Association between sacroiliac joint forms and subchondral changes in patients with Crohn's disease
Oksana Melekh, Felix Barajas Ordonez, and Bohdan Melekh contributed equally to the manuscript.
Abstract
Aim
To assess the relationship between anatomical variants of sacroiliac joint (SIJ) and subchondral changes detected in magnetic resonance enterography (MRE) in patients with Crohn's disease (CD).
Methods
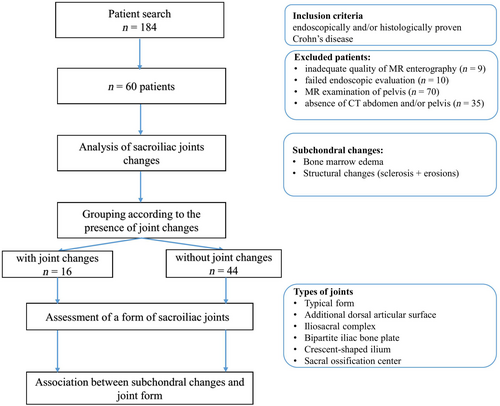
This was a retrospective study of 60 CD patients, who were divided into two groups: with (n = 16) and without SIJ (n = 44) involvement, depending on the presence of inflammatory (bone marrow edema) and structural changes (sclerosis and erosions) in MRE. Anatomical variants of SIJ were assessed in CT of the abdomen and/or pelvis, distinguishing typical form with convex iliac surface and atypical forms. Univariate and multivariate analyses were performed to reveal an association between joint changes and forms.
Results
Our study included 60 patients (38 males; mean age 38.72 years ± 13.33). Patients with SIJ changes were older (p = .044). No significant differences in CD localization and behavior were found. The most common SIJ lesions were structural changes (in 75% of patients); the main atypical form was the iliosacral complex. The univariate and multivariate analyses showed a significant association of atypical forms with total subchondral changes (odds ratio [OR]: 3.429, 95% confidence interval [CI] 1.043–11.268; p = .042; OR: 5.066, 95% CI: 1.273–20.167; p = .021, respectively), and with structural changes (OR: 4.185, 95% CI: 1.155–15.160; p = .029; OR: 5.986, 95% CI: 1.293–27.700; p = .022, respectively).
Conclusion
Atypical forms of SIJ are a risk factor for the occurrence of structural joint changes in CD patients. An association between bone marrow edema and atypical forms was not found.
Plain language summary
- Magnetic resonance enterography reveals inflammatory and structural subchondral changes of the sacroiliac joints in patients with Crohn's disease.
- The typical form of sacroiliac joints with a convex iliac surface is distinguished from atypical forms.
- Atypical forms are a risk factor for the occurrence of structural joint changes in patients with Crohn's disease.
1 INTRODUCTION
Sacroiliitis is the most common extraintestinal manifestation of Crohn's disease (CD), with an incidence of 12%–46%, and remains one of the main reasons for worsening quality of life and reducing working capacity.1-5 The diagnosis of sacroiliitis is based on evaluating clinical, laboratory, and radiological methods. According to the Assessment of SpondyloArthritis International Society (ASAS), MRI plays a crucial role in assessing sacroiliac joint (SIJ) changes, especially in the early stage, when only bone marrow edema (BME) or synovitis develop.6-8
Magnetic resonance enterography (MRE) is another MRI tool that can be used to evaluate SIJ changes. As a non-ionizing imaging modality, MRE is becoming an essential pillar for the diagnosis and assessment of disease activity and complications such as stricture, fistula and abscess, as well as monitoring and guiding decision-making in inflammatory bowel disease (IBD).9-12 The interest in this method is constantly growing due to the ability to cover a more significant spectrum of patients and an opportunity to simultaneously investigate intestinal and sacroiliac changes, the relationship of which still needs to be studied. Some previous studies have already reported the ability of MRE to detect BME and structural changes as incidental findings in patients with IBD, with a prevalence of 15%–23.5%.13, 14 In a recent systematic review by Evans et al.15 in 2021, who investigated the prevalence of sacroiliitis in patients with IBD, the clinical relationship between sacroiliitis and CD intestinal forms remains unclear, as no association was found between sacroiliitis, age, number of exacerbations, CD duration, bowel involvement, and behavior.
