Impaired social decision-making in males with methamphetamine use disorder
Ming-Hui Li and Mingming Zhang contributed equally to this study.
Abstract
Individuals with methamphetamine use disorder (MUD) commonly exhibit socially problematic behaviours. Investigating the prosocial decision-making of individuals with MUD could enable a better understanding of their impaired social functioning and help improve their social relationships. We conducted two studies to examine the performance of individuals with MUD and healthy controls on a modified dictator game. In Study 1, 55 male individuals with MUD and 34 healthy male participants made a series of choices between two pairs of monetary prizes for themselves and for others. In Study 2, 62 male individuals with MUD and 31 healthy male participants made the same choices as in Study 1 after a brief exposure to methamphetamine-related pictures. In both studies, we consistently found a context dependency of decreased prosociality in individuals with MUD. That is, individuals with MUD made fewer prosocial choices than healthy individuals in disadvantageous contexts (but not advantageous contexts). The results of the computational model suggested that the lower prosociality of individuals with MUD in disadvantageous contexts could be attributed to the lower weight placed on others' benefits. Moreover, when exposed to methamphetamine-related pictures, individuals with MUD showed less caution and slower encoding/motor speed than healthy individuals, and individuals with MUD with a longer history of methamphetamine use tended to respond less cautiously. Our findings provide evidence that in disadvantageous contexts, individuals with MUD show reduced prosociality and less consideration of others' benefits. Identifying the origin of the alterations in prosocial decision-making has implications for diagnosis and treatment.
1 INTRODUCTION
Methamphetamine is a highly addictive stimulant that is associated with numerous negative consequences.1, 2 Individuals with methamphetamine use disorder (MUD) have poor physical and psychological health.3 They also have low levels of social adaptation and experience a number of interpersonal difficulties.2 One of the major difficulties experienced by individuals with MUD is interacting well with others. Specifically, individuals with MUD exhibit insensitivity to others' thoughts and feelings and even engage in behaviour that is harmful to other people, such as aggressive and antisocial behaviours.2, 4, 5 These impaired social interactions may increase negative mood states and increase the risk of relapse among individuals with MUD.6, 7
Altruistic and cooperative interactions are central to human social behaviour.8, 9 Many of our important decisions are made in social contexts where the costs and benefits to both oneself and other people need to be considered.10 Prosocial behaviour, which involves helping others at a cost to the self, is important in maintaining positive relationships with others.11, 12 In this vein, prosocial behaviour plays an important role in social functioning. Investigating the prosocial decision-making processes of individuals with MUD could enable a better understanding of their impaired social functioning and help improve their social relationships. Studies of cocaine and methylphenidate users have used economic decision-making tasks, such as dictator games and distribution games, to examine social dysfunctions.13-15 Existing findings suggested that compared with controls, cocaine and methylphenidate users were more self-serving or less prosocial, as evidenced by giving less money to others in the dictator game.13, 14 In addition, Verdejo-Garcia et al.15 found alterations in brain activation during the ultimatum game in cocaine users, such as reduced activation in the dorsolateral prefrontal cortex, compared with controls, during the evaluation of unfair offers. Moreover, a longitudinal study on cocaine users revealed slight improvements in prosocial behaviour in the dictator game and distribution game after 1 year of abstinence.16 However, few studies have directly investigated the prosocial decision-making processes of individuals with MUD and how these individuals value their own interests over the interests of others.17, 18 Therefore, the aim of the present research was to investigate how individuals with MUD would behave during a prosocial decision-making task.
Recent studies have demonstrated that MUD is associated with deficits in social cognition, such as emotion recognition and theory of mind.5 Increasing evidence suggests that individuals with MUD have an impaired ability to correctly identify emotions and infer the mental state of others.19-22 Specifically, individuals with MUD are less empathetic and have more difficulty understanding another's thoughts, feelings and intentions. Many studies with drug-free participants have demonstrated that impairments in empathy or theory of mind are associated with antisocial or offending behaviours.23, 24 In contrast, individuals who scored higher on social cognition measures, such as emotion-understanding, perspective-taking and false-belief tasks, exhibited higher levels of generous behaviour.11, 12, 25 Given that individuals with MUD have impaired social cognitive abilities, they may make fewer prosocial decisions than healthy individuals.
Evidence from neuroscience research also provides strong circumstantial evidence for the argument that methamphetamine use is linked with decreased prosociality. The neurotoxic effects of chronic methamphetamine use may include abnormalities in brain structure and function.1 Many of the brain regions affected by methamphetamine are also implicated in prosocial decision-making.20 Methamphetamine use has been found to lead to dysfunction in the prefrontal cortex and other areas, such as the striatum and insula.6, 21, 26 Activity in these brain regions is an important neural underpinning of prosocial decision-making.25, 27, 28 For example, anterior insula and temporoparietal junction activity has been shown to predict generous donations.25 Activity in the ventromedial prefrontal cortex has been shown to increase when donating to charities, and activity in the striatum has been shown to be positively correlated with the frequency of donation.28 Given that individuals with MUD show dysfunction in the brain regions involved in prosocial decision-making, they are likely to make fewer prosocial decisions than healthy individuals.
