Racism Is Not a Factor in Door-to-electrocardiogram Times of Patients With Symptoms of Acute Coronary Syndrome: A Prospective, Observational Study
Abstract
Background
Investigators have identified important racial identity/ethnicity-based differences in some aspects of acute coronary syndrome (ACS) care and outcomes (time to presentation, symptoms, receipt of coronary angiography/revascularization, repeat revascularization, mortality). Patient-based differences such as pathophysiology and treatment-seeking behavior account only partly for these outcome differences. We sought to investigate whether there are racial identity/ethnicity-based variations in the initial emergency department (ED) triage and care of patients with suspected ACS in Canadian hospitals.
Methods
We prospectively enrolled ED patients with suspected ACS from one university-affiliated and two community hospitals. Trained research assistants administered a standardized interview to gather data on symptoms, treatment-seeking patterns, and self-reported racial/ethnic identity: “white,” South Asian” (SA), “Asian,” or “Other.” Clinical parameters were obtained through chart review. The primary outcome was door-to-electrocardiogram (D2ECG) time. ECG times were log-transformed and two linear regression models, controlling for important demographic, system, and clinical factors, were fit.
Results
Of 448 participants, 214 (48%) reported white identity, 115 (26%) SA, 83 (19%) Asian, and 36 (8%) “Other.” Asian respondents were younger and more likely to report initial discomfort as “low” and be accompanied by family; respondents identifying as “Other” were more likely to report initial discomfort as “high.” There was no difference in D2ECG time between white participants and all other groups, but there were statistically significant differences by sex: women had longer D2ECG times than men. Exploring more specific racial identities revealed similar findings: no significant differences between the white, SA, Asian, and other groups, while sex (women had 13.4% [95% confidence interval, 0.81%–27.57%] longer D2ECG times) remained statistically significantly different in the adjusted models.
Conclusion
Although racial/ethnicity-based differences in aspects of ACS care have been previously identified, we found no differences in the current study of early ED care in a Canadian urban setting. However, female patients experience longer D2ECG times, and this may be a target for process improvements.
Ethnicity has been defined as “a self-chosen category that reflects distinctness based on ancestry, culture, language, religion, and geographic location.”1 Race, or racial identity, by contrast, generally refers to a conferred identity based on an concocted hierarchy of human value related to phenotypes, skin color, and other putative biologic features of inferiority, often associated with exclusion and unequal power between groups.2 Therefore, we use the term ethnicity to refer to a self-chosen category, racial identity to refer to one that has been conferred by others, and racial identity/ethnicity when the source of the designation is unclear.
Rates of receiving guideline-directed treatments, and outcomes, have differed by ethnicity or racial identity,3-13 apparent in symptoms and treatment-seeking among patients with acute coronary syndrome (ACS).11, 14-16 However, these patient-based differences only partly explain the observed differences in access to appropriate treatment and in outcomes. Given the global burden of ACS as well as the spectrum of ethnic diversity, a fuller understanding of the factors contributing to these differences is important, but lacking.
Some researchers have invoked the concept of implicit (unconscious) bias to explain some ethnicity/racial identity–based health care disparities. U.S. physicians have been found to exhibit a strong implicit preference for white over black patients, which was more predictive of their behavior than explicit attitudes, including in care of myocardial infarction patients.3, 17 Similar bias has also been found among pharmacy, nursing, and medical students.18 However, little research has examined whether there are ethnicity/racial identity–based differences in “upstream” processes (e.g., patient–provider interactions or health professionals’ assessment and clinical decision making) in the critical moments after presentation to an emergency department (ED) with symptoms of ACS—processes that shape the eventual clinical trajectory on which ACS patients travel. Indeed, experts have recently urged that the implicit attitudes and behaviors of health professionals be targeted for study.19, 20
We conducted a multisite, observational study to investigate whether there are differences, based on racial identity, in the initial care received (as measured by door-to-ECG [D2ECG] time) among patients presenting to EDs with symptoms of ACS. Both ethnicity and racial identity may affect the quality of health care received, but because our aim was to examine the behaviors of health professionals, we focused on racial identity as a potential predictor of D2ECG.
