Systematic review of symptom-level networks of alcohol use disorder
Funding information: The study was funded by a PhD project grant from the Center for Urban Mental Health, a research priority area of the University of Amsterdam.
Abstract
Background and aims
Network analysis is being used increasingly to study disorders such as alcohol use disorder (AUD) at the level of interacting symptoms. However, it remains unclear what insights AUD symptom networks have brought so far. Therefore, this pre-registered systematic review, following PRISMA reporting guidelines, aimed to collate and critically assess the literature on published AUD symptom networks.
Methods
1608 unique articles were collected from PsycINFO, Medline, Embase and Web of Science between January 2010 and May 2023. A total of six articles were included in the review, comprising seven unique cross-sectional networks. The general characteristics of the symptom networks are summarized (i.e. edge inclusion, whether the connection between nodes is present or absent; and node centrality, the importance of a node within an estimated network) and compared between population versus clinical samples.
Results
The networks included many edges, with densities ranging from 60% to 100% (mean and mode of 80%, standard deviation of 28%). The edge connecting Tolerance and Time Spent consuming alcohol was most consistently present across samples, while edges connecting to Physical/Psychological Problems were consistently connected only in population samples. Consuming Larger/Longer than intended, and Physical/Psychological Problems had highest strength centrality, while failure to Cut Down and Hazardous Use were consistently lowest.
Conclusions
Alcohol use disorder symptom networks tend to be densely interconnected and characterized by a high proportion of included edges (dependencies between variables). Some edges are more consistently found in population samples than in clinical samples and vice versa.
INTRODUCTION
Alcohol use disorder (AUD) is one of the most prevalent yet consistently undertreated mental health conditions [1, 2]. Individuals struggling with AUD find it challenging to manage their alcohol use despite its negative impact on their physical and mental wellbeing, as well as that on their close social network [2, 3]. Under the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), AUD is described as a problematic pattern of alcohol use leading to clinically significant impairment or distress, as manifested by at least two symptoms, occurring within a 12-month period, as outlined in Table 1.
| Meeting two to three symptoms is indicative of a mild AUD, four to five symptoms of a moderate AUD and six or more symptoms of a severe disorder |
| 1. Larger/Longer (LL): Drinking more or longer than intended |
| 2. Cut Down (CD): Unsuccessful efforts to cut down or control use |
| 3. Time Spent (TS): Significant time spent on alcohol-related activities |
| 4. Craving (CR): Strong desire or urge to drink |
| 5. Failure to Fulfill (FF): Failing to meet major life obligations |
| 6. Social/Interpersonal Problems (SI): Alcohol-related social or relationship problems |
| 7. Give Up (GU): Giving up important activities because of alcohol |
| 8. Hazardous Use (HU): Drinking in physically risky situations |
| 9. Physical/Psychological Problems (PP): Continued use despite physical or mental health issues |
| 10. Tolerance (TL): Needing more alcohol for the same effect |
| 11. Withdrawal (WD): Experiencing withdrawal symptoms when not drinking |
The complexity of studying and treating addictive behavior stems from the intricate nature of the disorder. Similar to other mental health conditions, AUD is thought to arise from the dynamic interplay of multiple interacting factors that span multiple social, psychological and biological dimensions [4, 5]. Acknowledging and modeling the complexity of the onset, progression and persistence of AUD [4, 6, 7] meets the need for approaches that go beyond traditional diagnostic outcomes or composite scores, which often average symptom severity. Symptom networks provide a more granular lens for understanding the disorder by analyzing specific symptoms and their interconnections [8]. This is particularly relevant because individuals with the same diagnosis frequently experience diverse symptom patterns, making diagnoses an insufficient descriptor of their disorder. Finally, examining symptom networks over time would give unique insights into the dynamics of AUD, shedding light on how symptoms interact and evolve, and providing a deeper understanding of the underlying mechanisms and heterogeneity of AUD. Hence, the network approach holds the potential to unravel the complexity of AUD and advance knowledge beyond conventional diagnostic frameworks. The field of psychology has witnessed a proliferation of articles employing network analysis to examine disorders at the level of interacting symptoms [9]. In this approach, disorders are visualized as networks in which symptoms are represented as nodes, whereas their conditional dependencies are shown as lines/edges between them (for more information, see Box 1). General reviews in the network literature have provided broad summaries of findings across disorders and evaluated methodological considerations and limitations [9-11]. More recent reviews have concentrated on specific disorders, for example, major depressive disorder [12, 13] and eating disorders [14, 15], yet reviews on AUD symptom networks are notably absent. Our initial search indicated that AUD symptom networks have been applied across diverse populations, with varying sample sizes, research questions, subgroups, and modeling and analytical techniques [6, 7, 16], but the direct implications of these studies are yet to be explored.
Box 1. Explanation of psychological networks and their key features
The network approach conceptualizes psychological phenomena as arising from the direct causal interactions of the symptoms themselves [17]. Statistically, the network approach describes multivariate data by finding pairwise dependencies between observed variables, such as items on a questionnaire. Any non-zero dependency is represented by an edge. Edge strength or weight relates to the parameter estimate for the pairwise dependency and can be positive or negative. Edges connect the observed variables, known as nodes. When the nodes represent clinically validated symptoms (e.g. based on the criteria in the DSM-5), this is called a symptom network. Such symptom networks have been studied in many different disorders, including AUD [6, 7, 18, 19].