The aforementioned literature suggests that individuals with MUD have lower levels of prosociality than healthy individuals; however, there is a lack of direct evidence for this suggestion. In this research, we examined the behaviours of individuals with MUD and healthy controls (HCs) on a modified dictator game derived from Hutcherson et al.29 In this task, participants make a series of choices between two pairs of monetary prizes for themselves (¥Self) and others (¥Other). These choices involve a trade-off between what is best for the self and what is best for the other (a stranger) and thus require people to choose to act selfishly or prosocially. We hypothesized that individuals with MUD would make fewer prosocial choices than healthy individuals.
Furthermore, we used a computational model to abstract the cognitive mechanisms underlying individuals' performance from their choices and response times (RTs). This model builds on the framework of drift-diffusion models (DDMs) of binary response selection, which have been used successfully in a range of cognitive tasks and as psychometric tools in clinical research to examine individual differences.29-31 This model assumes that choices are made by first assigning a value to each option under consideration and then comparing them in value-based decision-making.32 Attention may play a role in this comparison process by affecting the value assigned to the attended option32 and the amount of information needed to make a decision.33 Model-based analysis has several advantages over traditional comparisons of choice and RT. First, the model takes both choice and RT data into consideration when estimating the model parameters. Second, the model can provide a more detailed explanation of the nature of the decision-making process. Finally, the model is more sensitive to group differences in the behavioural task, as extraneous effects of the other parameters are controlled (e.g., response caution is controlled for when estimating the weights).
We also investigated the effect of exposure to drug-related cues on prosocial decision-making. This drug cue paradigm has been widely used to study both craving and attentional bias toward drug-related stimuli.34 Through repeated administration of a drug, drug users attribute incentive salience to drug-related stimuli.34 As these stimuli would grab users' attention, autonomic and enhanced signalling of these stimuli would leave fewer resources for drug users to perform subsequent tasks.35 Previous studies using DDMs suggested that a decline in cognitive resources (e.g., under time pressure) led to a reduced availability of information needed to trigger a decision.30 Therefore, we speculate that exposure to methamphetamine-related cues may reduce the attention that individuals with MUD allocate to the subsequent prosocial decision-making task and consequently reduce the availability of information needed to make a decision.
In the present research, we conducted two studies. In Study 1, individuals with MUD and demographically matched HCs completed the modified dictator game. Given that previous work has demonstrated significant cognitive effects of cue exposure on individuals with MUD, we integrated methamphetamine-related pictures in Study 2 to further examine the differences in prosocial decision-making between individuals with MUD and HCs. In Study 2, demographically similar individuals with MUD and HCs made the same choices as in Study 1 after a brief exposure to methamphetamine-related pictures.
2 METHODS AND MATERIALS
2.1 Participants
All participants provided written informed consent in accordance with procedures approved by the Institutional Review Board of the Institute of Psychology, Chinese Academy of Sciences and Shanghai Mental Health Center.
In Study 1, participants were individuals with MUD and demographically similar HCs. The inclusion criteria for individuals with MUD were to meet the criteria of stimulant use disorder (amphetamine-type substance) in the Diagnostic and Statistical Manual of Mental Disorders (fifth edition)36 as assessed by a structured interview, have been using methamphetamine for at least 1 year, use the drug at least three times per week over a period of at least 1 month (individuals reporting occasional drug use were not included) and be willing to participate in the study. In addition, we conducted a brief interview and recruited individuals who self-reported that they did not use other drugs (e.g., heroin, cocaine and cannabis) and that they did not have a history of psychiatric disorders and major or neurological diseases (e.g., epilepsy, stroke and dementia). Fifty-five individuals with MUD (male; mean age, 35.02 years; range, 21–54) were recruited from the drug rehabilitation centre via advertisements. All of them had negative urine tests when entering the rehabilitation centre and were currently abstaining from drug use. Thirty-four HCs (male; mean age, 36.97 years; range, 20–59) were recruited via advertisements. They had no history of abusing any illicit drugs. All participants were right-handed and had normal or corrected-to-normal vision. Individuals with MUD were given a bottle of shampoo (10 yuan, approximately US$1.4), and HCs were paid 10 yuan (approximately US$1.4) for participating.
In Study 2, a total of 93 male participants were recruited. Two different samples were used for Study 1 and Study 2. Individuals with MUD were required to meet the same inclusion criteria as in Study 1. Sixty-two individuals with MUD (mean age, 36.29 years; range, 23–57) were recruited from the drug rehabilitation centre. They had negative urine tests when entering the rehabilitation centre and were currently abstaining from drug use. Thirty-one HCs (mean age, 36.68 years; range, 19–59) were recruited via advertisements. They had no history of abuse of any illicit drugs. Individuals with MUD were given a bottle of shampoo (10 yuan, approximately US$1.4), and HCs were paid 10 yuan (approximately US$1.4) for participating.
