The effects of acute alcohol administration on circulating endocannabinoid levels in humans
Address where the work was carried out: 10 Center Drive, Bethesda, MD 20892-1540, USA.
Trial registration: clinicaltrials.gov Identifiers: NCT00713492
Abstract
Several lines of evidence suggest that endocannabinoid signalling may influence alcohol consumption. Preclinical studies have found that pharmacological blockade of cannabinoid receptor 1 leads to reductions in alcohol intake. Furthermore, variations in endocannabinoid metabolism between individuals may be associated with the presence and severity of alcohol use disorder. However, little is known about the acute effects of alcohol on the endocannabinoid system in humans. In this study, we evaluated the effect of acute alcohol administration on circulating endocannabinoid levels by analysing data from two highly-controlled alcohol administration experiments. In the first within-subjects experiment, 47 healthy participants were randomized to receive alcohol and placebo in a counterbalanced order. Alcohol was administered using an intravenous clamping procedure such that each participant attained a nearly identical breath alcohol concentration of 0.05%, maintained over 3 h. In the second experiment, 23 healthy participants self-administered alcohol intravenously; participants had control over their exposure throughout the paradigm. In both experiments, circulating concentrations of two endocannabinoids, N-arachidonoylethanolamine (AEA) and 2-arachidonoylglycerol (2-AG), were measured at baseline and following alcohol exposure. During the intravenous clamping procedure, acute alcohol administration reduced circulating AEA but not 2-AG levels when compared to placebo. This finding was confirmed in the self-administration paradigm, where alcohol reduced AEA levels in an exposure-dependent manner. Future studies should seek to determine whether alcohol administration has similar effects on brain endocannabinoid signalling. An improved understanding of the bidirectional relationship between endocannabinoid signalling and alcohol intake may deepen our understanding of the aetiology and repercussions of alcohol use disorder.
1 INTRODUCTION
Despite increasing rates of alcohol use and misuse over the past decades,1 no new pharmacological treatments for alcohol use disorder have been approved by the FDA in over 15 years. One potential novel target of interest is the endocannabinoid system.2 Preclinical evidence suggests that blocking cannabinoid receptor 1 (CB1) decreases alcohol intake.3-5 Altered endocannabinoid signalling may also affect human alcohol consumption. For example, individuals with a less functional variant of the gene for fatty acid amide hydrolase (FAAH), an enzyme that degrades the endocannabinoid transmitter anandamide, were more likely to be diagnosed with alcohol dependence.6 Individuals with alcohol dependence who carried this polymorphism and were of European ancestry were also found to binge drink more often, have higher scores on the Alcohol Use Disorder Identification Test (AUDIT) and have more severe alcohol dependence based on symptom counts.6 Despite these findings, blocking endocannabinoid signalling in humans has not been an effective treatment for alcohol use disorder (AUD) thus far. Treatment with the inverse CB1 agonist rimonabant failed to reduce relapse to alcohol use compared with placebo in a clinical trial7 or decrease alcohol self-administration in a human laboratory study.8 Nevertheless, novel agents targeting the endocannabinoid system are being developed which may hold promise for the treatment of AUD.2
Endocannabinoid signalling seems to influence alcohol consumption and, conversely, alcohol consumption may also impact endocannabinoid signalling. An acute infusion of intravenous alcohol has been shown to increase CB1 receptor availability in healthy human participants.9 By contrast, there is evidence from several studies that chronic alcohol intake may downregulate central CB1 receptors.10 CB1 receptors are also present in the periphery and there are circulating endocannabinoids present within serum and plasma. The two major endocannabinoids that function as endogenous ligands of cannabinoid receptors are N-arachidonoylethanolamine (AEA, also known as anandamide) and 2-arachidonoylglycerol (2-AG). Both AEA and 2-AG are agonists of CB1, although 2-AG is a more efficacious agonist than AEA.11, 12 In the brain, AEA and 2-AG are synthesized on demand by the postsynaptic cell and function as retrograde neurotransmitters, binding to CB1 receptors in presynaptic terminals and suppressing neurotransmitter release.13 AEA may additionally act in a paracrine fashion in the periphery, with preclinical evidence suggesting that macrophage-derived anandamide may lead to neighbouring pancreatic beta cell death in a mouse model of type 2 diabetes mellitus.14 However, the overall physiological roles of AEA and 2-AG in the periphery are still not well defined.15 Understanding the impact of acute and chronic alcohol intake on both central and circulating endocannabinoids is of importance in order to fully elucidate the relationship between alcohol use and endocannabinoid signalling.