The influence of mechanical stress on the appearance of subchondral joint changes has been increasingly discussed.16-21 Several experimental and clinical studies also showed the role of mechanical stress even in developing inflammatory joint diseases.19-21 For instance, Thorarensen et al. and Zeng et al. demonstrated that physical trauma or prolonged repetitive work, which led to mechanical stress, should be considered a risk factor for inflammatory joint disease in psoriatic (OR: 1.32, 95% CI: 1.13–1.54) and rheumatoid (OR: 1.8, 95% CI: 1.6–2.0) arthritis.19, 20
Vleeming et al.,22 studying functional anatomy and biomechanics of the pelvic girdle, showed that mechanical loading is crucial in developing SIJ changes due to the constant affection by the biophysical redistribution of forces between the trunk and lower limbs.
Prassopoulos revealed the variability of anatomical forms of SIJ, where a typical shape with a convex iliac surface was distinguished from atypical shapes (concave iliac surface, accessory joint facet, iliosacral bridge, and bipartite iliac bone plate).23 Using this model, Ziegeler et al.24 reported a higher prevalence of atypical forms and symptomatic patients with mechanical and inflammatory SIJ disease compared to control patients (80.3% vs. 44.1% vs. 37.5%, respectively; p < .001). The association of SIJ anatomical variability with inflammatory and structural SIJ changes in CD patients has not been previously analyzed. Thus, this study aimed to assess the relationship between anatomical variants of SIJ evaluated in CT and subchondral changes detected in MRE.
2 MATERIALS AND METHODS
2.1 Patient selection
This was a retrospective study of CD patients who underwent MRE in the University Clinic for Radiology and Nuclear Medicine (University Hospital Magdeburg) between June 2010 and April 2020. The search of CD patients was performed using the picture archiving and communication system (PACS INFINITT Healthcare, Seoul, South Korea). MRE scans were used to assess disease extension, discard complications, or evaluate therapy response. CT scans of the abdomen and/or pelvis were mostly performed as a part of diagnostic in case of abdominal pain or suspected fracture. The inclusion criteria were: (a) endoscopically and/or histologically proven CD; (b) complete demographic data in the clinical records; (c) first MRE chronologically available; (d) previously performed CT of the abdomen and/or pelvis with a slice thickness of ≤2 mm. The exclusion criteria were (a) MRE or CT without or with partial SIJ in the field of view (FOV), (b) incomplete clinical data, (c) strong MRE artifacts, and (d) MRI only of the pelvic region (for instance, to assess a perianal complication). Clinical data comprised sex, weight, height, age, duration of disease, and the number of exacerbations. This information was extracted from our internal database (MEDICO KIS, CompuGroup Medical SE & Co. KGaA, Koblenz, Germany). The study design is summarized in Figure 1.
Patients were classified according to the Montreal classification, considering age of onset (A1) ≤17 years, (A2) 17–40 years, (A3) >40 years; disease behavior (B1) non-stricturing, non-penetrating, (B2) stricturing, (B3) penetrating; and location (L1) terminal ilial, (L2) colonic, (L3) ileocolonic, and (L4) upper gastrointestinal tract.25
The body mass index (BMI) was calculated by dividing body weight in kilograms by height in meters squared. Patients were classified according to BMI as follows: underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (between 25 and 29.9 kg/m2), and obese (≥30 kg/m2).26
2.2 CT and MRE technique
Our MRE technique has been previously described, the MRI sequences are depicted in the Table S1.27, 28 All CT examinations were performed on a multidetector CT scanner (Siemens Somatom Definition AS+, Siemens Healthineers, Germany; Canon Aquilion Prime, Canon Medical Systems Corporation, Japan). The CT protocol was as follows: acquisition slice thickness of ≤2 mm; tube voltage, 120 kV; automatic tube current modulation; pitch factor, 1.2.
