Thoracoscopic tracheal reconstruction without surgical field intubation
Abstract
A cross-filed endotracheal intubation is usually applied to maintain single lung ventilation during both open and thoracoscopic tracheal resection and reconstruction. Herein, we report a case of thoracoscopic tracheal resection and reconstruction with interrupted ventilation via transoral endotracheal intubation in a patient with thoracic tracheal adenocarcinoma. Tracheal anastomosis was accomplished using a running suture with a 3-0 Prolene stitch.
Introduction
Surgical resection is the only curable choice for patients with tracheal malignancies.1 Surgery can be performed via thoracotomy for lesions of the thoracic trachea. Based on improved surgical techniques, thoracoscopic tracheal tumor resection with end-to-end anastomosis has become feasible and its use has been reported in a number of centers.2, 3 A surgical field endotracheal intubation is usually required to maintain ventilation when performing both open and thoracoscopic tracheal reconstruction. However, placing the intubation during thoracoscopic tracheal reconstruction is inconvenient as another port is required. Herein, we describe the use of interrupted ventilation with transoral intubation during a case of thoracoscopic tracheal resection and reconstruction.
Case report
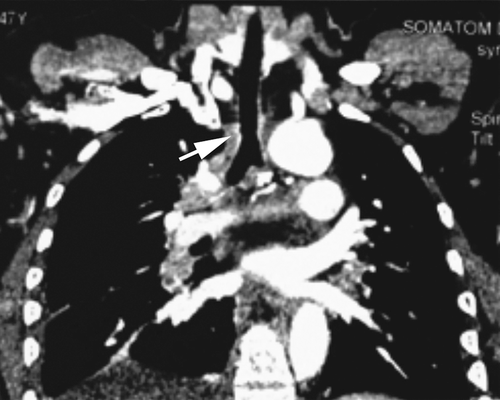
A 47-year-old female complained of cough with bloody sputum for two months. A computed tomography (CT) scan showed a 2.6 cm * 2.4 cm mass located 2.5 cm above the carina on the right posterior wall of the trachea (Fig 1). The lesion was diagnosed as tracheal carcinoma through transbronchoscopic biopsy. Given no surgical contraindications and the aesthetic needs, a total thoracoscopic tracheal tumor resection with end-to-end anastomosis was scheduled.
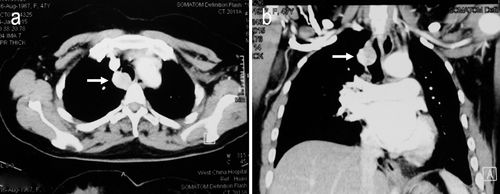
Chest computed tomographic image shows a mass in the lower trachea (arrow). (a) Axial view. (b) Coronal view.
The operation was conducted under general anesthesia. The endobronchial blocker was placed into the right main bronchus to achieve left single lung ventilation. The patient was placed in the left lateral decubitus position. A 1 cm observation port was made in the sixth intercostal space (ICS) on the midaxillary line. Two additional incisions were made: a 3 cm utility incision on the anterior axillary line in the third ICS, and a 2 cm assistant incision in the seventh ICS between the posterior axillary line and the subscapular line (Fig 2).
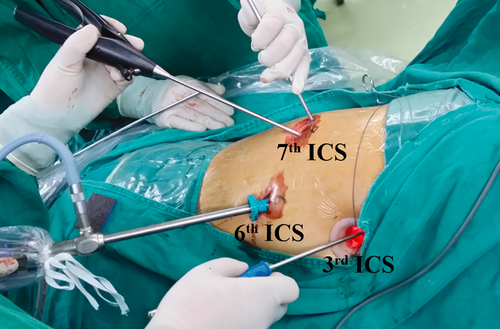
Distribution of the surgical ports. ICS, intercostal space.
After thoracoscopic inspection, the trachea was mobilized, combined with paratracheal lymph node dissection (Fig 3a). The inferior pulmonary ligament was then divided and a U-shaped incision was made on the pericardium to release the pulmonary veins. Two sutures were knotted on the trachea 1.5 cm away from the proximal and distal ends of the tumor for traction. The extent of tumor invasion was confirmed by the combination of thoracoscopic and intraoperative bronchoscopic vision. The trachea was transected 0.5 cm away from the margin of the tumor in the proximal and distal side, respectively. Six tracheal cartilage rings (3.5 cm) were removed to achieve a complete resection. The surgical margins were confirmed negative by intraoperative frozen section.