By using data from two well-controlled human laboratory studies, we sought to examine how acute alcohol administration influences circulating levels of two of the main endocannabinoid transmitters: AEA and 2-AG. In the first within-subjects study (the fixed-dose study), healthy participants were administered either placebo or intravenous alcohol clamped at a fixed breath alcohol concentration (BrAC) of 50 mg%, equivalent to just over 60% of the current legal limit for driving (80 mg% or 0.08%). The target BrAC of 50 mg% was chosen to represent a moderate exposure comparable to two to three drinks in most people. On each experimental day, circulating endocannabinoids were measured prior to and following an intravenous infusion of alcohol. In the second study (the alcohol self-administration study), a separate group of healthy participants completed an intravenous alcohol self-administration paradigm. Circulating endocannabinoid concentrations were measured both before and during the self-administration procedure. Based on the results of a prior study, which found reductions in AEA and 2-AG levels following oral alcohol consumption,16 we hypothesized that both alcohol self-administration and fixed alcohol exposure using the alcohol clamp would decrease AEA and 2-AG concentrations in an exposure-related manner.
2 MATERIALS AND METHODS
2.1 Experimental paradigms
Two human laboratory studies were conducted at the National Institute on Alcohol Abuse and Alcoholism (NIAAA) in Bethesda, Maryland. All study procedures were approved by the NIH Intramural Institutional Review Board at the National Institutes of Health. Participants provided written informed consent prior to enrolling in each study.
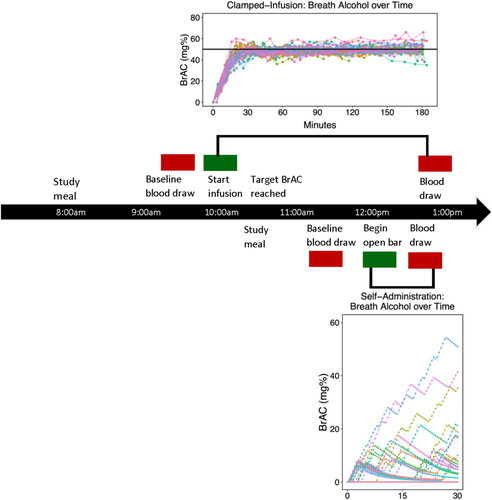
The fixed-dose study utilized an intravenous alcohol clamp paradigm17 in which participants were infused with alcohol with the goal of attaining and maintaining a target BrAC of 50 mg% over a period of 3 h. The main goal of this study was to evaluate the influence of age and sex on alcohol elimination rates and responses in healthy men and women. Forty-eight participants were recruited for this study. Of these participants, 47 had both pre- and post-infusion blood samples (i.e., blood draws occurred just prior to the paradigm and after 180 min) (Figure 1). The alcohol self-administration study utilized an intravenous computer-assisted alcohol self-administration paradigm in which participants controlled their own exposure to alcohol, which was allowed to range from 0 to 100 mg%.18, 19 The main goal of this study was to compare the effects of stress, alcohol-related, and neutral cues on alcohol self-administration. For the present analysis, we evaluated data from the neutral cues session to maintain consistency with the clamped infusion study (data from the other sessions will be published elsewhere). Thirty-three participants enrolled in the alcohol self-administration study. Of these, data from 23 were analysed; data from eight participants were not analysed due to study withdrawal prior to sample collection, and data from two participants could not be analysed due to significant haemolysis of samples or damaged sample vials. Endocannabinoid concentrations were detectable in all participants with non-hemolyzed blood samples and were measured at baseline (approximately 20 min prior to the start of alcohol self-administration) and after 30 min of alcohol self-administration (see Table S1 for a comparison of the two studies).
2.2 Study population
Both the fixed-dose and the self-administration studies recruited healthy participants, as determined by medical history, physical exam, electrocardiogram and routine blood tests. The studies shared the following inclusion and exclusion criteria: participants were current non-smokers (although past smokers who had quit for over 1 year were eligible); participants with a current or prior history of serious medical illness including cardiovascular, respiratory, gastrointestinal, hepatic, renal, endocrine or reproductive disorders were excluded; individuals with a positive hepatitis or HIV test at screening were also excluded; participants were evaluated using the Structured Clinical Interview for DSM-IV (SCID-IV)20 and were excluded if they had any current Axis-I psychiatric disorder or a past history of drug or alcohol dependence; participants were excluded if they were using prescription or over the counter medications that are known to interact with alcohol within 2 weeks of the study or if they had a positive result on a urine drug screen or alcohol breathalyser at the start of any study visit; females were excluded if they were currently pregnant (positive urine beta-hCG test) or intended to become pregnant; and participants who were alcohol naïve or alcohol abstainers were excluded.