2.3 Image analysis
Two radiologists with 15 and 9 years of experience blinded to the patient's clinical data independently evaluated all examinations. In case of discrepancies in data analysis, a consensus was reached by repeated joint analysis of images with discussion between two radiologists.
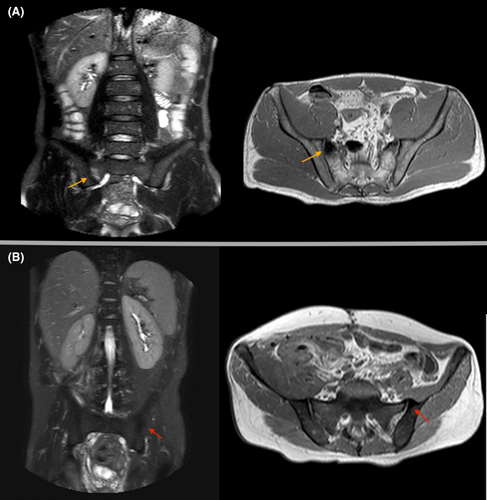
2.4 Assessment of sacroiliac joint changes in MRE
Each SIJ was divided into four segments (upper sacral and iliac, lower sacral and iliac). The borders between these segments were one horizontal line drawn through the lower edge of the first upper anterior sacral foramen on both sides and one vertical line drawn through the joint space on both sides (Figure S1). Changes in each segment of both SIJ were evaluated. According to the ASAS guidelines (Assessment of SpondyloArthritis International Society), BME was identified as a hypointense signal on T1-weighted images and a hyperintense signal on both T2-weighted and short tau inversion recovery (STIR) images8, 29 (Figure 2). Structural changes included subchondral sclerosis and erosions. Subchondral sclerosis was recognized as a hypointensity on T1- and T2-weighted sequences. In line with the ASAS recommendations, erosion was determined as a hypointensity on T1-weighted images with defects at the joint margins.8 In some cases, we did not reveal those defects due to the limitations of our MRE protocol. Therefore, we combined subchondral sclerosis and erosions into one group, “subchondral changes,” based on their hypointensity in T1-weighted images (Figure 2). Each change was scored using a binary system for every quadrant, based on the presence (score = 1) or the absence (score = 0).
2.5 Assessment of sacroiliac joint form in CT
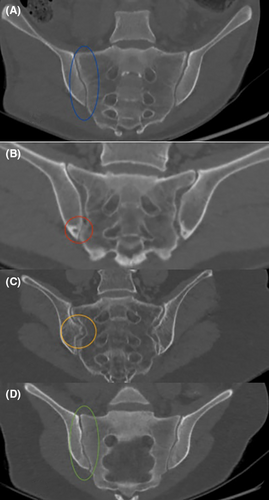
SIJ form was evaluated in a reformatted oblique coronal plane, parallel to the sacrum, using the model defined by Prassopoulos et al.23 This model distinguishes between a typical joint form with a convex iliac joint surface and atypical forms (Figure 3). The letters include: (a) joints with an additional dorsal articular surface; (b) the iliosacral complex, which is characterized by a large convex notch on the side of the ilium and a corresponding concave impression in the sacrum; (c) a bipartite iliac bone plate with unfused two articular plates of the iliac bone in the form of inverted lobster claws; (d) concave articular surface of the ilium in the form of a sickle; (e) semicircular defects on both the ilium and the sacrum; and (f) also with the centers of ossification of the sacrum in the form of an additional bone on the front upper side of the joint. Each type of joint form was also scored using a binary based on the presence (score = 1) or the absence (score = 0).
