Postoperative chemoradiotherapy improves survival in patients with stage II–III esophageal squamous cell carcinoma: An analysis of clinical outcomes
Abstract
Background
We compared the efficacy of postoperative chemoradiation (POCRT) and surgery alone (SA) in patients with stage II–III esophageal squamous cell carcinoma (ESCC).
Methods
We analyzed the records of 265 patients with stage II–III ESCC who had undergone transthoracic esophagectomy and lymphadenectomy; 105 patients received POCRT, while 160 had SA.
Results
The median disease-free survival (DFS) of the whole cohort was 22 months (95% confidence interval [CI], 19.2–24.8), while the median overall survival (OS) was 29 months (95% CI 25.5–32.5). The median DFS of the SA group was 21 months (95% CI 17.9–24.0), while that of the POCRT group was 29 months (95% CI 18.8–31.2; P = 0.048). Consistently, patients in the POCRT group had significantly longer median OS than patients in the SA group (34 vs. 26 months, respectively). Subgroup analysis showed that in patients with positive lymph nodes, pathological stage III, T3–4 stage, and poorly differentiated carcinoma, POCRT was apparently more effective than SA at improving OS and decreasing the rates of local recurrence and distant metastasis. Multivariate analysis demonstrated that lymph node involvement and treatment with POCRT were independent prognostic factors.
Conclusion
Compared with SA, POCRT may be more effective in improving OS and decreasing the rates of local recurrence and distant metastasis, particularly in stage III or positive lymph node stage II–III ESCC patients.
Introduction
Esophageal cancer patients with stage II–III disease who have undergone resection are often considered a subgroup with a poor prognosis – even those treated with curative esophagectomy are still at a high risk for both local and distant recurrence.1, 2 Although neoadjuvant treatments, including preoperative chemoradiotherapy and chemotherapy, have been evaluated for esophageal adenocarcinoma, there are obvious differences in the biological, epidemiological, and clinical characteristics, as well as in the treatment methods between adenocarcinoma and squamous cell carcinoma (SCC).3 In China, most esophageal cancer patients are first referred to a thoracic surgery department for complete resection, which is contrary to the treatment modality recommended by National Comprehensive Cancer Network (NCCN) guidelines (version 1, 2015) for esophageal adenocarcinoma. The issue of whether to add chemoradiotherapy to esophageal squamous cell carcinoma (ESCC) treatment after surgery is still under investigation.4 Because of the lack of clinical research data and standard therapeutic modes, the role of adjuvant therapy in resected ESCC patients is unknown. The optimal treatment modality and the subgroup of patients that will most benefit are controversial issues.
Recently, the benefits of postoperative chemotherapy (POCT) for disease-free survival (DFS) and postoperative radiotherapy (PORT) on survival have been confirmed in several large clinical trials of SCC patients with positive lymph nodes. Previous reports have revealed that PORT was associated with better survival in patients with node-positive thoracic ESCC.5, 6 Although postoperative chemoradiotherapy (POCRT) may be accompanied by increasing side effects, it is more efficacious, in theory, than POCT in eliminating local residual tumor and micro metastasis than PORT or chemotherapy alone.7 However, the effect of combining adjuvant radiotherapy with chemotherapy on the survival of patients with ESCC requires further study. As the NCCN guidelines do not currently provide a recommendation, patients who have undergone esophagectomy are generally treated with POCT and PORT, whereas PORCT is emphasized primarily for patients with SCC after surgery by some centers, particularly departments of thoracic oncology or radiotherapy. Previous results have revealed that PORT and POCT may improve ESCC patient survival in China, where SCC is most common.8, 9 According to research data, adjuvant chemoradiotherapy is prescribed as part of the treatment for SCC patients in China.
A number of reports have concluded that POCRT improves survival.6, 10, 11 Liu et al. reported that even after combined adjuvant therapy, 31.7–41.8% of patients with positive nodes experienced local tumor recurrence and 23.2% distant metastasis.12 However, further investigation is warranted for new therapeutic regimens and modalities for ESCC patients with stage II and III disease, because of the lack of studies focusing on this stage of ESCC.