So far, most network analyses have been conducted on cross-sectional data (i.e. all cases in the data set are independent). In that case, the network analysis can produce one group-level network, where conditional dependencies are driven by individual differences [20]. The edges in these networks do not point in any direction (i.e. undirected). However, networks based on longitudinal data can produce three different networks: temporal, contemporaneous and between-person networks [20]. Here, ideographic networks can be estimated, which may not match the group-level networks [20]. Moreover, the edges in the temporal networks point in the direction of one node to the next (i.e. directed).
Many metrics can describe, interpret and compare symptom networks. Globally, network density – defined as the proportion of estimated edges relative to all possible edges – indicates whether a network is dense (many edges) or sparse (few edges). This distinction informs resilience research [17, 21] and affects estimation procedures like regularization [20].
Locally, centrality measures the connectedness or influence of a node on others. Node strength, the sum of absolute edge weights connected to a node, is often used to rank node importance in networks. Other centrality measures, such as closeness and betweenness, are more problematic for psychological networks [20]. For further details, see [22, 23].
In light of this research gap and the expanding use of the network approach in AUD research, this review aimed to collate and critically assess the literature on AUD symptom networks. Adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [24] guidelines, which were pre-registered (PROSPERO database: CRD42023439148), we systematically reviewed the literature on networks assessing AUD symptoms. The primary objective is to discern consistent patterns in AUD symptomatology obtained from the network approach and how those findings align with the wider AUD literature. We investigated two main research questions. First, what characterizes AUD symptom networks, particularly symptom connectivity (e.g. based on node centrality and edge strength)? Second, how do AUD symptom networks vary when considering clinical or population samples? We qualitatively synthesized data from the identified studies, emphasizing the disparities between clinical and population-based samples to answer these questions.
METHODS
The pre-registered PRISMA protocol [25] can be found on the Open Science Framework (OSF) (https://osf.io/um3w4/). The PROSPERO pre-registration can be found with registration ID CRD42023439148 in the PROSPERO database at https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023439148. Moreover, all details about this project, including search strategy, analysis code, (individual network) results, plots and online supporting information are available at https://osf.io/um3w4/. Data were visualized using R [26]; in particular, the R packages ggplot2 [27], tidyverse [28] and qgraph [29] were used for data wrangling and the visualization of our findings.
Search protocol and eligibility
The search was conducted with a librarian's help in May 2023. The following databases were searched: EMBASE, MEDLINE, PsycINFO and Web of Science Core Collection. The search dates range from January 2010 to May 2023 and only included peer-reviewed articles published in English. The cut-off of January 2010 was implemented as the network approach in psychology was not used before then [9, 30]. The search terms were focused on AUD and psychometric network analysis.
Two independent raters screened the titles and abstracts of the studies, and decisions were recorded in Rayyan [31]. Studies were included if they conducted a psychometric network analysis of AUD symptoms. These networks could be cross-sectional and longitudinal in nature. Each node had to represent a validated AUD diagnostic symptom based on DSM-IV, DSM-5, International Classification of Diseases 10th Revision (ICD-10) or ICD-11 [32-34] criteria and could not represent any other psychological conditions or variables.
When eligibility was unclear, the article was selected for full-text screening, following the same inclusion criteria. In case of disagreements between two raters, the whole project team assessed the article and agreed through discussion. Before any formal screening, the screening guideline was piloted on 10 studies. Upon finalizing the screening guideline, it was uploaded on OSF.
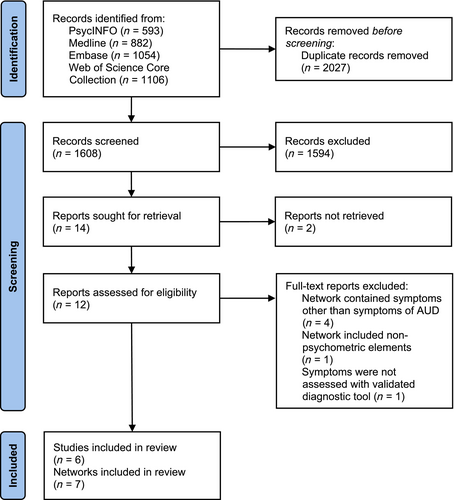
Figure 1 presents the PRISMA flow diagram, including the search, screening and final selection of results.
Quality assessment
Owing to the recent rise of the network approach, quality assessment tools for studies employing network models are not yet established. Therefore, we chose to adapt recently published guidelines for reporting cross-sectional network analyses in the field [23]. These guidelines were developed to improve transparency and replicability and make psychological network studies more rigorous. We adapted these guidelines, by creating a checklist of features that a network study should minimally report on (i.e. quality assessment criteria), which we used in this review. 1 One reviewer extracted the quality assessment criteria, while a second reviewer independently verified the extracted data. Any discrepancies were reconciled through discussion among the research team members. For details on the quality assessment scoring, please see Appendix S2. The selected studies are summarized in Table 2 and the quality assessment results are summarized in Table 3 (see quality assessment results for individual networks in the ExtractedResults folder on OSF, at https://osf.io/um3w4/).
