Effect of inhibition proliferation in human lung adenocarcinoma A549 cells by cytokine-induced killer cells
Abstract
Background
Adenocarcinoma, the most common form of lung cancer, is one of main human malignant tumors. In this paper, we focus on the effect of antitumor activity of cytokine-induced killer (CIK) cells on human lung adenocarcinoma cell line A549.
Methods
CIK cells were obtained by inducing peripheral blood mononuclear cells with recombinant human (rh) interferon-gamma, monoclonal anti-CD3 antibody, rh interleukin (IL)-1alpha, and rhIL-2, which were added into the culture. A549 cell viability of CIK cells was determined using MTS assay. Flow cytometry (FCM) experiments were performed to detect cell cycle changes. The expression of P27 in A549 cells treated by CIK cells was evaluated by Western blot.
Result
The percentage of CD3+CD16+CD56+ T cells in a representative peripheral blood mononucleated cell sample was 33.7 ± 1.3%. CIK cells, in dose and time dependent manners, inhibited the proliferation of A549. FCM demonstrated that A549 cells were accumulated in G2/M and G0/G1 phases when treated with CIK cells. FCM was used to analyze whether A549 cells treated with CIK cells induced apotosis or necrosis at 10:1 or 20:1. Compared to the control group, P27 was prominently upregulated in the CIK treated group.
Conclusion
We propose that the pharmacological mechanisms of A549 cells inhibited by CIK cells can be estimated to possibly elicit different biological significance, which, in part, can be ascribed to a different mass transport rate in vitro.
Introduction
Human lung cancer is one of the most common malignant diseases and a leading cause of death each year in much of the developed world, particularly in China.1 Adenocarcinoma, the most common form of lung cancer, is one of main human malignant tumors, and its occurrence and development are highly correlated with the inactivation of tumor suppressor genes. Many genes play a role in negatively regulating lung tumor growth and apoptosis.2, 3 Most lung cancer patients are diagnosed at advanced stages (III or IV) and various treatments have emerged including chemotherapy, radiotherapy, target therapy, and immunotherapy.4 Failure of chemotherapies and hormone-deprivation therapies is the major cause of death in patients with castration-resistant lung cancer.
Cytokine-induced killer (CIK) cells are major histocompatibility complex unrestricted cytotoxic lymphocytes and are generated by incubation of peripheral blood monocytes (PBMC) in the presence of various types of cytokines, such as CD3 monoclonal antibody, interleukin-2 (IL-2), IL-l, and interferon-gamma (IFN-γ).5 Currently, the immunomodulatory properties of CIKs provide a rationale for their use with immunotherapeutic agents in lung cancer, especially for patients with minimal response to chemotherapy alone. The mechanism of how CIK cells regulate tumor growth remains largely unknown. Thus, we also examined the inhibitory mechanism of CIK cells on tumor growth of lung adenocarcinoma A549 cells.
To confirm the inhibitory tumor growth effects of CIK cells on lung adenocarcinoma, we cultured CIK cells and treated human lung adenocarcinoma A549 cells to investigate the effects of CIK cells on A549 cell proliferation. Here we show for the first time that lung tumor A549 cells are more sensitive to CIK-mediated lysis through immunogenic modulation, and that these immunomodulatory activities are P27-dependent.
Materials and methods
Generation of cytokine-induced killer (CIK) cells
CIK cells were isolated and cultured according to standard protocol. Peripheral blood (50 mL) was drawn from the patients using heparin as an anticoagulant. Mononuclear cells were isolated by Ficoll-Conray density gradient centrifugation (GE Healthcare, Fairfield, CT, USA), and then the remaining cells were washed twice with phosphate buffered saline (PBS). The viability and concentration of mononuclear cells were determined using trypan blue and a hemacytometer. About 2.0 × 106/mL of mononuclear cells were cultured in six-well culture dishes with medium containing RPMI 1640 plus 1.0 × 106U/L human IFN-γ, 10% heat inactivated human serum, 25 mM HEPES, and 2 mM L-glutamine incubated overnight at 37°C in 5% CO2. After 24 hours, 50 μg/L monoclonal antibody (MAb) against CD3 and rhIL-2 (1 × 106 U/L) was added. Fresh complete medium with rhIL-2 (1 × 106 U/L) was added every two to three days, and the cells were harvested on day 14. All CIK cell cultures were tested for contamination (bacteria, fungi, and mycoplasma) throughout the study to assure culture quality and transfusion safety.