The benefits of POCRT need to be clarified in a cohort of patients with stage II and III disease. In this retrospective study, we considered that earlier studies varied in design and selection criteria, although the results were generally uniform. Data from a cohort of patients with stage II and III ESCC who underwent complete resection from West China Hospital were reviewed and analyzed. We aimed to assess the survival benefit of POCRT by comparing it with surgery alone (SA). We have identified factors contributing to poor prognosis in patients with stage II and III ESCC after tumor resection.
Methods
Patient characteristics
From January 2006 to December 2011, the data of 511 patients was screened. The selection criteria were as follows: (i) stage II–III ESCC (American Joint Committee on Cancer 7th edition); (ii) patients who had undergone complete dissection and system mediastinal lymphadenectomy; (iii) patients who received POCRT or SA; (iv) patients aged 18–80; and (v) patients with a Karnofsky performance status score of more than 70. Exclusion criteria included: POCRT patients who received radiation therapy of less than 40 Gy or less than two cycles of chemotherapy; patients with other malignancies; patients who experienced severe adverse events or complications of surgery; patients with any serious concurrent disease, such as severe diabetes, uncontrolled hypertension, serious chronic obstructive pulmonary disease, or any residual tumors; and patients who survived less than 30 days after surgery.
The final sample included 265 patients who had received R0 resection at West China Hospital, Sichuan University, from January 2006 to December 2011. All of the patients had pathologic stage II–III ESCC, and 105 received postoperative treatment that combined chemotherapy and radiotherapy. Forty-eight patients received sequential chemoradiotherapy, 57 received concurrent POCRT, and 14 received consolidation chemotherapy after POCRT. The treatment mode was determined by the physician, with some consideration of the economic circumstance of the patient.
Follow-up was conducted from the commencement of treatment every three months within the first two years, every six months in the third year, and annually in the fourth year. The median follow-up was 49 months; the average follow-up of patients lost to follow-up was 55.4 months. We reviewed survival, time of disease progression, and the date of death or last follow-up, as well as the details of treatment, tumor stage, gender, and age. Patient age at surgery ranged from 41 to 80 years, with a median age of 60 (62 years in the SA and 57 in the POCRT group). Except for the percentage of people who drink (P = 0.020) and positive lymph nodes involved (P = 0.003), the remaining characteristics did not differ significantly between the two groups. The clinical characteristics between the two groups are listed in Table 1. The interval between surgery and the start of postoperative therapy ranged from 16 to 83 days (median 28 days).
| Characteristic | S No. (%) | POCRT No. (%) | χ2 | P value |
|---|---|---|---|---|
| Gender | ||||
| Male | 128 (80.0) | 86 (81.9) | 0.148 | 0.752 |
| Female | 32 (20.0) | 19 (18.1) | — | — |
| Age (years) | ||||
| ≤ 60 | 74 (46.3) | 60 (57.1) | 3.009 | 0.102 |
| > 60 | 86 (53.7) | 45 (42.9) | — | — |
| Drinking | ||||
| Yes | 107 (66.9) | 84 (80.0) | 5.462 | 0.020 |
| No | 53 (33.1) | 21 (20.0) | — | — |
| Smoking | ||||
| Yes | 104 (65.0) | 78 (74.3) | 2.541 | 0.136 |
| No | 56 (35.0) | 27 (25.8) | — | — |
| Tumor location | ||||
| Upper | 16 (10.0) | 10 (9.5) | 2.706 | 0.120 |
| Middle | 67 (41.9) | 59 (56.2) | — | — |
| Lower | 77 (48.1) | 36 (34.3) | — | — |
| Pathological stage | ||||
| II | 79 (49.4) | 42 (40.0) | 2.246 | 0.165 |
| III | 81 (50.6) | 63 (60.0) | — | — |
| Tumor differentiation | ||||
| G1 | 4 (2.5) | 0 (0) | 0.562 | 0.477 |
| G2 | 67 (41.9) | 44 (41.9) | — | — |
| G3 | 89 (55.6) | 61 (58.1) | — | — |
| LN involved | ||||
| N− | 85 (53.1) | 36 (34.3) | 9.069 | 0.003 |
| N+ | 75 (46.9) | 69 (65.7) | — | — |
| pT stage | ||||
| T1–2 | 54 (33.8) | 25 (23.8) | 2.994 | 0.084 |
| T3–4 | 106 (66.2) | 80 (76.2) | — | — |
| No. of resected nodes | ||||
| ≤ 14 | 92 (57.5) | 64 (60.9) | 0.312 | 0.576 |
| > 14 | 68 (42.5) | 41 (39.1) | — | — |
- G, histopathological grading; LN, lymph nodes; No., number; POCRT, postoperative chemoradiotherapy; pT, pathological tumor stage.