| Study | Sample characteristics | AUD symptoms | Network analysis | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Size | Type | Age M (SD) | Female % | Data source | Assessment | Diagnostic manual | n symptoms | Severity | Time frame | Model | Network density1 | Centrality analysis | CS coefficient | Edge accuracy | |
| Hoffman et al. (2018) | 34 629 | Pop. | 49.08 (17.29) | 56.44 | NESARC Wave 2 | AUDADIS-IV | DSM-IV | 11 | ≥1 drinka,e | C | Isingd | – | Str., clo., bet. | – | – |
| 34 712 | Pop. | 46.85 (16.95) | 57.98 | NESARC-III | AUDADIS 5 | DSM-5 | 11 | ≥1 drinka,e | C | Isingd | – | Str., clo., bet. | – | – | |
| Hoffman et al. (2019) | 22 160 | Pop. | 45.88 (15.89) | 53.14 | NESARC Wave 2 | AUDADIS-IV | DSM-IV | 11 | ≥1 drinka | C | Isingd | 85.45% | Str., clo., bet. | – | 95% CI |
| 24 773 | Pop. | 44.40 (16.03) | 53.43 | NESARC-III | AUDADIS 5 | DSM-5 | 11 | ≥1 drinka | C | Isingd | 87.27% | Str., clo., bet. | – | 95% CI | |
| Rutten et al. (2021) | 6125 | Clin. | 45.4 (13.1) | 26.7 | Addiction treatment center | MATE, OCDSh | DSM-IV | 11 | Average lifetime use: 16.2 (SD = 12.5) yi | C | Ising (EBIC, y = 0.5) | 69.10% | Str. | 0.75 | BDT |
| Conlin et al. (2022) | 17 360 | Pop. | 45.96 (17.36) | – | NESARC Wave 1 | AUDADIS-IV | DSM-5 | 10 | ≥12 drinkse | C | Isingb | 84.44% | Str., clo., bet. | 0.672 | SEc |
| 17 360 | Pop. | 49.06 (17.30) | – | NESARC Wave 2 | AUDADIS-IV | DSM-5 | 10 | ≥12 drinkse | C | Isingb | – | Str., clo., bet. | 0.75 | SEc | |
| 17 360 | Pop. | – | – | NESARC waves 1 & 2 | AUDADIS-IV | DSM-5 | 10 | ≥12 drinkse | L | Binary autoregressive | – | Instr., outstr., clo., bet. | – | – | |
| Huth et al. (2022) | 23 591 | Pop. | f | 48 | NSDUH | NSDUH questionnaire | DSM-5 | 6 | Drinking ≥6 occasionsa,g | C | Ising (Bayesian) | 100% | Str. | 95% HDI | 95% HDI |
| 483 | Clin. | 38.65 (10.35) | 25 | AHEAD | CIDI-SF | DSM-5 | 6 | Symptom prevalence rates: 64%–90% | C | Ising (Bayesian) | 60% | Str. | 95% HDI | 95% HDI | |
| Gauld et al. (2023) | 787 | Clin. | 40.3 (11.6) | 27.7 | ADDICTAQUI | MINI | DSM-5 | 11 |
93% SUDk, ≥2 drinks/weeka |
C | Ising (EBIC, y = 0.5) | 70.91% | Str., clo., bet., E.I. | 0.67 | – |
- Note: Overview of the six studies included in this review. Information on the seven networks included in data aggregation are printed in bold. As some studies reported on multiple networks based on different study populations, multiple rows per study may be shown.
- Abbreviations: ADDICTAQUI, Addiction Aquitaine Cohort; AHEAD, Addiction Health Evaluation and Disease; AUD, alcohol use disorder; AUDADIS, Alcohol Use Disorder and Associated Disabilities Interview Schedule; AUDIT, Alcohol Use Disorder Identification Test; BDT, bootstrapped difference test; Bet, betweenness; C, cross-sectional; Clin., clinical; CI, confidence interval; CIDI-SF, Composite International Diagnostic Interview – Short Form; Clo., closeness; CS, correlation stability; DSM, Diagnostic and Statistical Manual of Mental Disorders; EBIC, Extended Bayesian Information Criterion; E.I., expected influence; GGM, Gaussian graphical model; HDI, highest density interval; Instr., instrength; L, longitudinal; MATE, Measurements in the Addictions for Triage and Evaluation; MINI, Mini International Neuropsychiatric Interview; NESARC, National Epidemiological Survey on Alcohol and Related Conditions; NSDUH, National Survey of Drug Use and Health; OCDS, Obsessive Compulsive Drinking Scale; Outstr., outstrength; P, population; SE, standard error; Str., strength; SUD, substance use disorder.
- 1 Only calculated and/or reported for studies/samples that were used for across study analyses in this review.
- a In the past 12 months.
- b Similar to Ising model, see study for details. Models with and without tuning parameter were highly similar.
- c Standard errors of edge weights reported in the supporting information.
- d Missing gamma (γ) parameter.
- e Per wave, there were four networks estimated based on low and high thresholds of the Cut Down and Craving symptoms. Low threshold means meeting the milder statement of the criterion; high threshold means meeting the more extreme statement. The sample remained the same across these manipulations, and therefore, only the details of the two waves are reported. See article for details.
- f Percentages only reported for particular age ranges: 18–25 years, 51.31%; 26–34 years, 15.57%; 35–49 years, 20.71%; >50 years, 12.42%.