Demographic and clinical data were collected. All participants reported their age, educational level, alcohol standard drinks that were defined as 10 g alcohol per drink37 and cigarette smoking. They also completed the Beck Anxiety Inventory (BAI),38, 39 Pittsburgh Sleep Quality Index (PSQI)40, 41 and Barratt Impulsiveness Scale (BIS).42, 43 These standardized questionnaires were used to evaluate anxiety, sleep quality and impulsivity symptomatology. For individuals with MUD, the characteristics of methamphetamine use were assessed, including the duration of current abstinence (months), years of methamphetamine use before abstinence and dosage of methamphetamine use before abstinence (g/month). The demographic and clinical data of all participants in both studies are reported in Table 1.
| Study 1 | MUD (N = 55) | HC (N = 34) | t | p | Cohen's d | ||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Age | 35.02 | 7.40 | 36.97 | 12.14 | −0.85 | 0.402 | 0.21 |
| Education (years) | 9.29 | 3.14 | 10.29 | 3.01 | −1.49 | 0.141 | 0.32 |
| BAI | 27.45 | 7.46 | 27.71 | 8.86 | −0.14 | 0.886 | 0.03 |
| PSQI | 6.36 | 3.76 | 4.56 | 2.54 | 2.70 | 0.008 | 0.54 |
| BIS | 80.89 | 17.43 | 73.15 | 20.84 | 1.89 | 0.062 | 0.41 |
| Alcohol standard drinks (10 g/drink) | 2.75 | 4.88 | 3.12 | 3.72 | −0.37 | 0.711 | 0.09 |
| Number of cigarettes smoked per day | 13.95 | 8.81 | 13.79 | 8.57 | 0.08 | 0.935 | 0.02 |
| DSM-5 score | 6.93 | 2.48 | NA | NA | NA | NA | NA |
| Duration of current abstinence (months) | 6.04 | 4.67 | NA | NA | NA | NA | NA |
| Years of methamphetamine use before abstinence | 7.65 | 4.78 | NA | NA | NA | NA | NA |
| Dosage of methamphetamine use before abstinence (g/month) | 14.66 | 14.57 | NA | NA | NA | NA | NA |
| Study 2 | MUD (N = 62) | HC (N = 31) | t | p | Cohen's d | ||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Age | 36.29 | 7.97 | 36.68 | 12.67 | −0.16 | 0.877 | 0.04 |
| Education (years) | 9.33 | 3.23 | 9.55 | 2.53 | −0.33 | 0.743 | 0.07 |
| BAI | 25.7 | 5.66 | 24.94 | 4.97 | 0.69 | 0.494 | 0.15 |
| PSQI | 6.48 | 3.74 | 4.03 | 2.56 | 3.71 | <0.001 | 0.72 |
| BIS | 81.48 | 16.55 | 72.16 | 20.52 | 2.36 | 0.020 | 0.52 |
| Alcohol standard drinks (10 g/drink) | 3.38 | 6.35 | 5.63 | 9.44 | −1.36 | 0.177 | 0.28 |
| Number of cigarettes smoked per day | 13.23 | 8.86 | 12.26 | 8.39 | 0.51 | 0.615 | 0.11 |
| DSM-5 score | 6.60 | 2.61 | NA | NA | NA | NA | NA |
| Duration of current abstinence (months) | 7.34 | 5.49 | NA | NA | NA | NA | NA |
| Years of methamphetamine use before abstinence | 7.13 | 3.72 | NA | NA | NA | NA | NA |
| Dosage of methamphetamine use before abstinence (g/month) | 12.86 | 13.13 | NA | NA | NA | NA | NA |
- Abbreviations: BAI, Beck Anxiety Inventory; BIS, Barratt Impulsivity Scale; NA, not applicable; PSQI, Pittsburgh Sleep Quality Index.
2.2 Behavioural task
Each individual's level of prosociality was estimated in a modified dictator game derived from Hutcherson et al.29 In each trial, participants chose between two pairs of monetary prizes (Figure 1A). Each pair has two outcomes: money to themselves (¥Self) and money to another (¥Other). One pair was a constant pair of ¥50 to both self and other. The other pair was a nonconstant pair drawn from one of the nine pairs shown in Figure 1B. Each of the nine nonconstant pairs appeared 12 times, and the pairs were randomly intermixed across trials. To minimize habituation and repetition effects, we jittered the amounts of the nine nonconstant pairs by ±¥1, except amounts above ¥100, which were always jittered downward. Accordingly, each nonconstant pair consisted of two or three different stimuli, and 22 unique choice problems with different amounts were presented in the task. The side of the screen on which the constant pair appeared was counterbalanced across trials. In Study 2, participants were asked to complete the same task as in Study 1, except that a methamphetamine-related picture was presented (lasting 1 s) before the choice phase. Twenty-eight colour pictures were randomly presented, and each picture was repeated two to four times across the task in Study 2. The pictures depicted methamphetamine-related scenes, including drug, drug instruments and drug use.
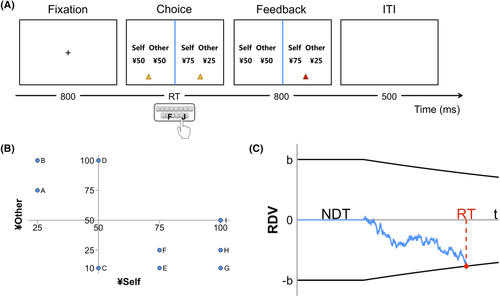
The interaction partner and monetary rewards were hypothetical. Participants were directed to imagine that they were randomly paired with a stranger and would make a series of choices about allocating money between themselves and the stranger. The task was conducted with E-Prime 2.0 (Psychology Software Tools Inc.). Each trial started with a fixation in the middle of screen (lasting 800 ms). Then, the two prize pairs were presented, and participants had up to 8 s to indicate their choice by pressing the letter F or J on the keyboard. Next, feedback with the chosen pair marked by a red triangle was presented (lasting 800 ms). There was a 500 ms interval between two trials. Each participant made 108 choices during the experimental blocks. We assigned the 108 trials to two blocks, and participants could take a break between blocks. Participants completed five practice trials before performing the experimental blocks.