The alcohol clamp study enrolled social drinkers stratified by age and sex. By design, half of the participants were young females and males between 21 and 25 years of age and the other half were older females and males between 55 and 65 years of age (Table 1). Participants with alcohol use exceeding 14 drinks per week for males and seven drinks per week for females or use of more than four drinks on any one occasion in the 6 months prior to the study were excluded. Participants needed to be family history negative for alcoholism (i.e., no family history of alcoholism in first or second degree relatives). All participants needed to report the absence of flushing either currently or in the past based on the Alcohol Flushing Questionnaire, assessed during screening. Young women needed to have normal menstrual cycles and were tested in the follicular phase of their menstrual cycle (within 7 days of offset of menses) and needed to have a negative urine pregnancy test at the start of each study session. Older women were post-menopausal with cessation of menses for at least 12 months prior to enrolment into the study and a serum follicle stimulating hormone (FSH) level >40 IU/L. Younger female participants were not permitted to use oral contraceptive pills and older female participants were not permitted to use hormone replacement therapy. Participants were also not permitted to use herbal preparations containing soy isoflavones, which may have estrogenic properties. Participants were not permitted to have ferromagnetic objects in their bodies which might adversely be affected by MRI and could not be unable to undergo an MRI scan for liver volume due to claustrophobia or anxiety when confined to small spaces.
| Fixed-dose study | Alcohol self-administration study | |
|---|---|---|
| Participants (N) | 47 | 23 |
| Age (years, mean [SD]) | Younger group: 23.1 (1.0) | 26.9 (4.8) |
| Older group: 59.4 (3.0) | ||
| Sex (male, N [%]) | 23 (48.9%) | 13 (56.5%) |
| Body Mass Index (kg/m2, mean [SD]) | 25.2 (3.9) | 24.7 (4.4) |
| Caucasian (N [%]) | 39 (83.0%) | 15 (65.2%) |
| African American (N [%]) | 3 (6.4%) | 5 (21.7%) |
| Hispanic (N [%]) | 3 (6.4%) | 3 (13.0%) |
| Average drinks per drinking day (median [Q1, Q3]) | 1.6 (1.1, 2.2) | Bingers (N = 14): 3.4 (2.8, 3.9) |
| Non-bingers (N = 9): 1.7 (1.5, 2.1) | ||
| Total drinking days (median [Q1, Q3]) | 17.0 (7.0, 37.0) | Bingers (N = 14): 29.5 (20.0, 38.0) |
| Non-bingers (N = 9): 29.0 (14.0, 39.0) | ||
| Binge drinking days (Median [Q1, Q3]) | 0.0 (0.0, 1.0) | Bingers (N = 14): 7.5 (4.0, 12.0) |
| Non-bingers (N = 9): 0.0 (0.0, 0.0) |
- Note: The fixed-dose study was stratified by age (younger group aged 21–25, older group aged 55–65) and sex. The self-administration study was stratified by binge drinking status. Binge drinking participants reported at least two binge drinking sessions in the month prior to the session, with a binge being defined as at least four drinks for females and at least five drinks for males in a given day. Average drinks per drinking day, total drinking days, and binge drinking days were derived from a 90-day timeline Followback interview. Drinking data for the fixed-dose study were not available for eight participants.
By contrast, the alcohol self-administration study enrolled male and female participants between 21 and 45 years of age stratified by binge-drinking status, where bingers were defined as consuming at least four drinks (females) or five drinks (males) in at least two drinking sessions during the month prior to the study and non-bingers were defined as having no binge drinking episodes in the month prior to the study (Table 1). Individuals seeking treatment for alcohol use disorders were excluded. All participants had at least one experience drinking five or more drinks on one occasion in their lifetime. Females had normal menstrual cycles and were tested outside of the menses phase of their cycle. Females also needed to have a negative urine pregnancy test at the start of each study session. Participants were excluded if they had a history of significant withdrawal symptoms or presented at screening with clinically significant withdrawal symptoms (Clinical Institute Withdrawal Assessment for Alcohol scale revised21 score >8). Participants were also excluded if they had current or prior history of alcohol-induced flushing reactions.