- g 50% of the sample reported no AUD symptoms at all, 27% indicated at least two symptoms to be present (indicative of mild AUD) and 6.5% reported >4 symptoms (indicative of moderate AUD).
- h Craving assessed with OCDS survey. See article for details.
- i DSM-IV total score M (SD) = 6.39 (2.64).
- k This included several substance use disorders (i.e., not only AUD).
| Quality assessment | |||
|---|---|---|---|
| Study | Sample and reporting | Analysis | Open science practices |
| Hoffman et al. (2018) | High | Low | Low |
| Hoffman et al. (2019) | Moderate | Low | Low |
| Rutten et al. (2021) | High | High | Low |
| Conlin et al. (2022) | Low | High | Low |
| Huth et al. (2022) | High | High | High |
| Gauld et al. (2023) | High | Moderate | Low |
Extraction of network study characteristics
The data collected included general information about the articles, the samples used and the network analyses performed. An initial test of the data extraction process was conducted on three pre-selected studies. Data were primarily extracted by one reviewer and verified by a second; discrepancies were discussed and resolved with the team.
Aggregation across studies
All study data were aggregated and compared by focusing on two key features of networks: edge presence (i.e. the partial association between two nodes estimated to be significantly different from zero) and node strength (i.e. a centrality metric that calculates the absolute sum of the partial associations connecting to a particular node). We would ideally have the edge parameters or the raw data available. Unfortunately, this information was not available to us for all studies. As such, we solely worked with the presence and absence of edges.
We chose to exclude some data from the included studies, for several specific reasons outlined as follows. Data from Hoffman et al. [16] were excluded as they chose different node thresholds. Only the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Wave 1 network from Conlin et al. [6] was used, avoiding the Wave 2 network for its significant overlap with Hoffman et al. [18] and lack of the node Craving. The unique longitudinal network [6] was excluded because of a lack of comparability with the rest of the studies. Only the ‘past-year drinkers’ subsamples from Hoffman et al. [18] were selected for consistency with population network studies. The node names from the Huth et al. [7] study were adjusted for better alignment with the original terms described in DSM-5 (see document Node_names on OSF). The Legal node in Rutten et al. [35] was excluded as it is no longer listed in DSM-5 and was seldom assessed. Taken together, seven cross-sectional networks from five studies were summarized, comprising three networks from clinical samples and four networks from general populations.
To investigate edge presence, we tallied the number of times an edge was included across the networks. This had to be done by visual inspection for most studies [6, 7, 19, 35], as no (regularized) association matrix was provided. To ensure some robustness, we only included regularized or Bayesian analyzed networks. As a further measure of robustness, we only discuss edges that were always present and estimated at least six times.
To investigate node strength across networks, we ranked the node strengths in each study based on visual inspection of the standardized centrality plots, except in Rutten et al. [35], where the standardized scores were provided. When two nodes were ranked identically, the next node's ranking was increased by two units. Each ranking was decreased by one unit and divided by the total number of nodes in that network minus one (i.e. min–max normalized).
RESULTS
Search
The initial search across various databases yielded 3635 results, 1900 of which had unique identifiers. After duplicates were removed, 1608 articles remained for screening.
Based on the abstract and following the exclusion criteria, 1594 articles were excluded (for a flow diagram with details of the selection procedure, see Figure 1). Full-text screening was undertaken for the remaining 14 articles. There was one inclusion discrepancy between screeners, which on second full-text inspection turned out to clearly fit the exclusion criterion of ‘not AUD-exclusive’. The final sample consisted of six studies, totaling 23 networks, which were not necessarily unique in time nor sample; the seven unique networks that were included for the data aggregation are summarized in Table 2.
Network study characteristics
Sample characteristics
An overview of the sample characteristics, network estimation and stability analyses of the included studies is provided in Table 2. Details for each study can be found in the supporting information (Appendices S1 and S2 and Tables S1 and S2). The quality assessment for each study can be found in Table 3, and details on the scoring are shared in Appendix S2 and on the OSF page.
Summary of individual studies
The two first papers published by Hoffman et al. examined cross-sectional network models of AUD symptoms using data from NESARC Wave 2 and NESARC-III [16, 18]. The first study [16] aimed to investigate the impact of different symptom thresholds on the network structure of 11 AUD symptoms. The AUD criteria for Craving and Cut Down are composed of two sub-items, where endorsement of either one meets the criterion. These sub-items differ in severity, so the authors analyzed how varying severity thresholds affected the networks. A ‘low threshold’ meant a symptom was endorsed with the low severity sub-item, whereas a ‘high threshold’ meant that endorsement required the high severity sub-item. The results showed that different thresholds for Craving or Cut Down affected the network edges. Low threshold nodes had stronger connections to highly endorsed nodes, whereas high threshold nodes had stronger connections to less endorsed nodes. Centrality metrics did not significantly change across different thresholds. The authors emphasized that diversity in diagnostic tools, such as varying thresholds, can impact reproducibility and generalizability.
The second [18] study explored four different filters for population selection from the NESARC data: the full sample, past-year drinkers, past-year binge drinkers and participants with at least one AUD symptom. The proportions of asymptomatic individuals significantly influenced network relationships. The full sample had more positive connections, whereas more stringent criteria led to absent or negative edges. Centrality estimates also varied, with Larger/Longer being central in broader samples and Give Up being central in symptomatic networks. The authors suggested that including many non-drinking individuals may inflate relationships between symptoms in symptomatic individuals.