Methods
Setting and Sample
This was a multicenter, prospective, observational study, conducted in Vancouver, British Columbia, a metropolis of approximately 3 million people. Those identifying as being of Asian and South Asian (SA) ethnicity make up the second and third largest ethnic minorities, respectively, after those of European origin. For this multicenter, prospective, observational study, we identified potential participants in the EDs of three sites: an inner-city, university-affiliated hospital referral center with a 24-hour cardiac catheterization laboratory and two community hospitals. The annual volumes of patients with possible ACS seen at these sites were 2,800, 6,500, and 1,300, respectively. All EDs have established minimum levels for nurse and physician staffing; in particular, the triage positions are always preferentially filled.
Research staff approached patients, either in the ED or, if they could not be approached in the ED for clinical reasons, on an inpatient unit within 48 hours of ED presentation, if they met all of the following inclusion criteria: 1) 20 years of age or older; 2) presented to the ED and triaged with codes related to a possible ACS (see below); 3) suspected to be having ACS, as evidenced by the emergency physician ordering either immediate cardiology consultation or management with a standardized protocol for continued observation (ultimately admitted or not); 4) hemodynamically stable and free of their initial presenting complaint for at least 1 hour; 5) English, Mandarin, Cantonese, or Punjabi speaking; and 5) able to provide informed consent. We excluded patients being cared for by a coinvestigator. We recruited participants 6 days per week, generally between the hours of 0800 and 1800. The research ethics board at each site approved the study and all participants gave written, informed consent.
The sites had similar protocols for managing patients with potential ischemic symptoms. All Canadian EDs use the Canadian Triage and Acuity Scale (CTAS),21 which defines the urgency of the presentation (the maximum interval until a patient should be seen by a physician). Nurses also use the Canadian Emergency Department Information System to classify the presenting complaint (participants included in this study had triage codes of chest pain, cardiac features; chest pain, moderate-severe respiratory distress; chest pain, moderate-severe hemodynamic compromise; chest pain resolved, significant cardiac history), which then generates a corresponding CTAS score. All study sites had protocols in place that triggered a nurse-initiated call for technician to perform an immediate 12-lead ECG for patients triaged with any of the above codes related to suspected ischemia. Depending on clinical status and bed availability, patients were triaged to 1) the resuscitation room, 2) a nurse-staffed stretcher with cardiac monitoring, or 3) a chair in the waiting room,22 This initial location would quickly change, depending on ECG or laboratory findings, change in clinical status, or increased bed availability.
Procedures
After obtaining informed consent, trained research assistants administered a standardized questionnaire in one of the four languages of the patient's choosing. The questionnaire included items about sociodemographic attributes, symptoms (onset, quality, duration), treatment-seeking behavior, their ethnic and racial identity, and satisfaction with the care received in the ED. Following the interview, data regarding delivery of guideline-based and other aspects of care in the ED (e.g., D2ECG time, time to first MD assessment, medications administered) and other processes (e.g., occurrence and timing of cardiology consultation, transfer from ED to an inpatient area) were collected from the clinical record. Data regarding several patient-, environment-, and system-related potential confounders were also collected (e.g., mode of arrival at ED, language spoken, whether accompanied by family/friend, language ability of family/friend, symptoms reported, and ED staffing levels).
Measures
The main outcome, D2ECG, which is a widely accepted measure of ED performance in ACS care, was defined as the time from registration with ED triage to the time of the initial 12-lead ECG, both of which were available as electronic time stamps. For our analysis, in which our focus was on health professionals’ responses to patients, it would have been ideal to ask the staff caring for the participants what they perceived the patient's racial identity to be. However, we felt this would have led to the staff changing their behavior, thus threatening the validity of our findings. Therefore, we relied on participants’ reports of how others perceived them (“reflected racial identity”) using the question: “What about people you meet, what racial background do they tend to think you are? Do they think you're white, Asian, South Asian, black, or Aboriginal or perhaps some combination of these or maybe something else?”23 Trained research assistants recorded participants’ responses verbatim. However, although participants responded freely to the racial identity question, to achieve statistical power we then categorized responses into one of four categories: “white,” “Asian,” “South Asian” (SA), or “other/unknown”). These racial identity categories were chosen based on the most common identities in the Canadian population.24 Two investigators categorized the responses independently and then reviewed the resulting categorizations for agreement.