2.3 Study design
The intravenous alcohol clamp study used a physiologically-based pharmacokinetic (PBPK) model paradigm to maintain participants at a fixed BrAC throughout the study.22, 23 The PBPK model calculated infusion-rate profiles for each participant to achieve and maintain BrAC at the target values of 50 and 0 mg% in the alcohol and placebo sessions, respectively. The alcohol and placebo sessions were conducted in cross-over, counter-balanced order across participants and scheduled approximately 7 days apart. Participants were asked to abstain from alcohol for 48 h prior to the infusion session. They arrived at the NIAAA outpatient clinic at around 7:00 AM following an overnight fast and received a light breakfast (~300 calories) approximately 3 h prior to the infusion. The infusion was started at approximately 10:00 AM. A breathalyser test was performed to ensure a zero breath alcohol concentration prior to the infusion. An indwelling intravenous catheter for ethanol or normal saline infusion and blood sampling was inserted into the antecubital vein of the arm using a sterile technique. Approximately 30 min prior to the start of the infusion, baseline blood samples were collected. Next, participants received either 6% v/v ethanol or 0.9% sodium chloride, administered in randomized, counter-balanced order between two single-blinded sessions. For the alcohol session, the infusion rate increased exponentially until a target blood alcohol concentration (BAC) of 50 mg% was reached at 15 min followed by an exponentially decreasing infusion rate which tapers to a constant steady-state value, to maintain the BAC at the target value for the predetermined 165-min interval. Serial breathalyser measurements ensured that participants were within 5 mg% of the target BAC and enabled minor adjustments to the infusion rate to overcome errors in parameter estimation and experimental variability. The infusion was terminated at the end of the 3-h period.
The IV alcohol self-administration study used the computer-assisted self-administration of alcohol paradigm, which allows participants to infuse ethanol to their preferred level of intoxication.24, 25 This procedure has been shown to differentiate drinkers at high-risk and low-risk for alcohol use disorder18, 19 and has been used to examine potential genetic risk factors for AUD.26 Participants were recruited to the National Institute on Alcohol Abuse and Alcoholism's outpatient clinic for five sessions. The first session was a baseline alcohol self-administration session, which allowed individuals to acclimatize to the IV alcohol self-administration procedure. The second session consisted of a manual-based semi-structured interview session27 to obtain personal vignettes from participants for the creation of personalized guided imagery scripts (approximately 5 min in length) to induce alcohol, stress or neutral states. In each of the final three alcohol self-administration sessions, participants were exposed to one of their three scripts in randomized order prior to alcohol self-administration. Data utilized in our analysis come from the neutral self-administration session as our main objective in these analyses was to determine the effects of alcohol on circulating endocannabinoid concentrations. The effects of stress-cues and alcohol-cues will be examined in future publications. For each self-administration session, participants arrived at the clinic at around 11:00 AM after abstaining from alcohol for 48 h and received a light lunch (~350 calories). Unlike the fixed-dose study, participants were not asked to fast overnight. A breathalyser test was performed to ensure a zero breath alcohol concentration prior to alcohol self-administration. Indwelling intravenous catheters were inserted into the antecubital vein of both arms, one for the alcohol infusion and the other for blood sampling. Following a 1-h relaxation period, participants heard their personalized neutral script via headphones and were asked to imagine the situation being described as if they were actively participating in it. The guided imagery was presented over 5 min. Then participants participated in a free-access alcohol self-administration paradigm, during which time they could press a button for standardized IV infusions of alcohol. The free-access period lasted 120 min overall. Participants could infuse up to a maximum breath alcohol concentration of 100 mg%, imposed for safety reasons. Blood samples taken at baseline (approximately 20 min prior to the infusion) and at 30 min after the start of the infusion were analysed. The 30-min timepoint was selected to evaluate the short-term effect of alcohol on circulating AEA and 2-AG concentrations, which were previously found to be reduced following red wine consumption at 20 and 45 min, respectively.16
2.4 Measurement of circulating endocannabinoid concentrations
Blood processing steps included centrifugation at 1880G for 10 min at 4°C, pipetting off the supernatant plasma and freezing the sample at −80°C until analysis. AEA and 2-AG were quantified in plasma samples from human subjects by liquid chromatography/tandem mass spectrometry. 100-μl plasma was incubated at −20°C for 10 min with 900-ml ice-cold acetone and 400-μl Tris buffer (50 mM, pH 8.0) to precipitate proteins. After spinning at 3000 g at 4°C for 10 min, the supernatant was transferred to a glass tube to evaporate the acetone phase under nitrogen flow. Then, the supernatant was extracted two times with 2 mL of CHCl3:MeOH (2:1, vol/vol). Lower chloroform phase was collected and transferred to another glass tube. Then combined chloroform phases were dried under nitrogen flow. The dried samples were reconstituted in 50 μl of ice-cold methanol prior to loading the autosampler for mass spectrometry measurements. The LC–MS/MS measurements were conducted on an Agilent 6410 triple quadrupole mass spectrometer (Agilent Technologies, USA) coupled to an Agilent 1200 LC system (Agilent Technologies, Waldbron, Germany) with conditions set as previously described.28 Liquid chromatographic separation was obtained using 2-μl injections of samples onto a Zorbax SB-C18 rapid resolution HT column (2.1 mm × 50 mm, 1.8 μm) from Agilent Technologies. The autosampler temperature was set at 4°C and the column was maintained at 34°C during the analysis. Gradient elution mobile phases consisted of A (0.1% formic acid in water) and B (0.1% formic acid in methanol). Gradient elution (250 μl/min) began and was held at 10% B for the first 0.5 min, followed by a linear increase towards 85% B at 1 min; this was maintained until 12.5 min and then increased linearly again to 100% B at 13 min; this was maintained until 22 min. At minute 28.5, the gradient changed linear to the initial setting, which was maintained for 6 min. The Agilent 6410 triple quadrupole mass spectrometer was set for electrospray ionization (ESI). The electrospray interface was operated in positive ion mode. The source parameters were as follows: capillary voltage, 4000 V; gas temperature, 350°C; drying gas, 10 L/min; and nitrogen was used as the nebulizing gas with a pressure of 40 psig. Collision-induced dissociation (CID) energy was performed by using nitrogen. Levels of endocannabinoids were analysed by multiple reactions monitoring (MRM). The molecular ion and fragment for each compound were measured as follows: m/z 348.3➔62.1 for AEA, m/z 352.3➔66.1 for [2H4]AEA and m/z 379.3➔91.1 for 2-AG. The analytes were quantified using MassHunter Workstation LC/QQQ Acquisition and MassHunter Workstation Quantitative Analysis software (Agilent Technologies). The amounts of AEA and 2-AG in the samples were determined against standard curves using [2H4]AEA as internal standard. Values are expressed as pmol/ml.