2.6 Statistical analysis
The normality of the data distribution was assessed using the Kolmogorov–Smirnov test. Continuous variables were expressed as mean (M) and standard deviation (SD) or median and interquartile range (IQR). Continuous variables were compared between groups using the Student's test or Mann–Whitney test, as appropriate. Categorical variables were compared by performing the chi-squared test or Fischer's exact test. The univariate and multivariate (adjusted for age, sex, and BMI) analyses were performed to evaluate the association between forms and subchondral changes of SIJ using a logistic regression model. The intra- and interobserver agreement was assessed using Cohen's kappa test for our categorical variables, including subchondral SIJ changes (structural changes and BME) and types of anatomical SIJ variants. The kappa coefficient is interpreted as follows: .01–.20, slight agreement; .21–.40, fair agreement; .41–.60, moderate agreement; .61–.80, substantial agreement; and >.80, almost perfect.30 A p-value of .05 was considered to be statistically significant. The statistical analysis was performed with a statistical software package (SPSS Statistics for Windows, version 27.0; IBM Corp., Armonk, NY, USA).
3 RESULTS
Our study included 60 patients (38 males and 22 females; mean age: 38.72 years ± 13.33). Patients were divided into two groups: with (n = 16) and without (n = 44) SIJ involvement. The mean age of patients with SIJ involvement was significantly higher than those without (44.43 years ± 13.12 and 36.64 years ± 12.94, respectively, p = .044). The median disease duration in the group with SIJ involvement was 4.5 years (IQR, 2.25–11.5 years) and 8 years (IQR, 2–15 years) without SIJ changes. This difference was not statistically significant (p = .322). The number of patients with CD onset at 40 years and older was significantly higher in the group with joint involvement than those without (37.5% and 13.6%, respectively, p = .042). We found no significant difference in CD localization and behavior comparing both groups. The median BMI in the group with SIJ involvement was 22.1 kg/m2 [IQR, 19.225–24.6275 kg/m2], and without SIJ involvement, it was 21.37 kg/m2 [IQR, 18.9625–24.63, kg/m2], p = .841. See Table 1.
| With SIJ changes (n = 16), n (%) | Without SIJ changes (n = 44), n (%) | p-Value | |
|---|---|---|---|
| Male | 11 (68.8) | 27 (61.4) | .602 |
| Age (years) M, SD | 44.43 ± 13.12 | 36.64 ± 12.94 | .044 |
| Disease duration (years), median [IQR] | 4.5 [2.25–11.5] | 8 [2–15] | .322 |
| Montreal classification | |||
| Age at diagnosis | |||
| A1 | 1 (6.3) | 13 (29.6) | .062 |
| A2 | 9 (56.2) | 25 (56.8) | .967 |
| A3 | 6 (37.5) | 6 (13.6) | .042 |
| Location of bowel involvement | |||
| L1 | 8 (50.0) | 21 (47.7) | .876 |
| L2 | 5 (31.2) | 15 (34.0) | .840 |
| L3 | 3 (18.8) | 8 (18.3) | .965 |
| L4 | 0 | 0 | 0 |
| Behavior | |||
| B1 | 8 (50.0) | 19 (43.2) | .643 |
| B2 | 7 (43.8) | 20 (45.5) | .908 |
| B3 | 1 (6.2) | 5 (11.3) | .563 |
| Body mass index (BMI) kg/m2, median [IQR] | 22.1 [19.225–24.6275] | 21.375 [18.9625–24.63] | .841 |
| BMI < 18.5 kg/m2 | 2 (12.5) | 10 (22.7) | .386 |
| BMI 18.5–24.9 kg/m2 | 11 (68.8) | 25 (56.8) | .405 |
| BMI 25–29.9 kg/m2 | 2 (12.5) | 6 (13.7) | .905 |
| BMI > 30 kg/m2 | 1 (6.2) | 3 (6.8) | .934 |
- Note: Continuous variables are presented as mean (M) and standard deviation (SD) median and interquartile range (IQR). A1: <17 years; A2: 17–40 years; A3: >40 years; B1: non-stricturing and non-penetrating; B2: stricturing; B3: penetrating; L1: terminal ileal; L2: colon; L3: ileocolonic; L4: upper gastrointestinal tract.