A549 cell culture
The lung epithelial carcinoma cell line A549 was obtained from the Cellular Biology Institute of the Chinese Academy of Sciences. The frozen cells were defrosted, transferred, and maintained in medium RPMI-1640 (Gibco BRL, Life Technologies Inc, Gaithersburg, MD, USA) supplemented with 10% heat-inactivated fetal calf serum (Sijiqing Biological Engineering Co., Hangzhou, China), 100 U/mL penicillin, and 100 μg/mL streptomycin (North China Pharmaceutical Co. Shijiazhuang City, China). Cells were grown in a humidified atmosphere (37°C, 5% CO2).
The viability and concentration of mononuclear cells were determined using trypan blue and a hemacytometer.
MTS cytotoxicity assays
Viability of the lung epithelial carcinoma cell line treated with three ratio combinations was assessed using CellTiter 96® Aqueous Non-Radioactive Cell Proliferation Assay (Promega Corporation, Madison, WI, USA) as previously described. Briefly, A549 cells were seeded in 96-well microtiter plates (Nunc) at 1.0 × 104 per well at 37°C in a 5% CO2 humidified atmosphere. After a 24-hour incubation, the medium was removed and the cells were treated with CIK cells for 72 hours. Effector-to-target cell ratios (E/T ratio) ranged from 10:1, 20:1, or 30:1. In the control group there was only A549 cells. After a 24 hour incubation, the medium was carefully removed and replaced with fresh medium; 20 μL [3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxy-phenyl)-2-(4-sulfophenyl)-2H-tetrazolium, inner salt] (MTS) agent (Promega Corporation) was added to each well and incubated at 37°C for two hours. The cytotoxicity of the A549 cells was measured at 570 nm. All assays were performed in triplicates and repeated in three independent experiments.
Flow cytometry assays
After stimulation, the lymphocytes were surface stained with antibodies as indicated, as well as with a fixable dead cell stain (Live/Dead; Invitrogen, NY, USA). In some experiments, GolgiPlug (BD Biosciences, NY, USA) was added after the first hour of stimulation. Thereafter, cells were fixed, permeabilized, and stained internally with anti-CD3, anti-CD16, and anti-CD56. All flow cytometry (FCM) data were acquired on an LSR Fortessa instrument (BD Biosciences, USA) and the resulting data were analyzed with FlowJo Version 9.4 software (TreeStar Inc., Ashland, OR, USA). The phenotypes of cultured cells were determined by flow cytometry (BD FACSCalibur, NY, USA). The cells were labeled with monoclonal antibodies (BD Biosciences) that recognize human CD3, CD16, and CD56.
The cells in the control and treated groups were harvested and stained by trypsinization with phycoerythrin-labeled annexin V and 7-AAD (BD Biosciences), and fluorescence was measured using FCM. Ten thousand cells were counted.
Analysis of P27 protein by Western blot
A549 cells with or without CIK cells were harvested with lysis buffer, total proteins were extracted, and the protein concentration in the lysate was determined using a spectrophotometer. Lysate containing 70 μg of protein was loaded on to 12% acrylamide gels, subjected to sodium dodecyl sulfate-polyacrylamide gel electrophoresis (Bio-Rad, Hercules, CA, USA), and subsequently transferred onto a polyvinylidene difluoride membrane by electroblotting. Immune complexes were visualized with specific antibodies against ING4 (dilution; 1:500) and p27 and glyceraldehyde 3-phosphate dehydrogenase (dilution; 1:200) (Santa Cruz Biotechnology, Santa Cruz, CA, USA). We also used non-immune goat serum antibody (Santa Cruz Biotechnology) as the negative control. The secondary antibodies used were mouse anti-rabbit immunoglobin G. The sections were reacted with 3,3-diamino-benzidine tetrahydrochrolide (Santa Cruz Biotechnology) in the presence of 3% H2O2 to develop colour. The sections were counter-stained with haematoxylin and mounted with glycerol. Mononuclear cells staining positively in gingival sections were counted in each of three, randomly selected microscopic fields (at ×200 magnification) from five slides from a gingival cell sample.
Statistical analysis
Statistical analysis of the data was performed using the SPSS package (v.12.0.1, SSPS Inc., Chicago, IL, USA). The chi-square (Fisher's exact test) and Student's t tests were used to evaluate the differences in categorical variables and continuous variables, respectively. Results were expressed as mean ± standard deviation. Analysis of variance (ANOVA) and the Fisher protected least significant difference were test using for analysis. Results were compared with one-way analysis of variance (ANOVA) and Fisher protected least significant difference. P values of <0.05 were considered significant.