2.5 Data analysis
2.5.1 Fixed-dose study
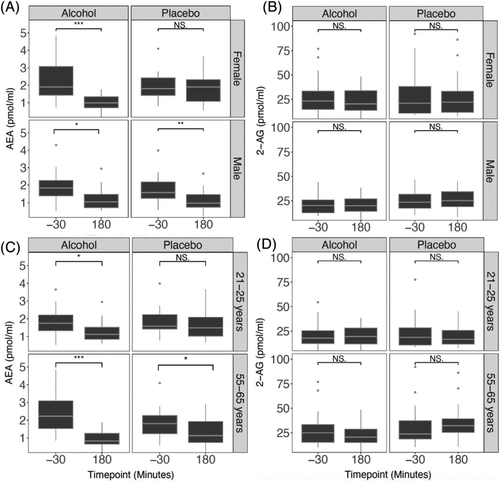
Circulating endocannabinoid concentrations were log-transformed to a normal distribution. A repeated measures ANOVA was then used to analyse the effect of alcohol exposure on circulating AEA and 2-AG concentrations. Drug (alcohol or placebo) and time (pre- or post- infusion) were included as within-subjects factors. The main outcome of interest in this analysis was whether the change in circulating endocannabinoid concentrations over time differed by drug condition, that is, whether there was a significant drug by time interaction. Given that sample recruitment was stratified by age and sex, we also performed exploratory ANOVAs with sex or age group (21–25 years and 55–65 years) as between-subjects factors. The main objectives of these exploratory analyses were to determine whether there were drug by time by age or drug by time by sex interactions. The relationships between age group, sex, drug condition, and time were explored visually with boxplots (Figure 3). Wilcoxon signed-rank tests were used for boxplot visualization to compare changes in endocannabinoids across time in each drug, sex, or age subgroup. For all AEA and 2-AG analyses, we excluded individuals with extreme outlying circulating endocannabinoid concentrations. The standard definition of extreme outliers was used: values three times the interquartile range above the third quartile or below the first quartile.29 Two individuals were removed from the AEA analyses and one individual was removed from the 2-AG analyses.
2.5.2 Alcohol self-administration study
In the alcohol self-administration study, we examined circulating AEA and 2-AG concentrations at baseline (20 min prior to the infusion) and 30 min after the start of the alcohol self-administration. First, paired samples t-tests were used to determine whether there were reductions in AEA and 2-AG during the first 30 min of the alcohol self-administration period. Then, we assessed whether total alcohol exposure (defined as the area under the estimated BAC versus time curve) was associated with change in circulating endocannabinoid concentrations using Pearson's correlations and linear regression. As sample recruitment for this study was stratified by a binary measure of binge drinking, we covaried for binge drinking status in addition to age and sex. As above, we assessed extreme outlying endocannabinoid concentrations using values three times the interquartile range above the third quartile or below the first quartile. There were no extreme outlying endocannabinoid concentrations at baseline, so all data points were retained in the AEA and 2-AG analyses. Finally, as an exploratory analysis, we used paired samples t-tests to analyse changes in AEA and 2-AG in the three individuals in our sample with the highest alcohol exposure (AUC > 500 mg%*min) and in the four individuals in our sample with no alcohol exposure (AUC = 0 mg%*min), with the hypothesis that only individuals with high exposure would experience significant reductions in AEA and 2-AG.