Data Analysis
Sample sizes were estimated using 80% power, 5% family-wise significance testing, and a 10-minute difference in D2ECG as clinically significant, assuming a normal distribution for log10-transformed mean (±SD) of 1.21 (±0.42) for the white group, using PASS 2008, version 08.0.5. This demonstrated that a total sample size of 402 participants (67 Asian, 134 South Asian, and 201 white) was required. Categorical baseline characteristics were summarized as frequencies and percentages. To test for differences across racial identities, the chi-square test was conducted. Continuous baseline variables were summarized either using the mean and standard deviation or median and first and third quartiles. Racial identity differences were tested using either ANOVA or the Kruskal-Wallis test. Two linear regression models were constructed to assess if there were racial identity–based differences in the primary outcome. In model l, we adjusted for age, sex, and site. To further examine the D2ECG times by racial identity, in model 2 we adjusted for clinically important potential mediators: education, mode of arrival (ambulance or not), severity of discomfort, CTAS score, whether the patient was accompanied by family/friend/coworker, and whether English was the primary language spoken at home, in addition to the variables in model 1. As D2ECG is a naturally right-skewed variable, a log transformation was applied. The beta coefficients and the corresponding 95% confidence intervals (CIs) from the linear regression models were transformed using 100%* (eβ – 1); thus, they can be interpreted as a percent increase or decrease relative to the reference level. Age was categorized as ≤55, 56 to 70, and >70 years, since the linearity assumption was not satisfied. Model 2 was used to assess the two-way interactions between racial identity and site, sex, and age. If the interaction term was not statistically significant (p > 0.05), the interaction term was removed from the model. Statistical analyses were performed using SAS software, version 9.4.
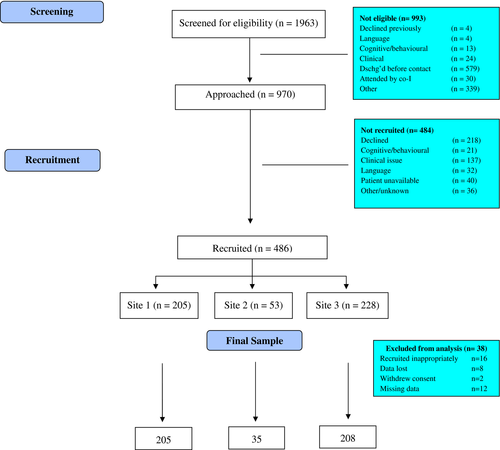
Results
Of 970 eligible patients, 448 participants were recruited between October 2013 and January 2017. Figure 1 outlines the study recruitment flow. The demographic and clinical characteristics of the final sample are summarized in Table 1. A total of 214 (47.8%) reported white racial identity, 115 (25.7%) SA, 83 (18.5%) Asian, and 36 (8.0%) other. There were no significant differences in ages across the groups.
| Characteristic | Racial Identity | ||||
|---|---|---|---|---|---|
| White (n = 214) | Asian (n = 83) | South Asian (n = 115) | Other/Unknown (n = 36) | p-valuea | |
| Female | 85 (39.7) | 33 (39.8) | 42 (36.5) | 13 (36.1) | 0.927 |
| Age (years)b | 62.1 ± 13.7 | 57.3 ± 14.2 | 61.0 ± 14.5 | 59.9 ± 14.3 | 0.067c |
| Age groups (years) | |||||
| ≤55 | 70 (32.7) | 36 (43.4) | 35 (30.4) | 12 (33.3) | 0.460 |
| ≤56 and ≤70 | 84 (39.3) | 32 (38.6) | 49 (42.6) | 16 (44.4) | |
| > 70 | 60 (28.0) | 15 (18.1) | 31 (27.0) | 8 (22.2) | |
| Education | |||||
| High school or less | 85 (39.7) | 40 (48.2) | 64 (55.7) | 14 (38.9) | 0.036 |
| More than high school | 129 (60.3) | 43 (51.8) | 51 (44.3) | 22 (61.1) | |
| Canadian residency status | <0.001 | ||||
| Born in Canada | 156 (72.9) | 13 (15.7) | 14 (12.2) | 13 (36.1) | |
