Lung adenocarcinoma with anomalous bronchi and pulmonary veins preoperatively identified by computed tomography
Abstract
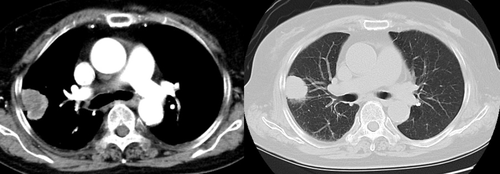
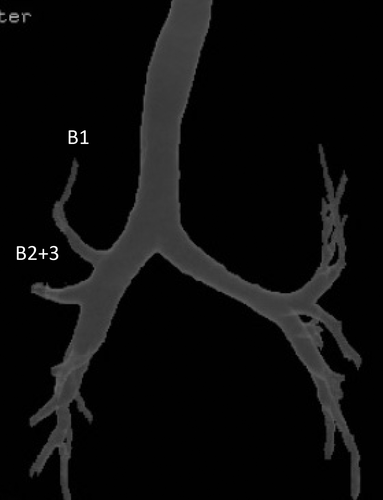
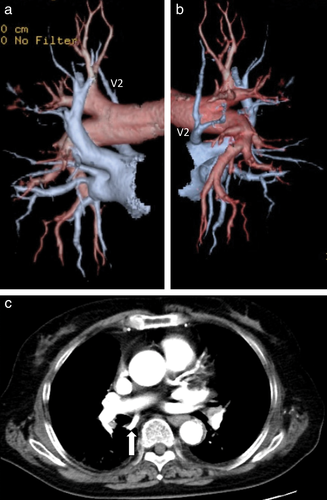
A 69-year-old woman visited our hospital complaining of right chest pain. Chest computed tomography showed a 55 × 45 mm tumor in the right upper lobe. Bronchoscopy revealed displaced anomalous B 1 and B 2 +3 arising from the right main bronchus, and the patient was diagnosed with lung adenocarcinoma by transbronchial lung biopsy from the displaced B 2 +3. Three-dimensional computed tomography with multiplanar reconstruction revealed a displaced anomalous B 1 and B 2 +3 branching directly from the right main bronchus, respectively, and abnormal distribution of the aberrant pulmonary vein (V 2) descended dorsally to the right main bronchus and emptied into the left atrium. Video-assisted right upper lobectomy with nodal dissection was successfully performed. Attention should be paid to the anomalous bronchus and pulmonary vessels for safer lung cancer operations, especially for video-assisted thoracic surgery.
Introduction
With the widespread use of bronchoscopy and the remarkable progress of recent three-dimensional-computed tomography (3DCT), identification of bronchial abnormalities has become quite common, while variant pulmonary veins are relatively rare.1 Preoperative recognition of anomalous bronchi or pulmonary vessels is very important for a safe operation, because anatomical variations can cause difficulty, especially in video-assisted thoracic surgery (VATS). This report documents the surgical case of a 69-year-old woman suffering from lung cancer who demonstrated an anomalous bronchi (B1 and B2 +3) branching from the right main bronchus and whose pulmonary vein (V2) independently drained directly into the left atrium. To the best of our knowledge, six reported cases of lung cancer, including the present case, have been associated with this type of pulmonary vein anomaly. This report profiles the third case accompanied by bronchial variations.
Case report
A 69-year-old woman visited our hospital complaining of right chest pain. CT showed a pulmonary tumor of 55 × 45 mm in the right upper lobe (Fig 1). Bronchoscopy revealed displaced anomalous B1 and B2 +3 arising from the right main bronchus, and a transbronchial lung biopsy from the displaced bronchus was diagnosed as adenocarcinoma. 3DCT with multiplanar reconstruction also revealed displaced anomalous B1 and B2 +3 branching directly from the right main bronchus (Fig 2), and an abnormal distribution of the aberrant pulmonary vein (V2) descended dorsally to the right main bronchus and emptied into the left atrium (Fig 3). No abnormal distribution was found in the pulmonary artery. The patient was diagnosed with primary lung adenocarcinoma (c-T2bN1M0) located in the right S3 with displaced B1 and B2 +3 and abnormal distribution of the aberrant pulmonary vein. A video-assisted right upper lobectomy was performed with a 7 cm access window and three ports. From the anterior aspect of the hilum, V1 +3 without the central vein (V2) was divided using a vascular endostapler. An anomalous vein (V2) was identified behind the right main bronchus at the posterior aspect of the hilum that independently drained directly into the left atrium and was divided using a vascular endostapler. The displaced B1, B2 +3, A2, A1 +3, and interlobar fissure were sequentially divided, and the right upper lobe was removed. Hilar and mediastinal lymph node dissection was performed. The postoperative course was uneventful. Pathological diagnosis was adenocarcinoma with a maximal diameter of 55 mm with #4R and #12u node metastases (pT2bN2M0).
Discussion
Recently, VATS has become a widespread procedure among thoracic surgeons as a potential alternative to conventional thoracotomy because of its clinical benefits, less postoperative pain, and quicker recovery following surgery.2 However, the vessels, bronchi, and interlobar fissures are dissected using a thoracoscope with less tactile feedback with a two-dimensional vision, which occasionally might lead to serious complications, especially in patients with anomalous pulmonary vessels, as bleeding from an unknown origin could cause a critical situation. Tsuboi et al. reported that one of the causes of conversion to thoracotomy during VATS could be an anomalous hilar structure, as well as dense pleural adhesion, difficulty in safely dissecting the interlobar pulmonary artery, or bleeding from vessels.3 Indeed, Asai et al. reported that one of nine right thoracotomy patients with a right upper lobe vein posterior to the bronchus intermedius suffered venous injury, and the patient's anomalous vein was not identified either preoperatively or intraoperatively.1 They further demonstrated that in 5.7% of the patients studied, the pulmonary vein branch of the right upper lobe posterior to the bronchus intermedius was observed. According to the five previous case reports with anomalous V2, it was recognized preoperatively in only two cases.3-7 Akiba et al. reported the importance of preoperative 3D imaging for a safe operation because variations in pulmonary vessels can have a serious impact on patients undergoing lung surgery, especially in VATS.8
Moreover, our patient also presented anomalous bronchi (B1 and B2 +3) branching from the right main bronchus. Although only a few surgical cases of lung cancer with anomalous vein accompanied by bronchial variations have been reported, as these abnormalities may be complicated, surgeons should pay attention to their possible presence, not only on preoperative images but also intraoperatively.5, 7
In this case, one of the important factors in a successful VATS lobectomy is preoperative foreknowledge of anomalous vessels and bronchi. For the safe completion of a VATS lobectomy, a cautious preoperative evaluation of the anatomical structures, as well as of the tumor itself, to identify any abnormal vascular or bronchial distribution is essential.
Disclosure
No authors report any conflict of interest.