3 RESULTS
3.1 Fixed-dose study
To examine the effects of intravenous alcohol on circulating AEA and 2-AG levels, we used repeated measures ANOVAs with drug (alcohol or placebo) and time (pre- or post-infusion) as within-subjects factors. For AEA, there was a significant drug by time interaction (F[1, 44] = 6.401, p = 0.015), with circulating AEA concentrations showing a greater decline during the alcohol infusion than the placebo infusion (Figures 2 and S1). Average AEA concentrations decreased by 0.97 pmol/ml (SD = 1.14) during the alcohol infusion and 0.36 pmol/ml (SD = 0.97) during the placebo infusion. For 2-AG, there was a significant main effect of drug condition (F[1, 45] = 4.898, p = 0.032), but no significant main effect of time (F[1, 45] = 0.064, p = 0.802) or drug by time interaction (F[1, 45] = 0.476, p = 0.494, Figures 2 and S1). Therefore, although overall 2-AG levels were slightly lower on average on the alcohol infusion day than on the placebo infusion day at both time points, there was no significant decline in 2-AG levels during either infusion.
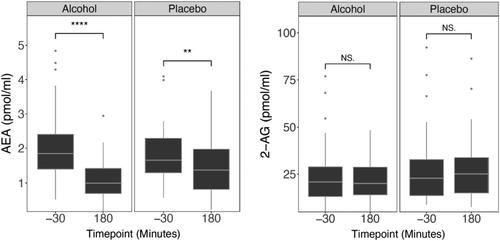
Because the sample was recruited by age and sex, further exploratory ANOVAs were conducted. These models were conducted with age group (21–25 years of age or 55–65 years of age) or sex as a between-subjects variable and drug (alcohol or placebo) and time (pre- or post-infusion) as within-subjects variables. There was a significant three-way interaction between sex, drug, and time on AEA levels (F[1, 43] = 10.788, p = 0.002, Figure 3, Table S2 and Figure S2) and a significant three-way interaction between age group, drug and time on 2-AG levels (F[1, 44] = 7.650, p = 0.008, Figure 3, Table S2 and Figure S2). There were no additional three-way interactions between either sex, drug and time on 2-AG levels or age group, drug and time on AEA levels. Given the three-way interaction for AEA levels, we performed an ANOVA with drug and time as within-subjects factors for each sex. For females, there was a significant drug by time interaction (F[1, 21] = 20.872, p < 0.001), but for males there was no significant drug by time interaction (F[1, 22] = 0.080, p = 0.781). Given the three-way interaction for 2-AG levels, we performed an ANOVA with drug and time as within-subjects factors for each age group. For the younger age group there was no significant drug by time interaction (F[1, 23] = 1.555, p = 0.225), but for the older age group there was a significant drug by time interaction (F[1, 21] = 8.331, p = 0.009).
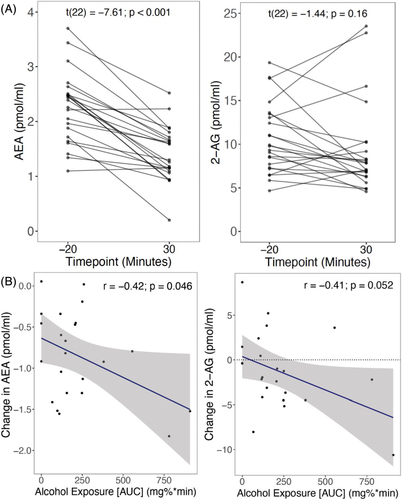
3.2 Self-administration study
In the alcohol self-administration study, circulating endocannabinoid concentrations were measured at baseline (20 min prior to the start of self-administration) and at minute 30 of self-administration. A paired-samples t test demonstrated that during alcohol self-administration, there was a reduction in circulating AEA levels from baseline (t[22] = −7.61, p < 0.001, Figure 4A). There was a correlation between alcohol exposure and change in AEA levels such that individuals with greater alcohol exposure had greater decreases in AEA levels (r = −0.42, p = 0.046, Figure 4B). A linear regression demonstrated that change in AEA was associated with alcohol exposure at a trend level after accounting for binge-drinking status, age and sex (b = −0.00083, 95% CI −0.0017 to 0.000052, p = 0.063, Table 2). In contrast, there was no decline in 2-AG levels during self-administration (t[22] = −1.44, p = 0.16). However, there was a trend level relationship between 2-AG levels and alcohol exposure (r = −0.41, p = 0.052), an effect that remained present at a trend level in a linear regression model accounting for age, sex and binge drinking status (b = −0.0079, 95% CI −0.016 to 0.00063, p = 0.068, Table 2). There was no significant correlation between change in AEA concentration and change in 2-AG concentration over this time period (r = 0.128, p = 0.562).