| Not born in Canada | |||||
| Lived ≤ 10 years | 6 (2.8) | 14 (16.9) | 23 (20.0) | 5 (13.9) | |
| Lived > 10 years | 52 (24.3) | 56 (67.5) | 78 (67.8) | 18 (50.0) | |
| English spoken at homed | 195 (91.1) | 20 (24.1) | 19 (16.7) | 23 (63.9) | <0.001 |
| Main symptom chest pain | 156 (72.9) | 67 (80.7) | 93 (80.9) | 31 (86.1) | 0.147 |
| Chest pain on arrival | 197 (92.1) | 76 (91.6) | 110 (95.7) | 35 (97.2) | 0.418 |
| Discomfort on arrival | |||||
| None/low (1–3) | 67 (31.3) | 28 (33.7) | 23 (20.0) | 8 (22.2) | <0.001 |
| Medium (4–7) | 86 (40.2) | 30 (36.1) | 33 (28.7) | 19 (52.8) | |
| High (8–10) | 20 (9.3) | 10 (12.0) | 16 (13.9) | 7 (19.4) | |
| Not available | 41 (19.2) | 15 (18.1) | 43 (37.4) | 2 (5.6) | |
| Arrival by ambulance | 55 (25.7) | 22 (26.5) | 35 (30.4) | 16 (44.4) | 0.128 |
| Accompanied by family/friend/coworker | 77 (36.0) | 42 (50.6) | 48 (41.7) | 11 (30.6) | 0.078 |
| Triage codee | |||||
| CP, cardiac features | 179 (84.0) | 68 (81.9) | 108 (93.9) | 32 (88.9) | |
| CP, severe respiratory distress | 6 (2.8) | 3 (3.6) | 2 (1.7) | 1 (2.8) | |
| CP, respiratory distress (<severe) | 14 (6.5) | 5 (6.0) | 1 (0.9) | 1 (2.8) | |
| CP resolved, signif card hx | 14 (6.6) | 6 (7.2) | 1 (0.9) | 2 (5.6) | |
| Syncope/presyncope | 0 (0.0) | 0 (0.0) | 1 (0.9) | 0 (0.0) | |
| Other | 0 (0.0) | 0 (1.2) | 2 (1.7) | 0 (0.0) | |
| CTASd | |||||
| Level 1 or 2 | 185 (86.9) | 65 (78.3) | 94 (81.7) | 30 (83.3) | 0.303 |
| Level 3 or 4 | 28 (13.1) | 18 (21.7) | 21 (18.3) | 6 (16.7) | |
| Hospital site | |||||
| 1 (tertiary) | 119 (55.6) | 48 (57.8) | 17 (14.8) | 21 (58.3) | <0.001 |
| 2 (community) | 20 (9.3) | 11 (13.3) | 3 (2.6) | 1 (2.8) | |
| 3 (community) | 75 (35.0) | 24 (28.9) | 95 (82.6) | 14 (38.9) | |
| Treatment-seeking delayfg hours | 3.5 (0.5, 24.5) | 2.0 (0.5, 20.0) | 2.1 (0.3, 11.3) | 8.5 (1.0, 66.5) | 0.078h |
- Data are reported as n (%).
- CP = chest pain; CTAS = Canadian Triage and Acuity Scale; signif card hx = significant cardiac history.
- a All testing based on chi-square test unless otherwise noted.
- b Mean ± SD.
- c ANOVA.
- d One missing.
- e Two missing.
- f Twenty-five missing (14 White, seven Asian, two South Asian, two other/unknown).
- g Median (Q1, Q3).
- h Kruskal-Wallis test.
The unadjusted D2ECG times, stratified by racial identity, are presented in Table 2. This unadjusted analysis indicated that SA participants had the shortest time, but after adjustment for baseline differences this was no longer apparent. Our initial model, which adjusted for age, sex, and site, showed no differences by racial identity. However, further examination of white racial identity versus the other groups, with adjustment for additional relevant sociodemographic and clinical variables, revealed statistically significant differences in D2ECG time by 1) sex (women's times were 13.41% [95% CI = 0.81% to 27.57%] longer) and 2) language spoken at home (those not speaking English at home had 15.90% [95% CI = –28.56 to 0.98%] shorter D2ECG times) while racial identity remained nonsignificant (see Table 3 and Figure 2). However, the interaction terms for racial identity by age, sex, and language spoken were not statistically significant. Exploring factors known to vary by sex demonstrated that chest pain was reported less frequently as the main symptom by women (72.5% vs. 81.5% for men, p = 0.04).