In 2021, Rutten et al. [35] conducted a cross-sectional network analysis on Dutch patients with substance use disorder in early treatment. This study included various substances such as alcohol, cannabis, cocaine, stimulants and opioids. The main aim was to compare network models for different substances and between DSM-IV and DSM-5 criteria, using structured clinical interviews. For AUD, the network showed the strongest centrality for Time Spent, Physical/Psychological Problems and Failure to Fulfill, and the weakest centrality for Legal Problems, Hazardous Use and Give Up. The strongest edge was between Give Up and Failure to Fulfill.
In 2022, Conlin et al. [6] utilized NESARC data from waves 1 and 2 to assess agreement between cross-sectional and longitudinal networks over a 3-year lag. High agreement was found between cross-sectional networks, but low agreement was observed between cross-sectional and longitudinal networks, although it was higher than expected by chance. The study indicated that cross-sectional networks might not capture dynamic changes in AUD well. Larger/Longer and Physical/Psychological Problems were the most central nodes, whereas Tolerance and Hazardous Use were the least central. In the longitudinal network, Social/Interpersonal Problems predicted Give Up, suggesting more advanced AUD symptoms.
In 2022, Huth et al. [7] compared AUD networks in general and clinical populations, using data from different interviews and criteria. For comparability, six variables resembling DSM criteria were chosen. In the general population, Time Spent had the highest centrality, whereas Cut Down (called Loss of Control in the study) had the lowest. In the clinical sample, Larger/Longer (called Loss of Control in the study) was highest, and Hazardous Use was lowest. The clinical network was sparser, with many ambiguous edges. Sociodemographic factors such as age, gender, ethnicity and income showed significant differences in network structures, with the most variation found between different age groups.
In 2023, Gauld et al. [19] examined substance use symptom networks in a French clinical population, focusing on the centrality of Craving. Data from participants seeking outpatient addiction treatment from 2009 to 2019 were used. Craving was the most central node, followed by Give Up and Withdrawal, with Hazardous Use being the least central. Strong edges were found between Craving and Withdrawal, and between Give Up and both Withdrawal and Failure to Fulfill.
Across studies
Edge links
Across all networks, all edges present were positive. The networks included many edges, with densities ranging from 60% to 100% (mean and mode of 80%, standard deviation of 28%). See Table S2 for the edge inclusion proportion for all reviewed edges.
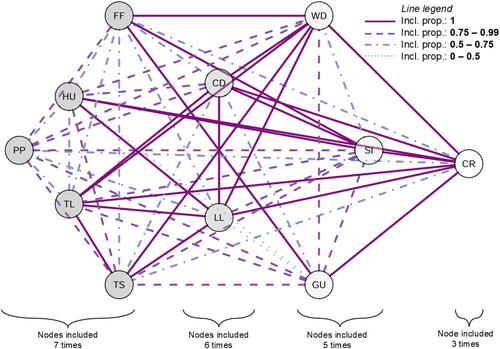
All networks
Upon aggregating the findings from all studies, the only edge consistently identified seven out of seven times was between Tolerance and Time Spent (Figure 2). Edges between Larger/Longer Time Spent, Larger/Longer Tolerance and Larger/Longer Hazardous Use were maximally present six times. For a contrasting figure showing all edges, see Figure S3.
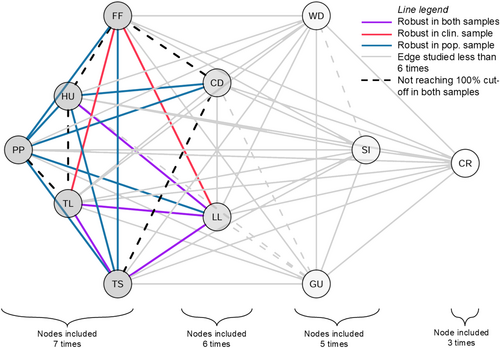
Edges in population versus clinical networks
As presented above, the association between Time Spent and Tolerance was consistently observed across all clinical and population samples (totaling seven instances). For separate edge inclusion proportions in population and clinical samples, see Figures S1 and S2 and Table S2. Visual inspection of the uniquely maximally included edges in the population versus clinical samples (i.e. blue versus red edges in Figure 3) indicated a denser network in the population sample: eight edges were uniquely maximally included in the population sample, compared with two in the clinical sample. For example, connections between Cut Down and Physical/Psychological Problems, as well as between Cut Down and Hazardous Use, were consistently found in population networks, whereas they were found less than 50% of the time in clinical networks. In contrast, the most consistent connections across the three clinical studies, present less than 50% of the time in population networks, were between Tolerance and Failure to Fulfill, as well as between Larger/Longer and Failure to Fulfill. These findings suggest that the robustness of particular conditional dependencies may vary depending on the sample type. For a network contrasting population and clinical samples with a more lenient cut-off of edges being present more or less than 50% of the time, see Figure S4.
Centrality
The correlation stability (CS) coefficient of the centrality estimates was sufficient in all cases, according to currently accepted guidelines [36]. Figure 4 displays the relative ranked node strength centrality in seven networks taken from five studies.