Results
Characterization of CIK cells
To study the cellular immune responses generated during PBMC, cells were cultured with low concentrations of IFN-γ, IL-2, and αCD3 mAb. Cells were harvested on days +14, then counted to be used to assess informative phenotypic features. Interestingly, the percentage of CD3+CD16+CD56+ T cell expression in a representative PBMC sample was 33.7 ± 1.3%, as shown in Figure 1.
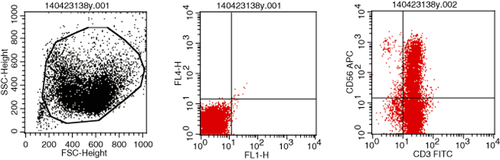
Expansion of cytokine-induced killer (CIK) cells in cultures supplemented with cytokines. The absolute number of CIK cells (CD3+CD16+CD56+) were analyzed by flow cytometry after the provision of interferon-gamma, interleukin-2 and αCD3 mAb to the cultures. Numbers in outlined areas indicate percentage of cells. Results of one representative experiment showing the percentages of CD3+CD16+CD56+ cells. Data are representative of six separate experiments each involving groups of two cultures.
Cell cytotoxicity of CIK cells on A549 cells
The cytotoxicity of the CIK cells was assessed by cell viability against the A549 cells lines by MTS assay. With the different ratio of effector and target cells, the cytotoxic activity was determined. Generally, the cytotoxicity of the treated group at the different ratios of E/T was higher than that of the control group, indicating the inhibition effect of CIK on the A549 cells. A549 cells had similar patterns in response to the cytotoxicity of CIK cells. Meanwhile, the cytotoxicity of the treated groups significantly changed compared with that of different ratios of E/T treatment for 24, 48, and 72 hours, indicating that the CIK activity is likely to have a time and dose dependent manner of inhibitory effect on A549 cells (Fig 2).
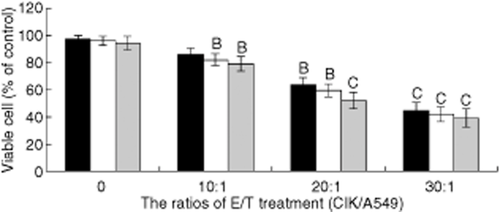
Effects of cytokine-induced killer (CIK) cells on cell cytotoxicity in A549 cells determined by MTS assay. Results are expressed as % of control (n = 6. Mean ± standard deviation. BP < 0.05, CP < 0.01 vs. the control group). Analysis of variance with subsequent multiple comparisons test. ■, 24 hours; □, 48 hours;  , 72 hours.
, 72 hours.
Cell cycle analysis
The cells were cultured in a six-well plate for 24 hours and then incubated with different ratios of CIK (10:1, 20:1, or 30:1) for 72 hours. The cells were then digested, resuspended, incubated with P-gp antibodies for 30 minutes at 4°C, and washed twice in PBS. As shown in Table 1, CIK cells caused a significant dose-dependent accumulation of A549 cells in the G2/M phases, lightly in the G0/G1, and a decrease of S phases from 1:10 to 1:30 at 48 hours (Fig 3.) The differences in cell cycle distribution between the A549 and CIK treated A549 cells were statistically significant (P < 0.01). This indicated that CIK cells influenced the distribution of A549 cells in each phase of the cell cycle, especially at higher concentrations (Table 1).
| Group (μg/mL) | Cell cycle distribution (%) | ||
|---|---|---|---|
| G0/G1 | S | G2/M | |
| Control | 44.9 ± 1.3 | 35.1 ± 2.5 | 12.4 ± 2.0 |
| Treated | |||
| 10:1 | 51.7 ± 3.3 B | 19.7 ± 4.6 C | 29.9 ± 3.7 C |
| 20:1 | 56.1 ± 5.6 B | 10.1 ± 2.7 C | 32.1 ± 4.2 C |
| 30:1 | 59.1 ± 5.2 B | 2.9 ± 1.8 C | 38.4 ± 5.0 C |
- Because of infrequent cytokine-induced killer (CIK) cells treated, S and G2/M are combined as G0/G1 changed in A549 cells. Control and treated group (n = 6). A549 cell populations discriminated by CIK cells. Results expressed as mean (%) positive (range). Results are expressed as % of control. BP < 0.05, CP < 0.01 versus control.
The effect of cell cycle progress in A549 by cytokine-induced killer cells.