| AEA | 2-AG | |||||||
|---|---|---|---|---|---|---|---|---|
| b | Standard error | t | p | b | Standard error | t | p | |
| Linear model 1: No covariates | ||||||||
| Intercept | −0.64 | 0.14 | 4.40 | <0.01 | 0.38 | 1.17 | 0.32 | 0.75 |
| Alcohol Exposure | −0.00095 | 0.00045 | −2.12 | 0.046 | −0.0075 | 0.0036 | −2.06 | 0.052 |
| Linear model 2: With covariates | ||||||||
| Intercept | 0.17 | 0.62 | 0.27 | 0.79 | −3.16 | 5.97 | −0.53 | 0.60 |
| Alcohol Exposure | −0.00083 | 0.00042 | −1.98 | 0.063 | −0.0079 | 0.0041 | −1.95 | 0.068 |
| Age | −0.03 | 0.02 | −1.51 | 0.15 | 0.15 | 0.20 | 0.75 | 0.47 |
| Sex | −0.31 | 0.18 | −1.67 | 0.11 | −1.74 | 1.78 | −0.98 | 0.34 |
| Binge drinker | 0.33 | 0.20 | 1.66 | 0.11 | 0.89 | 1.93 | 0.46 | 0.65 |
- Note: Sex is coded as a binary value (0 = female, 1 = male). Binge drinker is also coded as a binary value (0 = non-binge drinker, 1 = binge drinker). For model 1, R2 = 0.177 for the AEA model and R2 = 0.168 for the 2-AG model. For model 2, R2 = 0.475 for the AEA model and R2 = 0.242 for the 2-AG model.
In the alcohol self-administration paradigm, we compared changes in circulating endocannabinoid concentrations in the three individuals who achieved the highest alcohol exposure in our study (AUC > 500 mg%*min) to four individuals who did not self-administer any alcohol (AUC = 0 mg%*min). For AEA, there was a significant reduction from baseline to post-infusion in the high AUC group (t[2] = −4.51, p = 0.046) but no significant change in AEA in the individuals who did not self-administer any alcohol (t[3] = −2.07, p = 0.13, Figure S3). In contrast, there was no significant change in 2-AG in either the high AUC group (t[2] = −0.74, p = 0.53) or the group that did not self-administer any alcohol (t[3] = 1.09, p = 0.36, Figure S3).
4 DISCUSSION
This is the first study to examine the effects of pharmacokinetically-controlled intravenous infusions of alcohol on circulating endocannabinoid levels. We found that exposure to alcohol significantly reduced AEA levels but not 2-AG levels when compared to placebo. To determine whether there was an exposure-related suppression in AEA levels, we then looked at data from an intravenous alcohol self-administration study. We found a correlation between alcohol exposure and AEA reductions, such that individuals who self-administered greater amounts of alcohol had larger reductions in AEA. There was some evidence to suggest a similar relationship between alcohol exposure and reductions in circulating 2-AG levels, although overall circulating 2-AG levels did not decline significantly during the first 30 min of the self-administration paradigm.
To our knowledge, only one other study has examined the effects of acute alcohol administration on circulating endocannabinoid levels. This study found that red wine consumption reduced both AEA and 2-AG levels in humans 20 and 45 min after consumption.16 AEA had its maximal decline after 20 min, whereas 2-AG reached its lowest point after approximately 45 min.16 Interestingly, we did not find similar levels of decline in 2-AG, which may be due to the differences in the time frame of sampling between our studies. It is also possible that methodological differences such as the route of alcohol administration account for these disparate findings; for example, 2-AG levels could be affected by alcohol cues (e.g., smell and taste) or other compounds present in red wine. There is some evidence of such cue-related effects; for example, in social drinkers, alcohol cues have been found to increase circulating AEA levels.30 Future studies should seek to more fully characterize the time course of circulating endocannabinoid changes following alcohol exposure and whether the presence of alcohol cues impacts AEA and 2-AG levels. Furthermore, determining the sources of these alcohol-induced changes in circulating endocannabinoids is another important goal for future studies, as circulating levels may be derived from various organs and tissues including the brain, adipose tissue and skeletal muscle.15
An important future area of work will be to distinguish the effects of acute versus chronic alcohol exposure on endocannabinoid system functioning. With respect to chronic ethanol intake, it has recently been shown that individuals with AUD in early abstinence have higher levels of circulating AEA and lower brain levels of FAAH than healthy controls.31 Individuals diagnosed with AUD also have decreased CB1 availability compared with healthy controls,9, 32 which may be due to receptor downregulation or increased CB1 occupancy by endocannabinoids. It is therefore possible that whereas acute exposure to alcohol leads to reductions in endocannabinoid signalling and subsequent CB1 upregulation,9 longer term exposure eventually leads to compensatory effects in which endocannabinoid signalling is ultimately enhanced through increased synthesis, decreased degradation, or both mechanisms. Before this can be elucidated, studies evaluating circulating and central endocannabinoid system functioning in larger samples of individuals with AUD need to be conducted. Future studies should also determine whether acute alcohol exposure leads to a similar depression of circulating endocannabinoid signalling in chronic heavy drinkers. It should also be noted that not all studies have reported similar findings. For example, the aforementioned PET study found that individuals with AUD had higher circulating AEA concentrations than healthy controls,31 but in another study, abstinent individuals with alcohol dependence had lower circulating AEA concentrations than healthy controls.30 This further highlights the need for larger replication studies.