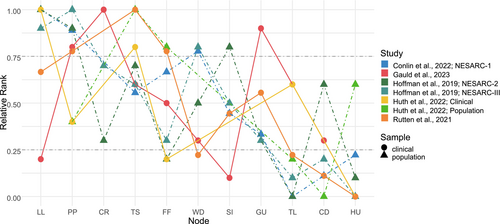
All networks
Aggregated findings from all studies suggest that Physical/Psychological Problems was identified with high centrality in five of the seven networks analyzed. This was closely followed by the symptom node Larger/Longer, which emerged as highly central in four of the seven networks. Furthermore, Hazardous Use was found to have low centrality in six of the seven studies, with Tolerance and Cut Down following this trend in five and four of the seven studies, respectively.
Node strength in population versus clinical networks
A noticeable difference between the two samples is that in the population sample, Tolerance consistently falls into the lowest centrality rating (i.e. <0.25), whereas it ranked low and moderately in the clinical sample (i.e. around 0.5). This indicates that Tolerance may have a different or potentially more prominent role in the symptom network of clinical populations, compared with the general population. In the case of Craving and Give Up, only one clinical sample showed high centrality (both from the study by Gauld et al. [19]), whereas the population samples ranked neither high nor low. Conversely, Withdrawal was highly central in two population samples, whereas it was ranked moderately or low in the clinical samples.
DISCUSSION
This review qualitatively summarizes the first generation of AUD network studies to describe the characteristics of AUD symptom networks and whether there are differences between networks derived from clinical and population-based samples.
Our study observed that the AUD symptom networks tended to be dense, characterized by a high proportion of included edges (i.e. with non-zero connections between nodes). These edges were consistently found across studies, with many being included as frequently as they were tested. Certain patterns emerged consistently across studies regarding node strength (i.e. relative importance of the symptom in the network), with some nodes showing high relative strength (e.g. Larger/Longer and Physical/Psychological Problems) and others demonstrating low strength (e.g. Hazardous Use, Cut Down and Tolerance). Conversely, the relative strength of some nodes, such as Craving, Failure to Fulfill, Give Up, Social/Interpersonal Problems and Withdrawal, varied more considerably.
The finding that Physical/Psychological Problems exhibited high centrality in five out of seven networks aligns with the general characterization of AUD in DSM-5: a condition marked by clinically significant physical and/or psychological impairment or distress associated with alcohol use. The high centrality of using Larger/Longer is also consistent with major etiological models of addictive disorders. For example, the Impaired Response Inhibition and Salience Attribution (iRISA) model by Goldstein and Volkow [37] emphasizes the loss of control over substance use, resulting in more intake or longer use than planned, represented by the Larger/Longer symptom. However, because of the cross-sectional nature of the reviewed networks, the current results cannot comment on any temporal interactions between symptoms (see further discussion below).
In contrast, Hazardous Use exhibited the lowest centrality across studies, suggesting that engaging in physically hazardous alcohol use, such as drunk driving, is not a central aspect of AUD. This could be attributed to the specificity of this criterion, as it represents a particular example of negative consequences. This interpretation is supported by a study that found six criteria (Tolerance, Time Spent, Give Up, Failure to Fulfill, Craving and Social/Interpersonal Problems), with a diagnostic threshold of two, were optimal for AUD diagnostics in the NESARC sample, thus excluding Hazardous Use [38, 39]. Further, earlier studies have also indicated the problematic and poor psychometric performance of Hazardous Use as a diagnostic criterion for AUD [40].
Characteristics of AUD symptom networks in subgroups
In our analysis of AUD symptom networks, certain edges were more consistently found in population samples than in clinical samples and vice versa. A notable exception is the edge linking Time Spent and Tolerance, which was present in all seven networks. Edges were consistently connected to Physical/Psychological Problems in population samples, which might indicate that these issues are linked to AUD criteria at an earlier stage of the disorder. In more severe AUD cases, such linkage to problematic alcohol use appears less consistent, which could also be partly attributed to lower variance in this symptom in clinical samples, where a high number of clinical symptoms is prevalent across the sample.
Centrality, or importance of the symptom, also varied between clinical and population samples. Tolerance exhibited low centrality in the population sample, but moderate centrality in the clinical samples. This is logical from a clinical perspective, as higher and more persistent alcohol use, such as continuous drinking without abstinent days, will result in tolerance, whereas a less severe drinking pattern – as more prevalent in population samples – will be related to lower tolerance.
The centrality of Give Up varied significantly, with only one clinical sample showing high centrality, whereas population samples showed neither high nor low centralities. This difference between groups could reflect the fact that a recognition of having given up important activities because of drinking needs to be present to endorse this symptom, and this acknowledgement may be higher in clinical samples, where the realization of these problems may be more explicit. Surprisingly, Craving had high centrality in only one of the three studies. Despite its addition to DSM-5 in 2013 and its role in models predicting AUD stability [41, 42], only the study by Gauld et al. [19], conducted in a clinical setting, confirmed the high relative importance of Craving in AUD.
Clinical utility of established AUD symptom networks
Although still evolving, the established AUD symptom network studies present several promising avenues for research and treatment. The first notable contribution of this work lies in elucidating the relative importance of different symptoms. In our review, Larger/Longer and Physical/Psychological Problems emerged as central nodes across studies, underscoring their potential as focal points in clinical intervention. Yet, it is important to note that interpreting centrality metrics is increasingly recognized as a complex task [22].