Surgery
In our analysis, thoracic surgeons with at least 10 years of surgical experience performed two or three-field lymph node dissections by right or left thoracotomy esophagectomy and mediastinal lymphadenectomy dissection. Systematic and complete dissection of the mediastinal lymph nodes was performed in all of the patients for curative intent, while perigastric lymph node resection was carried out in patients with tumors located in the middle or lower thorax.
Postoperative chemotherapy
One hundred and five patients received platinum-based chemotherapy with a median of four cycles (range 2–6), combined with radiotherapy. Sixty-seven patients received a median of four cycles (range 2–6) of cisplatin (25 mg/m2 intravenously on days 1–3), fluorouracil (750 mg/m2 intravenously on days 1–5) and leucovorin (200 mg/m2 intravenously on days 1–5) of. Thirty-eight patients received a median of four cycles (range 3–6) of paclitaxel (135 mg/m2 intravenously on day 1) and cisplatin (25 mg/m2 intravenously on days 1–3). The length of each cycle of the various chemotherapy regimens was 21 days.
Postoperative radiotherapy
Of the 265 patients, 105 received PORT. Radiation was delivered with 6-MV X rays at a dose of 40–50 Gy (median 50 Gy) in 1.8–2 Gy daily fractions applied five days per week. Sixty-three patients received three-dimensional (3D) computerized dosimetric planning and radiotherapy, while 42 received intensity modulated radiation therapy. The clinical target volume (CTV) for treatment generally encompassed the mediastinum (in terms of the anatomic landmarks of a perioperative computed tomography [CT] scan). The planning target volume (PTV) was determined as the CTV plus 0.8 cm margins. The radiation field extended from 4 cm beyond the tumor bed to the supraclavicular fossa, including the mediastinum. However, disease irradiation stemmed from the lower third of the esophagus with only the celiac node involved. The exact placement of the field borders differed from case to case according to the postoperative shift of mediastinal structures and the length of the lesion. Treatment commenced with administration to parallel-opposed anteroposterior fields of a total dose of 38–40 Gy using 3D conformal radiation therapy technology. Off-cord oblique or lateral fields were applied to the remaining dose to the tumor bed and mediastinum.
Definitions and statistical analysis
The minimal staging procedures for all of the patients included medical history and physical examination, barium swallow, bone scan, magnetic resonance imaging (MRI) of the brain, and chest and abdomen contrast CT. Cases were assigned a pathological staging in accordance with the AJCC Tumor Node Metastasis (TNM) Classification of Carcinoma of the Esophagus and Esophagogastric Junction (7th edition, 2010).
The long-term outcome was determined from medical records and follow-up information. Overall survival (OS) was calculated from the date of surgery to death or the last follow-up visit. DFS was measured from the date of surgery to the time of the first recurrence or metastasis, or death from any cause. Local recurrence was defined as tumor relapse in the organ of origin. Locoregional lymph nodes were visualized by CT scan or positive gastroscope. Recurrence beyond those sites was considered distant progression.
All statistical calculations were performed using SPSS 19.0 software (IBM Corporation, Armonk, NY, USA). OS and DFS rates were estimated by Kaplan–Meier method and the difference in survival rates between the two groups was assessed by log-rank test.13, 14 A Cox proportional hazards model was used to identify factors predictive of OS.13-15 The level of significance was P < 0.05.
Results
One hundred and ninety patients died, and the surviving patients were followed-up for a median of 49 months. Because of potential bias in the clinician's treatment selection, the percentage of patients who received POCRT was higher in the positive lymph node group (P = 0.003). The clinical characteristics between the two groups are shown in Table 1.