- Abbreviation: SIJ, sacroiliac joint.
3.1 Assessment of subchondral SIJ changes, detected in MRE
SIJ changes were found in 16/60 patients (26.7%), with a total of 32 lesions regarding segmental distribution. BME was recognized in 7/16 patients (43.8%) with 14/32 lesions (43.8%). Structural changes were detected in 12/16 patients (75%), with 18/32 lesions (56.3%).
3.2 Assessment of SIJ form in CT examinations
The prevalence of typical and atypical forms in CD patients with and without SIJ changes is summarized in Table 2. The typical SIJ form was observed in 50% of patients with joint changes and 70.5% without joint changes (p = .144). The main pattern of atypical SIJ forms was additional dorsal articular surface (18.8%) and iliosacral complex (18.8%) in patients with SIJ involvement, whereas in the group without SIJ involvement, it was only iliosacral complex (25.0%). A crescent-shaped ilium was observed only in two patients with joint changes (12.5%). In both groups, we did not detect such forms as the sacral ossification center and the bipartite iliac bone plate.
| SIJ form | With SIJ changes (n = 16), n (%) | Without SIJ changes (n = 44), n (%) | p-Value |
|---|---|---|---|
| Typical form | 8 (50.0) | 31 (70.5) | .144 |
| Atypical form in total | 8 (50.0) | 13 (29.5) | .144 |
| Additional dorsal articular surface | 3 (18.8) | 2 (4.5) | .079 |
| Iliosacral complex | 3 (18.8) | 11 (25.0) | .619 |
| Bipartite iliac bone plate | 0 | 0 | |
| Crescent-shaped ilium | 2 (12.5) | 0 | .003 |
| Sacral ossification center | 0 | 0 |
- Note: SIJ changes included subchondral sclerosis, erosions, and bone marrow edema.
- Abbreviation: SIJ, sacroiliac joints.
3.3 Assessment of association between SIJ changes and SIJ forms
The univariate analysis showed a significant association between atypical SIJ form and total subchondral changes (OR: 3.429, 95% CI: 1.043–11.268; p = .042). This association was also confirmed in multivariate analysis (OR: 5.066, 95% CI: 1.273–20.167; p = .021). The evaluation of the relationship between atypical SIJ changes with inflammatory and structural changes, atypical forms were significantly associated with structural changes (sclerosis and/or erosions) in univariate and multivariate analyses (OR: 4.185, 95% CI: 1.155–15.160; p = .029, OR: 5.986, 95% CI: 1.293–27.700; p = .022, respectively). There was no association in univariate and multivariate analyses between atypical forms and inflammatory changes (OR: 1.133, 95% CI: 0.243–5.293; p = .874, OR: 4.730, 95% CI: 0.337–13.445; p = .429, respectively) (see Table 3).
| Body composition groups | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Total SIJ changes | ||||||
| Atypical form (absent vs. present) | 3.429 | 1.043–11.268 | .042 | 5.066 | 1.273–20.167 | .021 |
| Structural SIJ changes | ||||||
| Atypical form (absent vs. present) | 4.185 | 1.155–15.160 | .029 | 5.986 | 1.293–27.700 | .022 |
| Bone marrow edema | ||||||
| Atypical form (absent vs. present) | 1.133 | 0.243–5.293 | .874 | 4.730 | 0.337–13.445 | .429 |
- Note: Multivariate analysis (adjusted for age, sex, and body mass index).
- Abbreviation: SIJ, sacroiliac joint.