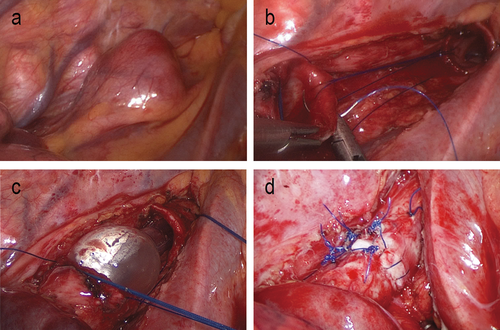
(a) Thoracoscopic view of the tumor. (b) Running suture without endotracheal intubation. (c) Ventilation during anastomosis. (d) Tracheal anastomotic stoma.
When the tumor was removed, the Univent tube was inserted into the distal stump of the trachea to achieve ventilation. The tube was drawn back temporarily when performing end-to-end anastomosis, and reinserted into the distal trachea when arterial oxygen saturation (SaO2) was less than 95% (Fig 3b,c). After re-intubation, the end-tidal carbon dioxide (ETCO2) level was less than 45 mmHg. Anastomosis was completed with a running suture using a 3-0 Prolene stitch. The left wall of the trachea was sewn up first, sequentially, followed by the anterior and posterior walls. The right wall was the final sewn. The two ends of the stitch were knotted (Fig 3d). A 28-Fr chest tube was placed after surgery.
The operation was accomplished within 200 minutes with 80 mL of blood loss. The chest tube was removed on postoperative day four. The patient's recovery was uneventful and she was discharged on postoperative day 11. Pathologic examination confirmed tracheal adenocarcinoma without lymph node involvement. CT scanning of the reconstructed trachea showed no stenosis at the one-month follow-up (Fig 4).
Computed tomographic scan of the trachea shows no stenosis (arrow) at one-month follow-up.
Discussion
Thoracotomy is the most commonly applied approach for surgical resection and reconstruction of thoracic tracheal tumors.1 However, video-assisted thoracoscopic surgery has recently been reported as an alternative approach for patients with tracheal tumors.2, 3 The key issues of this mini-invasive approach for tracheal surgery are airway management and reconstruction.
When performing tracheal sleeve resection, a cross-field endotracheal intubation of the main bronchus is usually applied to achieve single lung ventilation.4 This strategy was adopted in both of the previously reported cases of thoracoscopic tracheal surgery.2, 3 However, an additional port was required for this cross-field intubation during thoracoscopic surgery. Additionally, we found that it was inconvenient to carry out tracheal anastomosis with an intubation in the surgical field. Because of this complication, with the assistance of the anesthesiologist, we inserted the transoral intubation into the distal tracheal stump to keep SaO2 within a safe range. The tube was withdrawn into the proximal trachea when suturing, and no additional port was needed. With this method, we accomplished tracheal reconstruction with three surgical ports on the chest wall.
Tracheal anastomosis is the core step of thoracoscopic tracheal sleeve resection. Both interrupted and running sutures have been reported feasible during thoracoscopic bronchial reconstruction.5-7 We prefer running sutures for both bronchial and vascular sleeve resection via the thoracoscopic approach.7, 8 The most important advantage of a running suture is that this technique avoided suture winding. As in previously reported cases, we applied a running suture during this procedure.2, 3 Another important point to achieve a satisfactory anastomosis is the tension of the stoma. A 3.5 cm trachea was resected during surgery. In order to achieve a tension-free anastomotic stoma, we dissected the right inferior pulmonary ligament and made a U-shaped incision on the pericardium to release the hilar vessels.
In conclusion, thoracoscopic tracheal sleeve resection is safe and feasible. A transoral endotracheal intubation can be used as an alternative for cross-field intubation during tracheal reconstruction, not only avoiding the need for an extra port, but also making suturing easier and more convenient. However, the long-term outcomes of this mini-invasive approach for tracheal malignancies are yet to be confirmed.
Acknowledgments
This work was supported by the Key Science and Technology Program of Sichuan Province, P.R. China (2013SZ0005, 2014SZ0148).
Disclosure
No authors report any conflict of interest.