2.3 Computational modelling
As in prior work, we modelled participants' behaviour with a computational model that has been shown to provide accurate descriptions of both choice and RT data in the modified dictator game29 (Figure 1C). The model has five primary parameters: drift slopes for self and other ( and ), starting value and collapse rate of decision threshold ( and , respectively) and nondecision time (NDT). Drift slopes for self and other reflect the weights placed on monetary prizes for self and other during the evidence accumulation process. A larger slope for self would promote fewer prosocial choices, while a larger slope for others would promote more prosocial choices. The decision threshold represents the amount of information required to make a decision, reflecting response caution. Nondecision time accounts for sensory and motor-related processes unrelated to the comparison process itself.
Following the method of Hutcherson et al.,29 we used the maximum likelihood method based on a simulated likelihood function to estimate the best-fitting parameters of the model for each participant. All trials including nonresponses were used to fit the model. RT was separated into bins from 0 to 8 s in 250 ms increments, and there was an additional bin for nonresponses. We computed the likelihood function for choices and RT bins by running 1000 simulations of the model with each possible combination of parameters for each unique choice problem used in the task. We first used a grid of parameter combinations derived from Hutcherson et al.29 To avoid participants falling on a boundary edge for the parameters (no more than 2%), we then adjusted the range of the grid and performed a grid search with in {−0.015, −0.0135, …, 0.015}, in {−0.0075, −0.006, …, 0.0135}, NDT in {0, 0.2, …, 1.6}, in {0.02, 0.04, …, 0.48} and in {0, 0.00005, 0.0001, 0.00025, 0.0005, 0.00075, 0.001, 0.005}. Based on the likelihoods generated from the simulations, the parameter combination that minimized the negative log-likelihood of all trials for each participant was identified. If more than one parameter combination resulted in the same minimal negative log-likelihood, one was randomly selected as the solution.
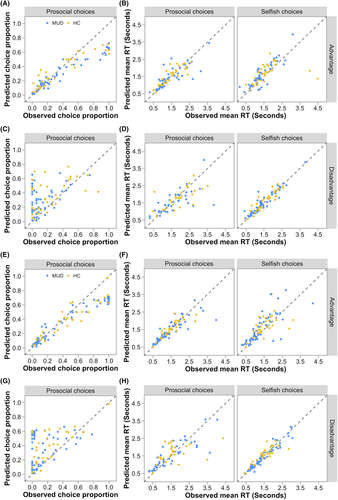
To assess the fit quality, we simulated 1000 samples of each choice problem for every participant with the best-fitting parameters. We then computed the summary statistics (proportions of prosocial choices and mean RTs associated with prosocial and selfish choices) over observed and simulated data separately for each participant. Correlations between these summary statistics from the simulated and the observed data were tested to check whether the model could capture interindividual differences. In addition, for each unique choice problem completed by each participant, we calculated the proportion of prosocial choices and mean RT over observed and simulated data. The problem-level correlations regarding these statistics for each participant were computed to check whether the model could capture intraindividual differences.
To examine the differences in model parameters between individuals with MUD and HCs, we fitted models using the full set of trials, as well as the subsets of disadvantageous trials and advantageous trials, for each participant.
3 RESULTS
3.1 Study 1
3.1.1 Behavioural results
Statistical analyses were performed using R (Version 3.6.1). The trials on which participants failed to make a choice within the 8 s time limit (0.1%) were excluded from the analysis.
We coded choices as Prosocial if the participants gave up their own benefits to help the stranger, that is, choosing the prize pair with smaller ¥Self or greater ¥Other; otherwise, choices were coded as Selfish. Specifically, for disadvantageous trials in which ¥Self was smaller than ¥Other (types A, B and D), choosing the constant pair was coded as Selfish. For advantageous trials in which ¥Self was greater than ¥Other (types C, E, F, G, H and I), choosing the constant pair was coded as Prosocial.
The choice data were analysed using a mixed-effects binary logistic regression model; the prosocial choice was coded as 1, while the selfish choice was coded as 0. Group (MUD vs. HC), trial type and their interaction were included in the model as fixed factors, and participant was included as a random factor.
The results showed a significant main effect of trial type (χ2(8, N = 9602) = 933.53, p < 0.001) and a significant interaction effect between group and trial type (χ2(8, N = 9602) = 129.75, p < 0.001). As shown in Figure 2A, simple effect analysis revealed that for disadvantageous trials, individuals with MUD made fewer prosocial choices than HCs (type A: Z = −2.54, p = 0.011, odds ratio (OR) [95% CI] = 0.35 [0.07, 0.63]; type B: Z = −4.00, p < 0.001, OR = 0.19 [0.04, 0.35]; type D: Z = −2.11, p = 0.035, OR = 0.44 [0.10, 0.77]), whereas no significant group differences were observed for advantageous trials (ps > 0.21). No other significant effects were observed. We obtained similar results when we included age, BAI, PSQI and BIS as control variables in the model (see Supporting Information for detailed results). The results suggested a context dependency of decreased prosocial choices in individuals with MUD.