Another contribution of the current work is the comparison between population and clinical samples. By examining similarities and differences among these groups, and within subpopulations (e.g. [7]), researchers and clinicians can gain insights into common and unique AUD mechanisms. Differences in networks might suggest pre-clinical symptoms or vulnerabilities for AUD, or they may reveal distinct states of health and disorder. However, it is crucial to consider that these group differences might also stem from methodological issues, such as biases in sample selection [18, 43] and the approach to measuring symptoms (e.g. via self-report or clinical interview). For example, a professional diagnosis is thought to offer a more reliable assessment of the clinically significant challenges faced by individuals with addiction compared with self-reported questionnaires, which can sometimes be influenced by varying levels of self-awareness or shame to endorse problems with drinking. Lastly, the first steps have been made in describing AUD symptom dynamics, including its onset and maintenance. This aspect, mentioned in several of the reviewed articles [6, 19, 35], becomes particularly salient in studies like those of Conlin et al. [6], which uniquely considered temporal factors. More work is needed to learn how AUD symptoms change over time.
Limitations of the study
This review was pre-registered and adhered to PRISMA reporting standards. Nonetheless, it is important to acknowledge several limitations, some of which stem from the limited available literature. One limitation is the inconsistency in the number of nodes across the included networks. For instance, the study by Huth et al. [7] included only six nodes, whereas the studies by Gauld et al. [19], Hoffman et al. [18] and Rutten et al. [35] each featured 11 nodes. The number and selection of nodes are known to significantly impact the network structure [44, 45]. Moreover, because of the limited data available, we solely worked with the presence and absence of edge parameters as a first step in reviewing the currently available research. Regarding the aggregation of findings, there was inherent subjectivity, especially in defining what constituted a ‘robust edge’. We introduced cut-offs when discussing centrality and edge inclusion findings to identify consistent patterns and improve the readability.
These cut-offs, although useful, were somewhat arbitrary and potentially overly restrictive. Therefore, we also included an edge-contrast network, where both 100% and 50% cut-offs were considered, which revealed very similar results. However, it is crucial to note that edge inclusion was based on regularized networks reported in the included studies, which have their own statistical limitations (as noted by Huth et al. [46] and Williams et al. [47]), including the fact that there was no evidence provided for edge absence in most of the reviewed studies.
Additionally, in providing an aggregated summary of centrality, we ranked the nodes, thereby omitting the distances between them. Currently, there is no established method for qualitatively aggregating network findings. Our approach, therefore, should be considered a preliminary step. As data- and analysis-sharing practices improve, we anticipate the development of more sophisticated methods for summarizing and interpreting these findings. More generally, to enhance the clinical relevance and overall quality of AUD symptom network studies, we propose focusing on at least five key areas of improvement.
Future directions and perspectives
Estimate longitudinal networks
The data reviewed in this study focus on symptoms within a single year, assessed at the group level using structured interviews or questionnaires. Mostly, this was a one-off assessment. Only the study by Conlin et al. [6] included multiple assessments, but its unique longitudinal network [6] was excluded from the data aggregation for a lack of comparability with the rest of the studies. Cross-sectional network models capture between-group effects at one time point, which do not allow for exploring dynamic symptom interactions over time nor necessarily align with within-person changes [6, 48]. For treatment improvement in AUD, personal-level network models, or idiographic models, are needed. These models require frequent, repeated measurements over a longer period of time. Exploring temporal dynamics is possible through panel modeling, multi-level vector autoregressive (VAR) modeling and idiographic modeling [49], which can detect within-person changes. However, longitudinal modeling faces challenges. Reliable detection of within-person effects, already in small networks, requires extensive data [50] and can be burdensome for participants. The application of these models in treatment strategies is currently being explored. Despite these drawbacks, longitudinal network modeling will help the field forward in allowing for the inference of the directionality of network edges and a better understanding of AUD network dynamics at the individual level.
Choice of sample
The quality of a network model is highly dependent on the sample composition used to assess the network, which significantly influences the implications drawn from the model (for a detailed discussion, see Hoffman et al. [16, 18]). Clinical samples, typically composed of individuals with specific disorders, differ markedly from general populations that predominantly consist of healthy individuals without clinical conditions. In clinical samples, higher levels of symptom endorsement are common, whereas individuals in population samples usually endorse few or no symptoms, all of which is reflected in the network structures: population samples often reveal edges indicating agreement with the non-endorsement of symptoms, whereas clinical samples show edges resulting from symptom endorsement. Hence, the underlying mechanisms driving these network relationships may be substantially different. Problems in estimation are exacerbated when individuals with clinical conditions are drawn from population samples using sum score cut-offs. This approach can lead to biased estimates of network edges through Berkson's bias [43], introducing weak and negative edges and producing misleading networks.
Hence, the interpretation of networks should be contextualized within the specific group (clinical or non-clinical) and stage of the disorder (prevention, intervention, relapse prevention) from which the data were collected. For studies focusing on clinical samples, obtaining a diagnosis established by a clinician is essential, rather than relying on samples based solely on sum score cut-offs. More extensive reporting on comorbidities may also provide valuable insights (see the ‘quality assessment’ suggestions below).
Choice of nodes
For accurate clinical inferences of symptom importance in AUD, it is imperative to capture all relevant aspects in the network. The selection of nodes significantly influences the validity of the network and the resulting conclusions [12, 45].