| Outcome | Racial Identity | p-valuea | |||
|---|---|---|---|---|---|
| White (n = 214) | Asian (n = 83) | South Asian (n = 115) | Other/Unknown (n = 36) | ||
| Door to ECG (mins) | 15.0 (10.5, 23.0)a | 16.0 (10.0, 23.0) | 12.0 (7.0, 17.0)b | 16.0 (9.5, 27.0) | 0.001 |
- Data are reported as median (Q1, Q3).
- D2ECG = door-to-ECG.
- a Two missing.
- b One missing
| Parameter | (eβ – 1)100% | 95% CI | p-value |
|---|---|---|---|
| Asian vs. white | 10.65 | –8.78 to 34.20 | 0.304 |
| South Asian vs. white | 5.44 | –12.59 to 27.20 | 0.579 |
| Other/unknown vs. white | 24.06 | –0.57 to 54.78 | 0.056 |
| Age ≥ 56 and ≤ 70 vs. < 55 years | 2.14 | –10.86 to 17.02 | 0.760 |
| Age > 70 vs. < 55 | 17.15 | –0.12 to 37.39 | 0.052 |
| Female vs. male | 13.41 | 0.81 to 27.57 | 0.036 |
| Education | |||
| More than high school vs. high school or less education | –6.26 | –16.74 to 5.53 | 0.284 |
| CTAS level 1 or 2 vs. 3 or 4 | –1.01 | –15.78 to 16.35 | 0.902 |
| Accompanied by family/friend/coworker vs. no one | 6.94 | –5.83 to 21.44 | 0.300 |
| Language spoken at home: other vs. English | –15.90 | –28.56 to –0.98 | 0.038 |
| Mode of arrival: not ambulance vs. ambulance | 1.33 | –11.55 to 16.09 | 0.849 |
| Severity of discomfort | |||
| High vs. none/low | –13.60 | –30.02 to 6.67 | 0.167 |
| Medium vs. none/low | –16.71 | –27.94 to –3.73 | 0.014 |
| Missing vs none/low | –14.45 | –28.92 to 2.97 | 0.099 |
- CTAS = Canadian Triage and Acuity Scale; D2ECG = door-to-ECG.
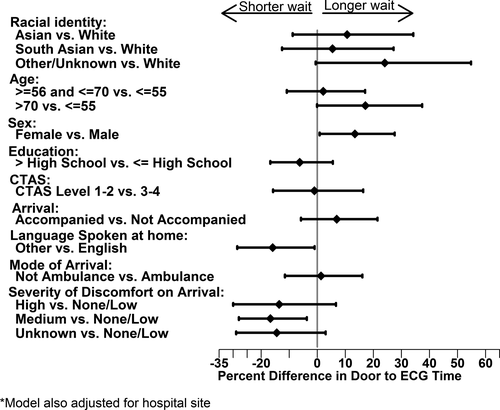
Discussion
We prospectively investigated 448 patients with symptoms of ACS at three Canadian EDs and found no statistically significant differences in D2ECG time, based on racial identity. However, women and those who spoke English at home had significantly longer D2ECG times.
Previous research has found differences based on racial identity in the early phases of ACS care: Diercks et al.25 demonstrated that the 10-minute D2ECG benchmark was significantly less likely to be achieved for nonwhite patients than for white patients and King et al.11 reported that early coronary angiography and percutaneous coronary intervention were performed significantly less often among SA, South-East Asian, and Chinese patients than those of European background. Further, research regarding general health care inequities among Canadian ethnic/racial minority groups has shown that, even in a universal-access system, disparities exist, such as access to renal transplantation or dialysis.26, 27 Researchers have suggested that racial identity–based differences in self-reported health status, which remain largely unexplained after adjustment for relevant demographic factors28 and the deteriorating health of immigrants following immigration,29, 30 may be due to the cumulative stress of frequent encounters with racism and discrimination in societal institutions28 and ethnic/racial bias or stereotyping in clinical encounters and decision making.31, 32 Although we acknowledge that this observational study cannot determine causality, we are encouraged by finding no racial identity–based differences in this aspect of ACS care, particularly so in spite of a high proportion of non–English-speaking participants in the Asian and SA groups, which might impede the triage process. Whereas other investigators have found differences in early ACS care,11, 25 we speculate that our findings may be related to the fact that, although 46% of our participants were not born in Canada, a high proportion (81%) had lived in Canada more than 10 years and thus would likely have been familiar with the Canadian health care system. Such familiarity might have increased these participants’ confidence during the clinical encounter, and perhaps clinicians’ perceptions of them as “good patients,”33 both of which could have led to equitable care. As well, there was a generally high level of education across all groups that may have improved communication and health literacy.