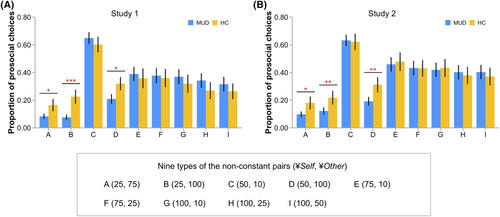
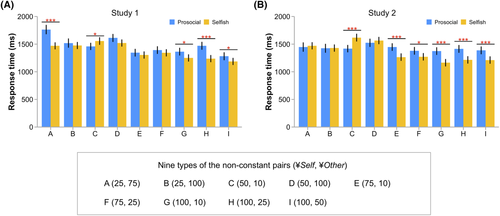
RT was analysed using a mixed-effects linear regression model. Group, choice (prosocial versus selfish), trial type and their two-way and three-way interactions were included in the model as fixed factors, and participant was included as a random factor. The results revealed significant main effects of choice and trial type and a significant effect of their interaction (ps < 0.001). No significant group-related effects were observed. The estimated marginal means of RT are shown in Figure 3A. We obtained similar results when we included age, BAI, PSQI and BIS as control variables in the model (see Supporting Information for detailed results).
3.1.2 Model estimation
As shown in Figure 4A–D, model predictions captured the interindividual differences in proportions of prosocial choices (MUD: r53 = 0.30, p = 0.027 for disadvantageous trials, and r53 = 0.97, p < 0.001 for advantageous trials; HC: r32 = 0.51, p = 0.002 for disadvantageous trials, and r32 = 0.93, p < 0.001 for advantageous trials), in mean RTs associated with prosocial choices (MUD: r36 = 0.70, p < 0.001 for disadvantageous trials, and r52 = 0.83, p < 0.001 for advantageous trials; HC: r25 = 0.70, p < 0.001 for disadvantageous trials, and r31 = 0.85, p < 0.001 for advantageous trials) and in mean RTs associated with selfish choices (MUD: r53 = 0.94, p < 0.001 for disadvantageous trials, and r48 = 0.87, p < 0.001 for advantageous trials; HC: r32 = 0.91, p < 0.001 for disadvantageous trials, and r30 = 0.38, p = 0.031 for advantageous trials). The model also captured the intraindividual differences in proportions of prosocial choices (MUD: mean r = 0.42, one-sample t54 = 11.23, p < 0.001; HC: mean r = 0.41, one-sample t33 = 9.42, p < 0.001) and in mean RTs (MUD: mean r = 0.28, one-sample t54 = 6.48, p < 0.001; HC: mean r = 0.30, one-sample t33 = 6.88, p < 0.001).
To examine differences in the model parameters between the MUD and HC groups, we conducted independent-samples t tests for each of the five parameters estimated from the full set of trials. The results showed that individuals with MUD had a smaller than HCs (t87 = −2.22, p = 0.029, Cohen's d = 0.48) (Table 2 and Figure 5B). No other significant differences were observed.
| Study 1 | Study 2 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MUD | HC | t | p | Cohen's d | MUD | HC | t | p | Cohen's d | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||||||||
| Full dataset | 0.0027 | 0.0059 | 0.0031 | 0.0044 | −0.31 | 0.759 | 0.07 | 0.0015 | 0.0062 | 0.0013 | 0.0039 | 0.23 | 0.819 | 0.04 | |
| −0.0013 | 0.0022 | −0.0002 | 0.0024 | −2.22 | 0.029 | 0.48 | −0.0015 | 0.0021 | −0.0005 | 0.0021 | −2.02 | 0.046 | 0.44 | ||
| 0.142 | 0.077 | 0.166 | 0.076 | −1.48 | 0.144 | 0.32 | 0.166 | 0.105 | 0.154 | 0.063 | 0.70 | 0.484 | 0.13 | ||
| 0.00026 | 0.00031 | 0.00022 | 0.00025 | 0.64 | 0.527 | 0.14 | 0.00047 | 0.00068 | 0.00019 | 0.00025 | 2.86 | 0.005 | 0.48 | ||
| NDT | 0.411 | 0.242 | 0.359 | 0.189 | 1.07 | 0.288 | 0.23 | 0.371 | 0.245 | 0.303 | 0.247 | 1.25 | 0.213 | 0.28 | |
| Disadvantage | 0.0062 | 0.0045 | 0.0051 | 0.0048 | 1.12 | 0.266 | 0.24 | 0.0055 | 0.0039 | 0.0047 | 0.0046 | 0.92 | 0.358 | 0.20 | |
| −0.0034 | 0.0033 | −0.0017 | 0.0032 | −2.37 | 0.020 | 0.52 | −0.0037 | 0.0032 | −0.0015 | 0.0034 | −2.95 | 0.004 | 0.65 | ||
| 0.203 | 0.109 | 0.215 | 0.122 | −0.46 | 0.647 | 0.10 | 0.196 | 0.126 | 0.187 | 0.101 | 0.36 | 0.720 | 0.08 | ||
| 0.00038 | 0.00036 | 0.00056 | 0.00116 | −0.87 | 0.388 | 0.23 | 0.00044 | 0.00039 | 0.00026 | 0.00031 | 2.21 | 0.029 | 0.49 | ||
| NDT | 0.382 | 0.291 | 0.412 | 0.355 | −0.43 | 0.666 | 0.09 | 0.442 | 0.285 | 0.355 | 0.291 | 1.38 | 0.171 | 0.30 | |
| Advantage | 0.0032 | 0.0055 | 0.0037 | 0.0035 | −0.47 | 0.642 | 0.09 | 0.0018 | 0.0055 | 0.0017 | 0.0039 | 0.05 | 0.961 | 0.01 | |
| 0.0015 | 0.0041 | 0.0016 | 0.0045 | −0.11 | 0.911 | 0.02 | 0.0016 | 0.0043 | 0.0016 | 0.0037 | 0.05 | 0.958 | 0.01 | ||
| 0.165 | 0.093 | 0.162 | 0.074 | 0.13 | 0.900 | 0.03 | 0.161 | 0.079 | 0.180 | 0.102 | −1.01 | 0.314 | 0.22 | ||
| 0.00033 | 0.00034 | 0.00027 | 0.00029 | 0.90 | 0.370 | 0.20 | 0.00046 | 0.00040 | 0.00025 | 0.00027 | 2.97 | 0.004 | 0.58 | ||
| NDT | 0.349 | 0.204 | 0.371 | 0.226 | −0.46 | 0.645 | 0.10 | 0.377 | 0.202 | 0.265 | 0.227 | 2.44 | 0.017 | 0.54 | |
- Note: and represent weights applied to the value of self and other. and represent the starting value and collapse rate of the decision threshold. NDT: nondecision time.