Cell cycle distribution was detected after treating cells with an E/T ratio ranging from 10:1, 20:1 or 30:1 cells. Cell cycle analysis by FCM showed that the proportion of cells in the G0/G1 and G2/M phase were significantly higher after CIK cell treatment (one-way ANOVA).
As demonstrated in Figure 3, different lineage sets have different phase fraction profiles, suggesting that they cycle at different rates, following the order of 10:1 > 20:1 > 30:1 from most rapid to slowest proliferation. Mean results and ranges for cell cycle distribution in the control set are summarized in Table 1.
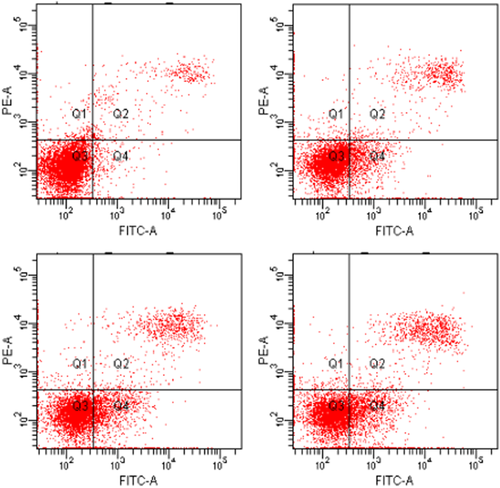
CIK-induced apoptosis of A549 cells
DNA fragmentation during apoptosis can occur in CIK treated cells. We analyzed the characterization of apoptosis detected by dual staining with Annexin V-FITC and PI. Assessment of the apoptosis rate of the treated groups at the different ratios of E/T was higher than that of the control group. This illustrated that the increased apoptosis observed in the treated group could be induced by CIK. Similar cell cycle analyses for Annexin V are illustrated in the representative control and CIK treated samples. Increased cell cytotoxicity occurred with increased concentrations of CIK cells (E/T ratio is 10:1, 20:1 or 30:1). Fluorescein-labelled annexin V and PI-stained cells analyzed the effect of CIK cells on A549 cells. The ratio of apoptosis and necrosis of the cells were increased (Table 2).
| Group (μg/mL) | Apoptosis rate (%) | Necrosis rate (%) |
|---|---|---|
| Control | 0.2 ± 0.1 | 0.1 ± 0.0 |
| Treated | ||
| 10:1 | 6.8 ± 1.0B | 1.3 ± 0.2B |
| 20:1 | 18.8 ± 3.9C | 7.1 ± 0.8B |
| 40:1 | 22.6 ± 4.1C | 10.9 ± 1.3C |
- Because of infrequent cytokine-induced killer (CIK) cells treated, the apoptosis rate is different in A549 cells. Control and treated group (n = 6). A549 cell populations discriminated by CIK cells. Results expressed as mean (%) positive (range). Results are expressed as % of control. BP < 0.05, CP < 0.01 versus control.
These results suggest that at least a major proportion of CIK cells co-cultured with A549 is related to apoptosis, either a result of DNA fragmentation during apoptosis or associated with initiation of apoptosis.
Effects of CIK cells on the activity of P27 protein
Subsequently, we explored the mechanisms involved in the effects of A549 cells on the above proteins by examining the effects of expression on the level of Wnt-1 cell signal transduction by Western blot analysis. A549 cells treated with CIK cells for 72 hours were analyzed for P27 protein activity by Western blot. Compared to the control group, P27 was prominently upregulated in the CIK treated group. The activity of P27 expression after CIK cell treatment in A549 cells became fourfold higher than in the control cells (Fig 4).
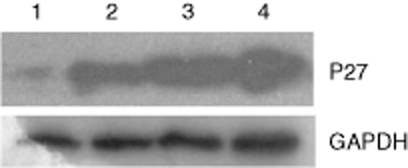
The expression of P27 was upregulated in response to cytokine-induced killer cells by Western blot analysis of A549 cells. Analysis of variance with subsequent multiple comparisons test. Control group: lane 1: treated group; lane 2: 10:1 effector-to-target cell (E/T) ratio; lane 3: 20:1 E/T ratio; lane 4: 30:1 E/T ratio. GAPDH, glyceraldehyde 3-phosphate dehydrogenase.