It is also necessary to elucidate whether altered endocannabinoid signalling perpetuates drinking behaviour in those with AUD. Individuals with the FAAH C385A polymorphism, which reduces FAAH function, are more likely to be diagnosed with alcohol dependence.6 Carriers of this polymorphism who are of European ancestry and have already been diagnosed with alcohol dependence display evidence of a greater addiction severity and increased levels of alcohol consumption.6 In line with this finding, PET imaging using the FAAH radiotracer [11C]CURB found that lower brain levels of FAAH and higher circulating levels of AEA were correlated with greater consumption of alcohol.31 The mechanism for this remains unclear, but there is some evidence that it could be due to crosstalk between the endocannabinoid and dopaminergic systems. For example, administration of AEA increases dopamine release in rodents.33 In both humans and rodents, there is evidence that the FAAH C385A polymorphism leads to changes in D3 receptor levels,34 which may also impact pharmacological responses to alcohol. More studies need to be conducted to determine the mechanism by which endocannabinoid signalling affects alcohol consumption and responses; this should include investigating how altered endocannabinoid signalling influences other neurotransmitter systems.
Our study had several limitations. For the alcohol clamp study, we only measured circulating endocannabinoid levels at two time points; therefore, we are unable to characterize the time course of alcohol exposure's effect on AEA levels. However, data from the alcohol self-administration study suggest that AEA levels start to decline within the first hour of exposure, which is in keeping with other findings.16 We only looked at the effects of relatively low levels of alcohol exposure on circulating endocannabinoid concentrations; it is unclear whether the higher blood alcohol concentrations typically achieved by heavy drinkers would have similar effects. We were investigating the effect of alcohol on circulating levels of endocannabinoids rather than central endocannabinoid signalling. Although there are strong correlations between brain FAAH levels and endocannabinoid levels in the peripheral circulation,31 cerebrospinal AEA levels have not always been found to correspond to serum levels.35 Future studies should therefore examine the effects of acute alcohol exposure on both cerebrospinal endocannabinoid levels and brain FAAH levels using [11C]CURB and other PET tracers. Finally, our self-administration study was limited by a small sample size, therefore we were not able to assess for sex-specific and age-specific effects in this sample. However, given the three-way interactions observed in the fixed-dose study, studies examining temporal and exposure-response effects in a larger sample of male and female participants of varying ages are clearly necessary.
In conclusion, we found evidence that acute alcohol administration suppresses circulating AEA levels in an exposure-dependent manner in healthy participants. We did not find clear evidence of alcohol effects on 2-AG levels. These results, when taken together with our previous findings that altered endocannabinoid signalling is associated with AUD severity, highlight the complex interrelationship between endocannabinoid signalling and alcohol use. As new studies further unravel this complex relationship, the resulting knowledge will hopefully facilitate the development of successful interventions for AUD that target the endocannabinoid system.
ACKNOWLEDGEMENTS
This study was supported by the NIAAA Division of Intramural Clinical and Biological Research (Z1AAA000466 and Z1AAA000310). Development of the CAIS software used for the intravenous alcohol self-administration paradigm was supported by Sean O'Connor, MD, and Martin Plawecki, MD, PhD, at the Indiana Alcohol Research Center (NIH P60 AA007611). Interest in using the CAIS software for IV alcohol laboratory studies may be directed to Vijay Ramchandani ([email protected]) or Martin Plawecki ([email protected]). We would like to thank the clinical staff at NIAAA's intramural programme for their invaluable assistance with conducting this study. We also thank Marcos Sanches for providing helpful advice regarding data analysis.
CONFLICT OF INTEREST
The authors report no conflict of interest.
AUTHOR CONTRIBUTIONS
MES and VAR conceptualized the manuscript. MES and CWG drafted the manuscript and performed the statistical analyses. BLS was responsible for overseeing the alcohol self-administration study included in our analyses. RC, GK, TDK, and HWB, completed the assays to obtain circulating endocannabinoid levels and helped interpret the resulting data. All authors reviewed the manuscript and provided critical revisions.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.