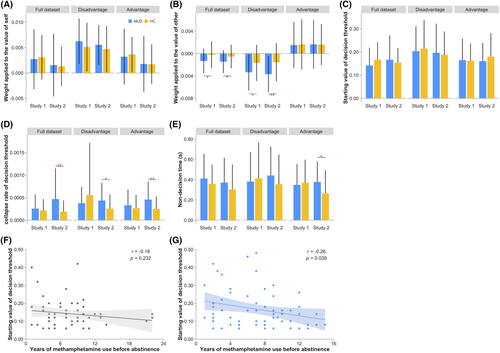
Given that choice data revealed the context dependency of decreased prosocial choices in individuals with MUD, we also fitted the model separately for disadvantageous trials and advantageous trials and assessed the fit quality. The model fitted the data well (results on model fit are provided in the Supporting Information). The independent-samples t tests showed that the significantly smaller of individuals with MUD than HCs was observed only in the disadvantageous context (t87 = −2.37, p = 0.020, Cohen's d = 0.52) (Table 2 and Figure 5B) but not in the advantageous context. No other significant difference was observed. Analyses with age, BAI, PSQI and BIS as control variables yielded similar results (see Table S1).
3.1.3 Correlation analysis
Pearson's correlation analysis was used to examine the associations of methamphetamine use variables with levels of prosociality and model parameters among individuals with MUD. Methamphetamine use variables included the duration of current abstinence, years of methamphetamine use before abstinence and dosage of methamphetamine use before abstinence.
We calculated the proportion of prosocial choices as an index of prosociality for each individual with MUD. No significant correlations were observed between the level of prosociality and any methamphetamine use variable.
Similarly, no significant correlation was observed for the model parameters.
3.2 Study 2
Statistical analyses were performed using R (Version 3.6.1). There were 13 (0.1%) invalid trials in Study 2.
3.2.1 Behavioural results
The choice data were analysed using a mixed-effects binary logistic regression model as in Study 1. The results revealed a significant main effect of trial type (χ2(8, N = 10,031) = 1134.03, p < 0.001) and a significant interaction effect between group and trial type (χ2(8, N = 10,031) = 73.40, p < 0.001). As shown in Figure 2B, simple effect analysis suggested that for disadvantageous trials, individuals with MUD made fewer prosocial choices than HCs (type A: Z = −2.50, p = 0.013, OR = 0.32 [0.03, 0.60]; type B: Z = −2.60, p = 0.010, OR = 0.31 [0.03, 0.58]; type D: Z = −2.62, p = 0.009, OR = 0.31 [0.04, 0.58]), while no significant group differences were observed for advantageous trials (ps > 0.56). No other significant effects were observed. We obtained similar results when we included age, BAI, PSQI and BIS as control variables in the model (see Supporting Information for detailed results). Similar to Study 1, the results suggested a context dependency of decreased prosocial choices in individuals with MUD.
RT was analysed using a mixed-effects linear regression model as in Study 1. The results revealed significant main effects of choice and trial type and a significant effect of their interaction (ps < 0.001). No significant group-related effects were observed. The estimated marginal means of RT are shown in Figure 3B. We obtained similar results when we included age, BAI, PSQI and BIS as control variables in the model (see Supporting Information for detailed results).