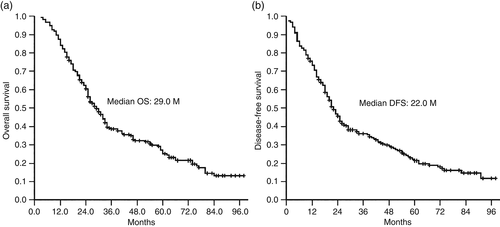
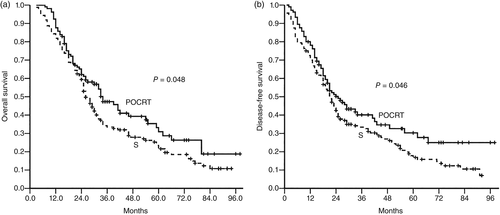
Overall and disease-free survival
The median DFS of the whole cohort of 265 patients was 22 months (95% CI 19.2–24.8), while the median OS was 29 months (95% CI 25.5–32.5). The median DFS of the SA group was 21 months (95% CI 17.9–24.0), while that of the POCRT group was 25 months (95% CI 18.8–31.2; P = 0.046). Analogously, patients in the POCRT group had significantly better survival than those in the SA group, with a median OS of 34 months (95% CI 26.1–41.9) in the POCRT group compared with 26 months (95% CI 23.4–28.6) in the SA group (P = 0.048, Fig. 1).
The overall recurrence rates (ORR), local recurrence rates (LRR), and distant recurrence rates (DRR) were compared between the two groups. There were notable differences in the ORR favoring the POCRT group (48.6% vs. 63.1%; P = 0.022). The LRR of the SA and POCRT groups were 52.5% and 39.0% (P = 0.033), respectively, while the DRR were 28.8% and 14.3% (P = 0.007), respectively.
Additional analysis was conducted for the 105 patients who received POCRT. The median OS between the concurrent chemoradiotherapy group and the sequential chemoradiotherapy group were 39 and 33 months (P = 0.915), respectively. There was no significant difference in DFS between the concurrent and sequential chemoradiotherapy groups (median DFS, concurrent vs. sequential: 27 vs. 24 months, P = 0.771).
Subgroup statistical analysis showed that, in patients with positive lymph nodes, pathologic stage III, and T3–4 stage, POCRT was much more effective than SA at improving OS and decreasing LRR and DRR. There was an obvious difference in OS and DFS between the SA and POCRT groups in stage III disease (median OS: 21 vs. 32 months; P = 0.000; median DFS: 13 vs. 21 months; P = 0.000, respectively). Moreover, for local recurrence-free survival (LRFS) and distant recurrence-free survival (DRFS) in the SA and POCRT groups, there were positive differences (median LRFS: 21 vs. 42 months; P = 0.000; median DRFS: 29 vs. n/a; P = 0.016, respectively). The same result was not observed in patients with negative lymph nodes, pathologic stage II, and pT1–2 (Table 2).
| Factor | SA group | POCRT group | P | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 1-year OS (%) | 3-year OS (%) | 5-year OS (%) | Median | 1-year OS (%) | 3-year OS (%) | 5-year OS (%) | Median | ||
| pT1–2 | 90.7 | 44.8 | 30.0 | 31.0 | 96.0 | 50.3 | 25.1 | 39.0 | 0.782 |
| pT3–4 | 77.4 | 27.5 | 17.3 | 25.0 | 85.0 | 46.9 | 34.6 | 32.0 | 0.016* |
| LN− | 92.9 | 52.8 | 34.2 | 41.0 | 91.7 | 65.6 | 54.1 | 62.0 | 0.353 |
| LN+ | 69.3 | 12.8 | 8.0 | 23.0 | 85.5 | 37.8 | 18.6 | 32.0 | 0.001* |
| G2 | 86.6 | 41.5 | 19.7 | 28.0 | 95.5 | 37.5 | 28.6 | 32.0 | 0.810 |
| G3 | 78.7 | 26.6 | 20.4 | 25.0 | 82.0 | 52.8 | 33.6 | 28.0 | 0.020* |
| II | 89.9 | 51.0 | 37.3 | 39.0 | 92.9 | 50.0 | 35.7 | 41.0 | 0.691 |
| III | 74.1 | 16.4 | 6.7 | 21.0 | 84.1 | 46.0 | 25.6 | 32.0 | 0.000* |
- * Statistically significant.