Variably defined nodes can lead to different network inferences, as demonstrated by the findings of Hoffman et al. [16] indicating that high versus low cut-offs of Cut Down and Withdrawal considerably changed the resulting network inferences. Moreover, measurement errors, particularly in smaller samples or when nodes are based on a single indicator, can distort the network [43]. Using multiple indicators for a single node is advisable to mitigate this issue. Nodes with topological overlap measure similar concepts and can also skew results. For example, Huth et al. [7] combined two symptoms under Loss of Control, implying that these separate nodes could possibly be represented as one.
Omitting nodes can have even more serious implications. Although focusing on DSM-based AUD symptom networks allows for more straightforward comparisons, it risks overlooking clinically relevant non-DSM symptoms or external factors that might influence AUD persistence, such as employment status or stress levels. Omitted nodes can be a confounding factor (i.e. common cause) for the link between two nodes in the network. For example, stress levels could cause both difficulties in successfully cutting down consumption and stronger desires to drink. Without considering stress, these two variables would be related but this relationship is statistically spurious, as stress is the cause of both variables.
Taken together, the considerations around node inclusions highlight a critical area for further research. Specifically, developing strategies for determining which nodes to include and devising methods to compare networks that only have partly overlapping nodes are essential next steps.
Undertake confirmatory work and model building
Network studies on AUD, like those on other disorders, have predominantly relied on exploratory or descriptive research methods [36]. This approach has established a foundation of descriptive findings, facilitating hypothesis generation and knowledge expansion. However, we and others advocate for a shift from individual, exploratory studies to model and theory building [45]. A critical first step is to test and replicate previous findings [51]. Additionally, there is a necessity to integrate these findings with existing theories to develop a formal model of AUD.
Formal models offer a clear and precise framework essential for hypothesis testing, making predictions and refining theories in scientific research [52]. They enable cost-effective experimentation, foster interdisciplinary collaboration and enhance decision-making processes. Efforts like those by van den Ende et al. [4] lay a promising groundwork. Furthermore, recently published guidelines on model building [53, 54] could be instrumental in this regard.
Quality assessment
We evaluated quality regarding sample characteristics, reporting, analysis and adherence to Open Science practices, based on the published guidelines for reporting cross-sectional network analyses in the field [23]. Regarding sample quality and reporting, there is a significant need for more detailed descriptions of the clinical characteristics of participants. Often, such information is either missing or limited to comorbidities with other substance uses. A more comprehensive clinical description would enhance our understanding of group similarities and differences, even in studies focusing solely on AUD symptoms.
Additionally, sharing data, partial association matrices, raw centrality scores and analyses are vital. This practice would significantly facilitate the comprehension, reproduction and aggregation of individual study results. There is also an urgent need for improved uncertainty assessment, as observed in the studies we reviewed [46]. Often, the uncertainty assessment was missing, poorly reported or suboptimal. This limitation hindered our ability to aggregate statistically robust findings, as presented in the work of Malgaroli et al. [13], thus affecting the certainty we can place in the current overall findings.
Bayesian network analysis offers a natural way to estimate various forms of uncertainty, including evidence for absent edges, uncertainty in network structure and parameter values [46]. Enhanced quantification of uncertainty is crucial for understanding the (non)replication between studies and the degree of confidence we can place in individual study findings [55].
CONCLUSION
Our study identified six relevant AUD symptom network studies, collectively revealing densely interconnected networks with consistent edge inclusion across all analyses. Certain symptoms, such as Larger/Longer and Physical/Psychological Problems, exhibited high centrality, aligning with the DSM-5 guidelines and major etiological models. Conversely, Hazardous Use was consistently less central, possibly indicating a more specific symptom of AUD. Additionally, network characteristics varied between clinical and population samples, emphasizing differences in symptom centrality and interconnections. Ultimately, the clinical relevance and overall quality of AUD symptom network studies are expected to be enhanced by future research that incorporates our suggested improvements, including higher quality of reporting and selection of (clinical) samples and nodes, investment in model building and validation, and the use of longitudinal and individual-level network designs.
AUTHOR CONTRIBUTIONS
Eve Oostendorp: Conceptualization (equal); data curation (equal); investigation (equal); methodology (equal); visualization (equal); writing—original draft (equal); writing—review and editing (equal). Karoline Huth: Data curation (equal); investigation (equal); methodology (equal); visualization (equal); writing—original draft (equal); writing—review and editing (equal). Freek Linders: Data curation (equal); formal analysis (equal); investigation (equal); validation (equal); writing—original draft (equal); writing—review and editing (equal). Judy Luigjes: Investigation (equal); writing—original draft (equal); writing—review and editing (equal). Anneke E. Goudriaan: Conceptualization (equal); investigation (equal); methodology (equal); writing—original draft (equal); writing—review and editing (equal). Ruth J. van Holst: Conceptualization (equal); formal analysis (equal); investigation (equal); project administration (equal); supervision (equal); writing—original draft (equal); writing—review and editing (equal).
ACKNOWLEDGEMENTS
None.
DECLARATION OF INTERESTS
The authors have no conflicts of interest to declare.
DATA AVAILABILITY STATEMENT
All details about this project, including search strategy, analysis code, results, plots and online supporting information, are available at https://osf.io/um3w4/.
REFERENCES
- 1 A full description is detailed in the PRISMA-Protocol, accessible at https://osf.io/um3w4/.