3.4 Intra- and interobserver agreement
The intra-observer and interobserver assessment of subchondral SIJ changes resulted in an almost perfect agreement with kappa values of more than .804 (p < .001). The analysis of anatomical SIJ variants was also almost perfect as well (kappa more than .880, p < .001) except for crescent-shaped ilium, which demonstrated a kappa value of .792 (p < .001). The latter outcome was caused by a low number of this SIJ form (the first reviewer found it only in two patients and the second one in three patients). All results are summarized in Table S2.
4 DISCUSSION
Our study retrospectively assessed the association of anatomical variation of the SIJ and the occurrence of inflammatory (bone marrow edema) and structural changes (sclerosis and erosions) in CD patients. Our findings suggest that the occurrence of subchondral changes is significantly more common in patients with atypical forms of SIJ, especially in the case of structural changes. An association between inflammatory changes and atypical SIJ forms was not found.
In our study, SIJ involvement, including inflammatory and structural SIJ changes, was identified in 23% of the patients and was consistent with previous research, which found sacroiliitis in 2%–45% of patients with inflammatory bowel disease using CT and MRI of SIJ.31-33 Also, we did not observe any difference in the incidence of SIJ changes compared to studies based on MRE; for instance, in a recent study by Cereser et al.,13 who in 2022 retrospectively assessed inflammatory and structural SIJ changes in 100 adult and 30 pediatric patients with CD, found it in 20% of adults and 6.7% of pediatric patients. The further studies showed a feasibility of MRE to detect BME, sclerosis, fatty deposits, and also to some extent erosions with ankylosis.6, 13, 14, 34 However, studies in patients with inflammatory bowel disease, especially with CD, based either on MRE or on MRI, found no significant association between SIJ changes and clinical parameters such as disease duration, behavior, bowel involvement, and BMI.6, 13, 14, 34-37 We also did not find any significant difference in the abovementioned clinical parameters between CD patients with and without SIJ changes. An essential advantage of our study was the analysis of changes in MRE, which allows us to reveal even clinically asymptomatic joint lesions, which can also appear due to the influence of potential mechanical stress. The influence of mechanical loading was demonstrated by Varkas et al.,17 they found asymptomatic BME in 50% of military recruits, who underwent an MRI of SIJ before and after 6 weeks of intense physical training. Asymptomatic BME was also revealed by Weber et al.38 in 30%–35% of runners and 41% of ice-hockey players.
We observed atypical forms of SIJ in 21/60 CD patients (35%), which was lower than the prevalence found by Ziegler et al.24 (44.1% and 80.3% in the case of axial spondyloarthritis and mechanical joint disease, respectively). This discrepancy could be explained with another inclusion criteria and CT protocol of our study. First, Ziegler et al. included patients with low back pain (>6 months) and suspicion of axial spondyloarthritis. The cohort of our patients consisted only of those who underwent MRE to reveal an intestinal form of CD; therefore, clinical manifestations of joint involvement were not considered.24 Second, the protocol of CT abdomen or pelvis, which was performed in our patients, was characterized by decreased resolution of reformatted CT due to thicker slices and a larger FOV compared to the protocol of CT examination of SIJ, which was used in the study by Ziegler et al.24 However, the main form of atypical joint variants, which was the iliosacral complex in patients of both groups, was in agreement with the results of the same studies by Ziegler et al.18, 24 Therefore, based on the obtained results, CT of the abdomen or pelvis allowed us to assess the SIJ form adequately.