- II, pathological stage II; III, pathological stage III; G, histopathological grading; LN, lymph nodes; No., number; OS, overall survival; POCRT, postoperative chemoradiotherapy; pT, pathological tumor stage; SA, surgery alone.
Prognostic factors
Univariate analysis showed that OS was apparently associated with pT stage, the number of lymph nodes involved, the number of resected lymph nodes, pathological stage, and whether the patient received POCRT after surgery. The median DFS for these two groups was 40 months (95% CI 22.4–55.6) in patients without lymph node involvement (N−) and 18 months (95% CI 14.9–21.1) in those with positive node involvement (N+; P = 0.000). The median OS was 46 months (95% CI 30.9–61.0) in patients without node involvement (N−) and 25 months (95% CI 23.0–26.9) in those with lymph node involvement (N+; P = 0.000). Divergence existed in DRFS (P = 0.000) and LRFS (median P = 0.001) between patients without and with nodal involvement.
Multivariate analysis showed that lymph node involvement and whether a patient received POCRT after surgery (P = 0.002) were independent prognostic factors (Table 3).
| Variables | Overall survival | Disease-free survival | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P | HR | 95% CI | P | |
| Gender (male vs. female) | 0.763 | 0.507–1.148 | 0.195 | 0.853 | 0.571–1.275 | 0.438 |
| Age (≤60 vs. >60) | 1.116 | 0.823–1.512 | 0.481 | 1.046 | 0.773–1.414 | 0.772 |
| T stage (T1–2 vs. T3–4) | 1.118 | 0.752–1.663 | 0.581 | 1.115 | 0.751–1.657 | 0.588 |
| Regimen (POCRT vs. SA) | 0.573 | 0.420–0.782 | 0.000* | 0.555 | 0.408–0.756 | 0.000* |
| Drinker (yes vs. no) | 0.855 | 0.549–1.333 | 0.490 | 0.939 | 0.615–1.435 | 0.939 |
| Smoker (yes vs. no) | 1.105 | 0.741–1.648 | 0.625 | 1.094 | 0.743–1.609 | 0.649 |
| Stage (II vs. III) | 1.606 | 1.148–2.246 | 0.006* | 1.630 | 1.175–2.262 | 0.003* |
| LN involved (N− vs. N+) | 1.972 | 1.403–2.771 | 0.000* | 2.030 | 1.458–2.826 | 0.000* |
| Number of resected LN (≤14 vs. >14) | 1.059 | 0.765–1.466 | 0.732 | 1.220 | 0.888–1.677 | 0.220 |
| Tumor location (up vs. mid vs. L) | 0.969 | 0.750–1.252 | 0.809 | 1.075 | 0.836–1.381 | 0.574 |
| Tumor differentiation (G1 vs. G2 vs. G3) | 1.186 | 0.893–1.575 | 0.239 | 1.139 | 0.861–1.508 | 0.362 |
- * Statistically significant.
- CI, confidence interval; G, pathological grade; HR, hazard ratio; L, lower; LN, lymph nodes; mid, middle; POCRT, postoperative chemoradiotherapy; SA, surgery alone; up, upper.
Toxicity
Gastrointestinal reactions including nausea, emesis, diarrhea, and poor appetite, were the most common toxic reactions in the POCRT group, occurring in 89 patients (84.8%). Neutropenia, which occurred in 87 patients (82.9%), was the second most common complication, with 68 patients (64.8%) at Grade 1–2 and 19 patients (18.1%) at Grade 3–4; one patient suffered febrile neutropenia (Table 4). There were no adjuvant treatment-related toxic deaths.
| Reactions | Number (105) | Percent |
|---|---|---|
| Gastrointestinal reactions | 89 | 84.8 |
| Grade 1–2 | 83 | 79.0 |
| Grade 3–4 | 6 | 5.7 |
| Decreased energy | 43 | 40.9 |
| Neutropenia | 87 | 82.9 |
| Grade 1–2 | 68 | 64.8 |
| Grade 3–4 | 19 | 18.1 |
| Thrombocytopenia | 13 | 12.4 |
| Grade 1–2 | 9 | 8.6 |
| Grade 3–4 | 4 | 3.8 |
| Radiation esophagitis (grade 3–4) | 3 | 2.9 |
| Radiation pneumonitis (grade 3–4) | 2 | 1.9 |
| Radiation skin damaged (grade 3–4) | 2 | 1.9 |
| Muscular soreness (grade 1–2) | 47 | 44.8 |
| Other | 6 | 5.7 |
- POCRT, postoperative chemoradiotherapy.