Discussion
Cytokine-induced killer cells derived from cord blood are a new type of antitumor immune effector cell in tumor prevention and treatment and have increasingly attracted the attention of researchers. Adoptive cell immunotherapy, as a potential new approach, holds great promise for the treatment of tumors resistant to conventional therapies.6, 7 Schmidt-Wolf et al. first reported that CIK cells, which are now considered as the primary candidate for adoptive cell immunotherapy, have a strong anti-proliferative capacity and cytotoxicity against tumor cells.8 It is believed that CIK cells are heterogeneous in in vitro-expanded T lymphocytes with mixed NK like T cells. The anti-tumor activity of CIK cells is a result of the high proliferative and cytolytic potential of CD3+CD56+ NKT cells, which increases about 100 to 1000-fold and is mediated by the interaction of the NKG2D receptor with MHC-unrestricted ligands on tumor cells.9, 10
In normal cells, multiple intrinsic and extrinsic signaling pathways tightly regulate proliferation. Cells become cancerous when they acquire genetic alterations that allow them to evade such regulatory mechanisms. We performed a detailed phenotypic analysis using a panel of markers in order to characterize the CD3+CD16+CD56+ cell subsets. Using FCM assay, we found that, in comparison with cell control, cell apoptosis increased markedly in treated cells, while the cell cycles of G2/M and G0/G1 phases significantly accumulated. Western blot analysis was used to determine the expression of cell proliferation-regulating protein, P27 activation, of the Wnt-1 pathway in A549.
Our results were very interesting. In order to elucidate the pathway leading to the change of cell cycle and apoptosis, we examined the activation of P27, which had been reported to initiate apoptosis upon various stimuli.11, 12 Alternatively, CIK cells exhibited a high proliferation rate while the cytotoxic activity was different between the control and treated groups. Western blot showed that the expression of apoptosis associated gene P27 was upregulated. These results suggested that the anti-tumor effect of CIK cells on A549 cells was related to the induction of apoptosis after changing the cell cycle. The results further suggested that the anti-tumor effect of CIK cells on A549 cells was related to the induction of apoptosis and necrosis.
Adoptive cellular immunotherapy of patients with hematologic malignancies after umbilical cord blood transplant is crucial. CIK cells are heterogeneous cell populations derived from human peripheral blood or mice spleen after in vitro expansion with IFN-γ, IL-2, and anti-CD3 antibodies.13 CIK cells mediate potent MHC-unrestricted cytotoxicity against a variety of tumor cells and can recognize and kill tumor cells without prior exposure or priming. Two main subpopulations can be distinguished within the bulk culture of in vitro expanded CIK cells, one co-expressing the CD3 and CD56 molecules (CD3+CD56+) and the other presenting a CD3+CD56− phenotype. The antitumor activity of CIK cells has been reported to be mainly restricted to CD3+CD56+ cells.14 Functional analysis had revealed that CIK cells play a critical role in inducing A549 cells to apoptosis and necrosis by FCM analyses, which showed that A549 cells were gradually eliminated during the process of CIK cell treated. Adoptive CIK cell transfer, as an adoptive immunotherapy demonstrates a promising nontoxic anticancer therapy in the treatment of solid tumors refractory to conventional therapies. However in clinical studies, the therapeutic activity of CIK cell transfer is not as efficient as anticipated.15 Effective adoptive cell transfer is facing numerous challenges, such as systemic immune tolerance and tumor local immune escape. The homing of immune cells to the tumor site is reduced and antitumor immune functions are inhibited by tumor microenvironment and immunomodulatory properties of suppressive cell populations.16, 17
The reason eliciting different biological outcomes by different microenvironments is still unclear. We carried out this study with an aim to understand more about the cellular physiology and, conversely, the different cytotoxicity of CIK cells that may occur in different microenvironments as specified by the co-culturing of A549 cells. Apoptosis, necrosis, and lysis of tumor cells are possible mechanisms by which CIK cells inhibited tumor growth.
Conclusion
In conclusion, the present study indicates that CIK cells, as tumor suppressors, negatively regulated A549 cell proliferation and tumor growth by upregulation of cell proliferation-regulating proteins, such as P27, by means of inactivation of Wnt-1 signaling. CIK cells could also enhance the apoptosis rate in A549 cells, suggesting that CIK cells may be a candidate for cell therapy and a new approach for treating patients with lung adenocarcinoma.
Acknowledgment
We are indebted to Bao-en Shan from the Research Centre, the Fourth Hospital of Hebei Medical University (Shijiazhuang, China) for equipment and technical assistance. We thank Paula E. Cushing for assistance with the manuscript. This research was supported by grants from the Key Medical Research Plan of the Hebei Province of China (No. ZD2013063) and the National Natural Scientific Foundation of China (No. 31101638).
Disclosure
No authors report any conflict of interest.