3.2.2 Model estimation
As shown in Figure 4E–H, model predictions captured the interindividual differences in proportions of prosocial choices (MUD: r60 = 0.34, p = 0.008 for disadvantageous trials, and r60 = 0.97, p < 0.001 for advantageous trials; HC: r29 = 0.72, p < 0.001 for disadvantageous trials, and r29 = 0.93, p < 0.001 for advantageous trials), in mean RTs associated with prosocial choices (MUD: r40 = 0.86, p < 0.001 for disadvantageous trials, and r59 = 0.87, p < 0.001 for advantageous trials; HC: r24 = 0.43, p = 0.028 for disadvantageous trials, and r28 = 0.86, p < 0.001 for advantageous trials) and in mean RTs associated with selfish choices (MUD: r60 = 0.97, p < 0.001 for disadvantageous trials, and r53 = 0.75, p < 0.001 for advantageous trials; HC: r28 = 0.84, p < 0.001 for disadvantageous trials, and r28 = 0.60, p < 0.001 for advantageous trials). The model also captured the intraindividual differences in proportions of prosocial choices (MUD: mean r = 0.33, one-sample t61 = 9.50, p < 0.001; HC: mean r = 0.28, one-sample t30 = 5.51, p < 0.001) and in mean RTs (MUD: mean r = 0.21, one-sample t61 = 4.65, p < 0.001; HC: mean r = 0.14, one-sample t30 = 3.17, p = 0.004). We also fitted the model separately for disadvantageous trials and advantageous trials and assessed the fit quality. The model fitted the data well (results on model fits are provided in the Supporting Information).
The independent-samples t tests for parameters estimated from the full set of trials revealed that individuals with MUD had smaller (t91 = −2.02, p = 0.046, Cohen's d = 0.44) and faster collapse rates (t85.2 = 2.86, p = 0.005, Cohen's d = 0.48) than HCs (Table 2 and Figure 5B,D). No other significant differences were observed.
For parameters estimated from the disadvantageous trials, individuals with MUD had smaller (t91 = −2.95, p = 0.004, Cohen's d = 0.65) and faster collapse rates (t91 = 2.21, p = 0.029, Cohen's d = 0.49) than HCs (Table 2 and Figure 5B,D). No other significant differences were observed.
For parameters estimated from the advantageous trials, individuals with MUD had faster collapse rates (t81.2 = 2.97, p = 0.004, Cohen's d = 0.58) and longer nondecision times (t91 = 2.44, p = 0.017, Cohen's d = 0.54) than HCs (Table 2 and Figure 5D,E). No other significant differences were observed. Analyses with age, BAI, PSQI and BIS as control variables yielded similar results (see Table S1).
3.2.3 Correlation analysis
As in Study 1, no significant correlations were observed between the level of prosociality and any methamphetamine use variable.
For model parameters, we found that the starting threshold estimated from the full dataset was negatively correlated with years of methamphetamine use before abstinence (r = −0.26, p = 0.039) (Figure 5G). No other significant correlation was observed.
4 DISCUSSION
The utilization of measures of social behaviour, such as prosocial decision-making, may enable a more comprehensive assessment of the impact of methamphetamine use on cognitive and psychosocial functions. In two studies using male participants, we consistently found that in disadvantageous contexts, individuals with MUD made fewer prosocial choices than healthy individuals (¥Self < ¥Other). We used a computational model that described our data well to abstract the cognitive mechanisms underlying individuals' performance. The results of model fitting suggested that individuals with MUD have lower levels of prosociality not because they give higher weight to their own benefits but because they give lower weight to others' benefits. Moreover, individuals with MUD had less stringent decision criteria and slower encoding/motor speed than healthy individuals when exposed to methamphetamine-related pictures, suggesting that exposure to methamphetamine-related pictures could exacerbate the cognitive impairments of individuals with MUD in prosocial decision-making. Our findings provide empirical evidence indicating that male individuals with MUD are less prosocial and more socially inconsiderate than healthy individuals, especially in disadvantageous contexts.
Decisions in the social context often require trade-offs between self-interest and consideration of others.44 The choice data do not indicate whether the decreased prosociality in individuals with MUD was due to higher levels of self-interest or lower levels of concern about the interests of others. The results of the computational model revealed that the decreased prosociality in individuals with MUD was attributed to their lower consideration of others' benefits. In other words, individuals with MUD may have intact self-preferences but an impaired ability to care about the welfare of others during prosocial decision-making. This result is consistent with previous findings that individuals with MUD have difficulty being able to accurately infer another's thoughts, feelings and intentions.2 However, social cognitive research pertinent to methamphetamine use has largely overlooked the context dependency of impaired social cognitive ability in individuals with MUD. Our findings underscore that individuals with MUD at a disadvantage (rather than at an advantage) show an inability to consider the interests of others.
Interestingly, our findings revealed a context dependency of decreased prosociality in individuals with MUD. This context dependency might be due to higher cognitive demands in the disadvantageous context than in the advantageous context. On the one hand, more deliberative processing is needed for value representations of others' interests than of selves'.29 On the other hand, there is an asymmetry of responses to obtaining an inferior payoff versus a superior payoff in interpersonal contexts.45-47 People strongly dislike receiving less than others but do not have strong preferences for getting more than others.45 Considering others' benefits in a disadvantageous context might require higher cognitive demands than in an advantageous context. Research finds that individuals with MUD show moderate cognitive deficits across various cognitive domains, such as attention, executive functions and working memory5; these findings may explain why we found that individuals with MUD gave lower weights to others' interests and made fewer prosocial choices only in a disadvantageous context, not in an advantageous context. We acknowledge that this reasoning offers a tentative rather than a conclusive explanation of the context dependency. Future studies will be needed to better understand this phenomenon.
Identifying the origin of the alterations in prosocial decision-making has implications for not only diagnosis but also treatment. The finding that individuals with MUD give lower weight to others' benefits implies that neuromodulators linked to other-regarding social computations in nonclinical fields (e.g., oxytocin)10 could have significant implications for therapeutic strategies for individuals with MUD. The finding of the context dependency of decreased prosociality in individuals with MUD implies that tailored treatments must consider social interactions and social contexts, including but not limited to contexts where individuals with MUD are at a disadvantage.