Discussion
In our analysis, OS and DFS were obviously improved in patients who received POCRT compared with the group who received SA. The survival advantage associated with POCRT in our analysis was similar to that of previous reports.16-18 POCRT significantly reduced the LRR and DRR, leading to substantially improved DFS and OS, compared with the SA group.6, 10, 11, 19-21 As shown in Figure 2, the survival curves of patients receiving POCRT and SA showed clear divergence from 20 months. This result suggests that the benefit of greater OS was achieved by POCRT from almost 20 months because of the decrease in LRR and DRR. A similar effect of POCRT has been reported in other analyses of patients with ESCC.11, 20, 21 The authors in these studies concluded that late effects, such as a decrease in local recurrence (which often leads to death) might be the main mechanism of the notable improvement in OS, a finding partly consistent with ours. However, further effects of POCRT could not be revealed because the number of cases in these analyses was relatively small. In our study, there was a substantial difference in the DRR between the POCRT and SA groups, and the POCRT group experienced an improved distant control rate and further improved DFS and OS. A previous study suggested that patients with stage III–IV disease could benefit from adjuvant chemotherapy regarding three-year OS, but not patients with stage I–II disease (relative risk 1.12, 95% CI 0.65–1.93; P = 0.68).9 Our subgroup analysis showed that patients with stage III ESCC who received POCRT had apparently more optimized survival benefits than those with stage II disease, possibly because POCT is more often performed in patients with stage III disease.9
Patients with lymph node-positive ESCC endured high rates of local and systemic failure. Thus, PORT and POCT are used after radical surgery to improve outcomes. Although there is no general recommendation, prophylactic radiotherapy after radical surgery could reduce local recurrence.6, 9-11, 19-21 In the present analysis, positive lymph nodes were a prognostic factor in multivariate analysis for all of the patients. Patients who were node negative had a greater DRFS and greater improvement in both DFS and OS, compared with those who were node positive. Previous studies demonstrated similar results.6, 9, 19 The distinction for both groups was obvious for five-year survival because even those node-positive cases that had undergone curative esophagectomy were still at high risk for both local and distant recurrence.1, 2 POCRT could decrease the ORR from the day of treatment. Ténière et al. reported that PORT improved the local control rate from 15–30%, but there was no survival benefit.22, 23 However, previous PORT technology (2D rather than 3D) may be associated with increased death from intercurrent diseases, which offset the survival benefits of radiation. A recent study reported that, compared with SA patients, patients with lymph node-positive ESCC receiving POCRT had better survival using modern technology – results that were similar to ours.9, 21
Death in patients with ESCC is commonly attributed to cancer-associated diseases, such as cachexia, rather than a direct result of the cancer. In our study, there were no adjuvant treatment-related toxic deaths. Nineteen patients (18.1%) experienced Grade 3–4 neutropenia, and only one of these experienced febrile neutropenia. Recently, researchers have found that PORT presented no significant difference to the incidence of late toxic reactions using advanced techniques.19 In our study, PORT was delivered to all patients via a linear accelerator and did not result in obviously increased radiation pneumonitis, although the POCRT group had a 1.9% incidence of grade 3–4 disease. Our analysis has shown that the addition of POCRT with modern technologies will decrease local recurrence with acceptable side effects.
In conclusion, compared with surgery alone, postoperative chemoradiation may be more effective at increasing OS and decreasing the rates of local recurrence and distant metastasis, particularly in stage III or lymph node-positive stage II–III ESCC patients. Considering that potential bias may exist in this study, larger, prospective randomized clinical trials are needed to confirm these findings.
Acknowledgment
Supported in part by a grant from the National Natural Science Foundation (NNSF) of China (No. 81301907).
Disclosure
No authors report any conflict of interest.