Complete remission of liver metastasis in a lung cancer patient with epidermal growth factor mutation achieved with Icotinib
Abstract
A 65-year-old Chinese male was referred to our hospital for epidermal growth factor receptor (EGFR)-mutated advanced non-small cell lung cancer (NSCLC). Aggressive combined therapy with surgical resection of the right upper lung lesion and chemotherapy was performed. One month later, continued Icotinib treatment was used as magnetic resonance imaging revealed liver metastasis (LM). Interestingly, complete remission of the patient's LM lesions was achieved in six months. To our knowledge, this is the first report documenting a successful case of an NSCLC patient with LM treated with Icotinib after receiving a radical resection for pulmonary carcinoma. Our experience could provide a treatment strategy for patients with similar disease.
Introduction
Cancer is the leading cause of death worldwide, with about 20% related to lung cancer. The most common extra-pulmonary sites of distant metastasis in non-small cell lung cancer (NSCLC) patients are the brain, bone, adrenal gland, and liver. In the past decade, epidermal growth factor receptor-tyrosine kinase inhibitors (EGFR-TKIs) have become widely used for the treatment of advanced NSCLC. However, the effect of EGFR-TKI treatment in patients with EGFR-mutated lung adenocarcinoma with liver metastasis (LM) after surgical resection of the lung cancer lesions is unclear.
Case report
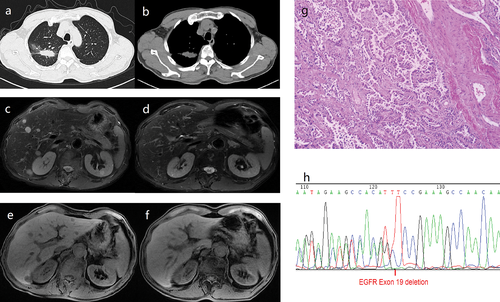
In February 2015, a 65-year-old asymptomatic male smoker was admitted to our hospital, after being diagnosed with lung cancer at Sir Run Run Shaw Hospital. The patient denied any other medical history. On hospital admission, physical examination and laboratory test results were normal. A chest computed tomographic scan revealed an oblong lesion in the right upper lobe of the lung measuring 3.4 cm × 1.6 cm × 2.1 cm and the right hilar lymph nodes were enlarged (Fig1a,b). Bronchoalveolar lavage was performed and histopathologic examination indicated NSCLC. No distant metastases were found outside the lung during examination. After obtaining the patient's informed consent, a radical resection of the right upper pulmonary carcinoma and mediastinal lymph node dissection by video-assisted thoracic surgery was performed. Histopathologic examination showed a 3.0 cm × 2.0 cm middle to well-differentiated adenocarcinoma of the right upper lobe (Fig 1g). Thirty-eight resected lymph nodes were detected and 10 were positive. The right upper lobe lesion carried an EGFR exon 19 deletion (Fig 1h). According to the 2015 National Comprehensive Cancer Network guidelines for NSCLC, chemotherapy was intravenously administered (pemetrexed 800 mg day 1 + cisplatinum 40 mg days 2–3) after the surgery. However, in March 2015, magnetic resonance imaging (MRI) revealed multiple lesions detected in the liver, which were considered to be metastases (Fig 1c,e). Considering that the right upper lung cancer was positive for EGFR mutations, the patient began treatment of 375 mg Icotinib daily, from March 2015. Interestingly, after six months of therapy, liver MRI showed that the multiple lesions had vanished (Fig 1d,f). The patient is currently receiving maintenance Icotinib treatment and no new metastases have been found in 16 months.
Discussion
The incidence of LM in NSCLC patients is 20–40%.1, 2 Patients with an EGFR mutation tend to have synchronous LM.3 For the past few years, many trials have demonstrated that advanced NSCLC patients with EGFR mutations could clinically benefit from receiving first-line treatment with EGFR-TKIs, such as afatinib, gefitinib, or erlotinib.4-6 Nevertheless, in stage IV lung adenocarcinoma patients, LM predicts poorer PFS and OS, despite treatment of susceptible gene mutations with first-line EGFR-TKIs.7 Although patients with liver metastasis on initial diagnosis have shorter PFS and OS than patients without liver metastasis, they could also benefit from first-line treatment with EGFR-TKIs. To our knowledge, no case of LM lesions in an NSCLC patient achieving complete remission by Icotinib treatment after radical resection of pulmonary carcinoma has previously been reported.
Following a traditional therapeutic method, the patient may receive chemotherapy, radiofrequency ablation, or transcatheter arterial chemoembolization after undergoing radical resection of pulmonary carcinoma. However, because the tumor was positive for an EGFR mutation of exon 19 deletion in our case, we developed a strategy that involved continued Icotinib treatment for the liver lesions after radical resection of the pulmonary carcinoma.
Early clinical data has shown that EFGR-TKIs, including icotinib, gefitinib, and erlotinib, are mainly metabolized in the liver. Liver dysfunction may contribute to drug overexposure.8-10 Thus, it could be hypothesized that drug overexposure may lead to the higher curative effect of EGFR-TKIs in patients with liver dysfunction caused by LM.
In our case, the patient underwent radical resection of the pulmonary carcinoma before receiving EGFR-TKI treatment. It could be hypothesized that resection of the pulmonary carcinoma leads to a higher curative effect of EGFR-TKIs, as it lightens the tumor load on the patient; however, further study needs to be conducted to confirm this hypothesis.
This case demonstrated the curative effect of EGFR-TKIs for NSCLC patients with LM, after radical resection for pulmonary carcinoma. Doctors could consider this treatment strategy for patients with similar disease. To date, the patient is still alive, receiving Icotinib treatment, with no further metastasis. Further study is warranted.
Disclosure
No authors report any conflict of interest.