In the comparative analysis of groups with and without SIJ changes, we found that atypical SIJ forms were significantly associated with total joint changes (OR: 3.429, 95% CI: 1.043–11.268; p = .042). The multivariate analysis was also performed to exclude the influence of sex, BMI, and age, which are related to the anatomical variants and subchondral changes of the pelvis. The association was confirmed (OR: 5.066, 95% CI: 1.273–20.167; p = .021). Based on the relationship between atypical SIJ forms and their joint changes in case of mechanical joint disease and axial spondyloarthritis (both p < .001), Ziegeler et al.24 assumed that this association might be caused by mechanical stress. This hypothesis should also be considered in our study, where we obtained similar results. Currently, mechanical stress is also considered a trigger factor for chronic inflammatory arthropathies, which, in addition to biomechanical influence, can provoke an immune response.16, 18 In an analysis of the influence of atypical forms on the appearance of inflammatory or structural changes, we found an association only with structural changes (sclerosis and/or erosions) in univariate and multivariate analyses (OR: 4.185, 95% CI: 1.155–15.160; p = .029 and OR: 5.986, 95% CI: 1.293–27.700; p = .022; respectively). The discrepancy in the results between inflammatory and structural changes, namely the lack of association of atypical forms with BME, may indicate that only in the late stages, mechanical stress increases the development of joint changes, in contrast to the early ones, where its role is probably significantly limited. In our opinion, this hypothesis needs further study based on prospective studies with a large number of probands.
This study has several limitations, including the monocentric setting and the retrospective design. The assessment of SIJ changes in MRE was limited compared to the evaluation of joint changes revealed in a dedicated MRI sacroiliac joint protocol due to a lack of inclined projections and a large FOV with lower spatial resolution. In addition, difficulties in interpreting the location of subchondral lesions of SIJ are associated with the complex anatomy of this joint. This joint consists of a C-shaped cartilaginous part, which is located caudally and ventrally, and a ligamentous part, which in turn is cranially and dorsally.39 Thus, the assessment of the localization of joint changes only in the usual coronal and axial planes is limited. Furthermore, the differentiation between erosions and sclerosis was only sometimes possible due to the absence of an appropriate morphological VIBE sequence.40 However, the lack of differentiation of erosions from sclerosis did not reduce the reliability of the obtained data since the structural changes were evaluated in total. There was another limitation in assessing the anatomical variants due to using the CT protocols of the abdomen and/or pelvis with a higher slice thickness (1–2 mm) and a larger FOV, which might limit the validity of our results to some extent. The small sample size was a significant limitation, mainly due to the low number of patients who underwent CT of the abdomen/pelvis and MRE. The lack of clinical data about concomitant diseases, especially axial spondyloarthritis, and the state of physical activities were also considered a limitation of this study.
5 CONCLUSION
Atypical forms of SIJ are a risk factor for structural joint changes detected in MRE in CD patients. An association between bone marrow edema and atypical forms was not found. Our findings indicate the clinical significance of considering mechanical stress as a co-factor for SIJ changes in CD patients, which can change a therapeutic strategy in clinical work. One area of future research should involve the association between mechanical stress on the appearance of subchondral changes in CD patients. A simultaneous application of MRE and MRI can cover a more significant number of patients and evaluate other articular involvements, such as fatty metaplasia, which is one of the critical pathogenetic links in the development of irreversible joint changes. The possible establishment of a relationship between anatomical variants of SIJ and subchondral and bowel changes in CD patients can uncover novel diagnostic and therapeutic opportunities.
AUTHOR CONTRIBUTIONS
Guarantors of the article: OM, FBO, BM, AS. Development of study concept and design: OM, FBO, BM, AS. Study supervision: MP, AS. Acquisition, analysis and interpretation of the data: OM, AS, FBO, BM. Statistical analysis: OM, BM, FBO. Drafting of the manuscript: BM, FBO, OM, AS. Critical revision of the manuscript for important intellectual content: BM, FBO, JO, PM, AS. All authors approved the final version of the manuscript including the authorship.
ACKNOWLEDGMENTS
Open Access funding enabled and organized by Projekt DEAL.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflict of interest.
ETHICAL APPROVAL
This study was approved by the Institutional Review Board Ethics Committee (number: 145/21), Otto-von-Guericke University, Magdeburg, Germany.
Open Research
DATA AVAILABILITY STATEMENT
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.




