Mediastinal venolymphatic malformations mimicking thymic carcinoma
Abstract
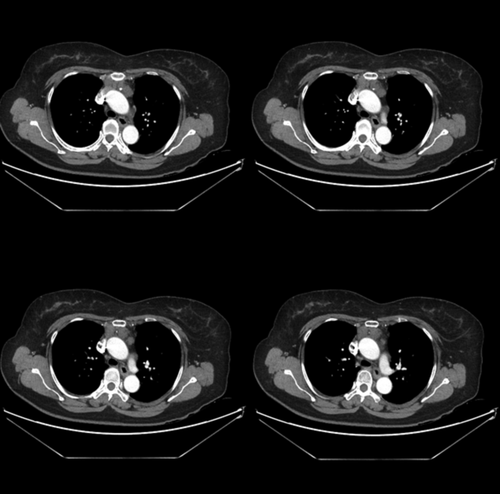
This report was about a 60-year-old asymptomatic female patient who presented to our clinic with an anterior mediastinal mass found on routine chest computed tomography (CT). Chest CT revealed an irregular poorly enhanced anterior mediastinal mass which showed signs of infiltration to adjacent structures with sparse calcifications. The preliminary diagnosis was thymic carcinoma. The patient underwent extended thymectomy via median sternotomy and complete excision of the tumor. A small draining vein to the left brachiocephalic vein and phleboliths were identified in the tumor. A definitive diagnosis was made of mediastinal venolymphatic malformation (VLM). The patient had an uneventful clinical course and was discharged without further complication. This report highlights that it is possible to misdiagnose mediastinal VLM as thymic carcinoma and could serve as a useful reminder to physicians in the future.
Introduction
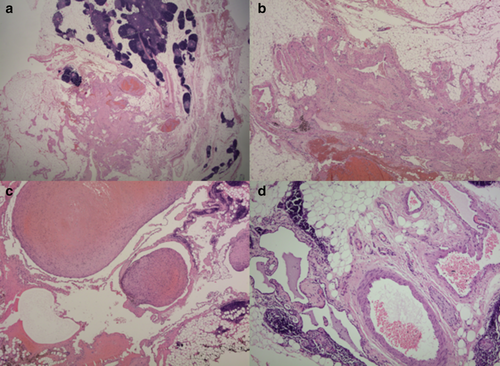
Mediastinal venolymphatic malformation (VLM) is a rare disease which was first described in 1983 by Angtuaco et al.1 A total of 13 cases have so far been identified in the English literature to date.2 In the report by Mahendra et al. VLM was considered to be vascular dysplasia, which contained both venous and lymphatic components. Microscopic view shows dilated spaces surrounded by endothelium, which was stained for either podoplanin (indicating lymphatics) or CD34 (indicating blood vessels).3 The etiology and pathogenesis of VLM has remained unknown until present, although there have been a few reports that support abnormality at the stage of vasculogenesis.4 The presentation of mediastinal VLM varies depending on the proportion of lymphatics and venous elements on imaging. This report describes a case of VLM with carcinoma-like infiltration to the adjacent structures which was successfully treated with surgical resection.
Case report
A 60-year-old female presented to the thoracic surgery department with a history of an anterior mediastinal mass. She was a 14-pack-year smoker but denied history of any recent trauma or significant disease. A chest CT scan revealed a poorly enhanced anterior mediastinal mass, with signs of infiltration to the adjacent structures with sparse calcifications (Fig 1). No lymphadenopathy or other mass lesions were identified. The preliminary diagnosis was thymic carcinoma. The patient subsequently underwent extended thymectomy via median sternotomy, complete excision of the tumor and lymph node dissection. The lesion was resected and frozen section biopsy revealed mediastinal VLM. The lesion showed a fragment of yellowish gray soft tissue, measuring 6.5 × 6.0 × 3.5 cm. Gross and microscopic features of the lesion are described in Figure 2. The patient had an uneventful clinical course and was discharged without further complication.
Discussion
VLMs were previously called lymphangiohemangiomas, which could be classified into lymphatic and venous malformations.5 Patients may be asymptomatic or diagnosed with cough, chest pain, hemoptysis, or venous varicosities. In the report by Kadota et al. magnetic resonance imaging (MRI) and multidetector row computed tomography (MDCT) angiography were useful for the diagnosis of mediastinal VLM because they could effectively detect slow-flow components and small vessels such as venous connections to the superior vena cava.2 Immunohistochemical-staining pattern was positive for podoplanin or CD34 and surgical resection was the treatment choice in all 13 cases and was curative and successful without any recurrence in all 13 patients.2 Our case study was unique because the 60-year-old patient presented an unusual radiologic findings of tumor-like anterior mediastinal mass which could have been misdiagnosed as thymic carcinoma. The treatment is consistent with those of previous studies with a satisfactory outcome. Our report may serve as a reminder that mediastinal VLM might be considered in the differential diagnosis of a mediastinal mass with infiltration to adjacent organs, although it is a rare disease and the best treatment option for mediastinal VLM could be surgical resection.
Disclosure
No authors report any conflict of interest.