In Study 2, we also found a faster collapse rate and a longer nondecision time in individuals with MUD than in HCs. In the collapsing-bound model, less evidence is required to trigger a decision as the collapse rate increases.30 The faster collapse rate of individuals with MUD suggests that individuals with MUD were less cautious than healthy individuals when making decisions after exposure to methamphetamine-related pictures. This finding was consistent with our speculation that in individuals with MUD, exposure to methamphetamine-related pictures could reduce the cognitive resources available for performing the prosocial decision-making task and consequently reduced the available information needed to make a decision. As nondecision time accounts for the duration of stimulus encoding and response execution,48 the longer nondecision time in individuals with MUD reflects slower encoding/motor speed with exposure to methamphetamine-related pictures. The slowdown of encoding/motor processes was also observed in schizophrenia patients49 and after alcohol intake.50 Our results are consistent with previous findings that performance on cognitive tasks requiring divided attention and the inhibition of distracting information were significantly impaired during exposure to methamphetamine-related cues in individuals with MUD but not in HCs.51
We also found that the characteristics of methamphetamine use could be implicated in the starting value of the decision threshold when individuals with MUD were exposed to methamphetamine-related pictures. Similar to the collapse rate, the starting threshold determines the amount of information needed for a response and thus represents response caution.30 Our findings suggest that individuals with MUD with a longer duration of methamphetamine use tended to respond less cautiously in the prosocial decision-making task. This result may be due to the decreased amount of cognitive resources available for performing the task among individuals with MUD with longer durations of methamphetamine use, given that the duration of methamphetamine use is related to cognitive deficits.52 Future studies can explore whether the starting threshold could be used to assess the severity of methamphetamine abuse.
Notably, the attention and motor processes of individuals with MUD during the prosocial decision-making task could be influenced by any form of picture. To substantiate whether the differences in collapse rate and nondecision time between individuals with MUD and HCs are due to exposure to pictures or methamphetamine-related pictures, the results of Study 2 are favourably compared with the results obtained using non-methamphetamine-related pictures. Given that participants were not exposed to any picture in Study 1, the two studies should be compared with caution. Future research using non-methamphetamine-related pictures is needed to decompose the effects of pictures and methamphetamine-related pictures.
We highlight some limitations here. First, this study cannot answer conclusively whether the lower level of prosociality observed in participants with MUD reflects a predisposition, is a consequence of excessive methamphetamine use or results from the negative characteristic of methamphetamine users' lives (e.g., being secretive or fearful of arrest). Longitudinal studies (especially long-term tracking) and lifestyle-related measures are needed to address the main cause of impaired social cognition in individuals with MUD. Second, the interaction partners and monetary rewards were hypothetical in the decision-making task. But participants were directed to imagine the choices—to make as they would if the interactions were real and we did not assess whether the participants in fact assumed that they were in a real social interaction. To exclude the possibility that participants might fail in the required imaginary act, future studies could use real partners and rewards. Third, social decision-making in cocaine users could be affected by socio-economic status, ADHD symptoms, depressive symptoms, cannabis co-use, positive drug urine tests and cocaine craving.13 Although our findings are robust after controlling for age, BAI, PSQI and BIS, future studies should take into consideration potential confounders (e.g., socio-economic status and psychiatric symptoms). Finally, there were only male participants in this study. While many characteristics and behaviours related to methamphetamine use are similar for males and females, there are gender differences in some aspects, such as motivation for initial use and methamphetamine-related problems.53 Future research could examine how females with MUD behave in social decision-making situations.
In summary, this study provides evidence that males with MUD exhibit decreased levels of prosociality and less consideration of others' benefits during social decision-making. One paradox of methamphetamine use is that despite the original intention of methamphetamine use being to promote social interactions, methamphetamine abuse commonly erodes social connections.2, 6 Our findings point to an important factor that could undermine the interpersonal relationships of individuals with MUD and their adjustment in various social situations. The reduced expression of prosociality and the lower weight given to others' benefits among individuals with MUD can lead to the social dysfunctions associated with methamphetamine use (e.g., interpersonal violence and social isolation). These maladaptive social behaviours may ultimately result in relapse and sustainment of methamphetamine abuse.21 Therefore, treatment and rehabilitation for individuals with MUD must consider the role of social cognition and incorporate the relearning of social interactions and behaviours.
ACKNOWLEDGEMENTS
This work was supported by National Science and Technology Innovation 2030 Major Project of China (2021ZD0203900). This work was also supported by the National Natural Science Foundation of China (92046006). We thank Cendri A. Hutcherson for sharing the MATLAB code for computational model analysis. We also thank Xiao-Yang Sui, Qian Zhuang, Bin Zhan, Lanjun Zhou and Yan Zeng for the help in collecting the data.
CONFLICT OF INTEREST
The authors declare no competing interests.
AUTHOR CONTRIBUTIONS
Li-Lin Rao and Ti-Fei Yuan developed and designed the experiments. Mingming Zhang conducted data collection. Ming-Hui Li performed the statistical analyses and drafted the manuscript. All authors provided critical revisions.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study can be accessed at http://ir.psych.ac.cn/handle/311026/38648.