Although racial biases were not evident in our findings, unfortunately there were significantly longer D2ECG times among women (p = 0.036) and those who spoke English at home, in our adjusted model. Women are more likely to present later and to have vague symptoms,34, 35 both of which could lead to a prolonged triage process. Reinforcing this notion, women experience a longer diagnostic phase after presenting with symptoms of ACS.36, 37 Indeed, in our study, a smaller proportion of women reported chest pain the main symptom, which may at least partially explain their observed longer D2ECG times.
Those who reported speaking a language other than English at home had shorter D2ECG times, which was initially surprising. However, a possible explanation for this is that, because verbal communication would likely have been difficult in this English-speaking clinical environment, this may have paradoxically sped up acquisition of the ECG by cutting short the assessment phase. The triage nurse may simply have erred on the side of caution if there were any suggestion of serious symptoms.38
Finally, in all groups, the D2ECG times exceeded the recommended time of 10 minutes. Quality improvement approaches and vigilance are required to achieve and sustain these targets.
Limitations
We recruited daytime patients with potential ischemic chest pain (not ACS) and most patients were deemed lower acuity, so our findings cannot be generalized to critically ill patients or those attending at night. To mitigate the Hawthorne effect, the study sites’ ED staff and physicians were blinded to the true purpose of our study. Therefore, we could not collect information about staff racial identity/ethnicity, their perception of patients’ racial identity, or their years of experience, all of which could have influenced any care processes. Instead, we asked participants what racial background other people tend to think they are, as a proxy for the staff's perceptions. Although participants self-reported their racial identity, we then recategorized their responses into four groups, to achieve sufficient statistical power, and this may have obscured some racial variation in our sample. To mitigate this, we also collected data on “immigration status” (i.e., whether born in Canada and length of residency), to further characterize our sample. Based on census data, we are confident that the majority of those not belonging to the Asian or South Asian group were of European background.24
We were only able to recruit participants who were fluent in English, Mandarin/Cantonese, and Punjabi. As a result, the diversity of the sample may have been compromised. Because we could not collect racial identity or other clinical or demographic information from those who did not consent to participate, we have only age and sex data about those who were initially eligible but not recruited, which were similar to those who were recruited. However, noting that a significant proportion of immigrants in our sample had been in Canada more than 10 years, our findings cannot be generalized to recent immigrants. While EDs can have variable levels of crowding, all sites declared that triage nurse positions are always filled and electrocardiographic technicians are always available, so the provision of ECGs should be reasonably independent of any crowding metrics. The interview tool has not been validated; however, some items have been used and validated by Statistics Canada, as described.
Conclusion
We are cautiously encouraged that no racial identity–based differences in initial ED care were found in this sample of patients presenting with possible acute coronary syndrome, which may be partially explained by the high proportion of participants who had lived in Canada for more than 10 years. This fact may have increased their knowledge and confidence in using the health system, which, in turn, could have tempered potential unconscious bias among health professionals. However, we acknowledge that this does not mean that such bias among health professionals, based on patients’ racial identity, does not exist in the initial care of acute coronary syndrome patients—only that it was not found here, as measured by door-to-electrocardiogram. The poorer door-to-electrocardiogram performance afforded to female patients remains a concern.
We acknowledge the assistance of the emergency department nursing staff in all study sites in the conduct of this study. We also acknowledge the high-quality work of Diana Kao and Mary O'Sullivan and numerous research staff during the course of this study. Finally, we thank the patient participants for giving generously of their time.