing the SOT scores and recalled falls history found an association between a lower composite score and the report of one or more falls in the previous 6 months.27 However, this was a retrospective study, and the SOT measurement was taken after the falls and so may have been affected by the fall rather than being predictive of a fall.
The remaining questions on the fall risk questionnaire operated broadly in the direction that would be expected. For example, those who fell were less likely to be able to walk 1 km without stopping and more likely to have been admitted to hospital than those who did not experience a fall during the 12 months. The differences in absolute numbers were small, however, and not statistically significant.
4.1 Limitations and directions for further research
The size of the sample combined with the relatively low incidence of Type 3 falls meant that it was not feasible to undertake robust cross-validation of the model using training and testing datasets, and the fitted model includes more variables per event than is desirable. Nonetheless, the effect size for each of the variables included was medium to large, and the likelihood ratio test for the model was significant (χ2 = 18.9, p-value <.001). Using the Nagelkerke R2 of 0.29 found in the analysis and the recommended shrinkage factor of 0.9, equation 11 for sample size given in Riley et al.28 produces an estimate of a minimum sample of 89 for a multivariate logistic regression model with three predictor variables. Until a larger study can be done, the results presented here should be treated as indicative rather than definitive, but our work is the first to provide a basis for establishing the parameters for such a study.
Having demonstrated that the AMEDA score is predictive of Type 3 falls, it will be possible to use it for future intervention studies that test the effects of fall intervention programs. This study suggests that focussing on programs that improve the ability to stand securely on one leg may be a good place to start.
The AMEDA testing process took between 5 and 10 min. While this is shorter than an average eye test, it could be a deterrent for adoption in a clinical setting. Refinements to the apparatus that allows for implementation of a more sophisticated testing regime, which could reduce the test duration, have the potential to streamline research and facilitate clinical use.
5 CONCLUSIONS
The falls classification used here provides a more nuanced understanding of falls and how their characteristics and the factors driving them might vary. While all types of falls can be potentially catastrophic, Type 3 falls are likely to be of most concern given the likelihood that a person experiencing a Type 3 fall will have multiple falls. The ability to put on one's socks while standing on one leg appears to protect against a Type 3 fall, with none of those who were able to do this suffering a Type 3 fall during the period they were monitored. However, over half of the participants were unable to meet this benchmark and most did not have a Type 3 fall. The additional information from the AMEDA score and the question regarding fear of falling allowed the fitted logistic model to achieve high sensitivity and specificity in predicting Type 3 falls in the study population. We found that poorer performance on the AMEDA was the most significant predictor of a Type 3 fall in the following 12 months, while a fear of falling, probably justified, was far more common among those experiencing a Type 3 fall than among other participants.
This study points to the potential to use the AMEDA both in future research into falls mitigation and in a clinical setting to diagnose and measure the rehabilitative effects of interventions.
6 ACKNOWLEDGEMENTS
The authors would like to acknowledge the commitment of those who participated in the study and reported daily on their falls experience for at least a year. Open access publishing facilitated by University of Canberra, as part of the Wiley - University of Canberra agreement via the Council of Australian University Librarians.
CONFLICT OF INTEREST STATEMENT
No conflicts of interest declared.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author [SA], subject to undertakings regarding its use in order to protect participant privacy. The R code which produces the tables and figures included in the manuscript is also available on request from the corresponding author.