Radiological Insights Into the Pericardium: A Comprehensive Review
Funding: The authors received no specific funding for this work.
ABSTRACT
The pericardium is not simply a two-layered membrane surrounding the heart and great vessels. Pericardial effusion is the most common manifestation of various pathological conditions involving the pericardium. Therefore, we are tempted to think of the pericardium as a virtual space containing only fluid, but it can also contain solid and cystic lesions. We must recall that clinical symptoms are non-specific and may mimic cardiac, pulmonary, or pleural diseases. Imaging findings are not specific for a particular pathology, but when combined with the clinical history, can provide sufficient information to make an accurate differential diagnosis. In this review, we will identify selected entities affecting the pericardium, from benign to malignant, with a brief description of their clinical characteristics.
1 Introduction
The pericardium is a two-layered membrane that envelops the heart and great vessels [1]. Pericardial effusion is the most common manifestation of various pathological conditions involving the pericardium. The pericardium can be affected by primary pathologies, systemic diseases, and iatrogenic causes such as cardiac surgery and radiation [2]. It is important to note that iatrogenic causes are a significant contributor to morbidity and mortality [3]. In most cases, the imaging findings are not specific to a particular pathology. However, they can provide sufficient information for an accurate differential diagnosis when combined with the pertinent clinical scenario.
Echocardiography is still the preferred initial imaging method for most patients with pericardial disease. However, in many clinical situations, a transthoracic echocardiogram is rarely sufficient [4]. Computed tomography (CT) and magnetic resonance imaging (MRI) have emerged as important alternatives or complementary tools to echocardiography for evaluating pericardial anatomic detail [2, 5]. To optimally manage a patient with suspected pericardial disease, it is necessary to know the major imaging modalities and select the appropriate study for each patient [3].
In this review we will identify selected entities affecting the pericardium, from benign to malignant, with a brief description of their clinical characteristics and provide a deep review of the imaging findings from conventional radiology to MRI, emphasising the ancillary findings that aid in the differential diagnosis approach.
2 Anatomy of the Pericardium and Pericardial Recesses
The pericardium is a sac surrounding the heart with an inner double-layered serous and a fibrous outer layer. The inner layer is subdivided into a visceral layer (epicardium) that surrounds the heart and great vessels, and a parietal layer that outlines the fibrous component [6]. The serosal layer has some reflections that are arranged around two tubes: one surrounding the aorta and pulmonary trunk, and the other one surrounding the superior vena cava, the inferior vena cava, and the four pulmonary veins [6].
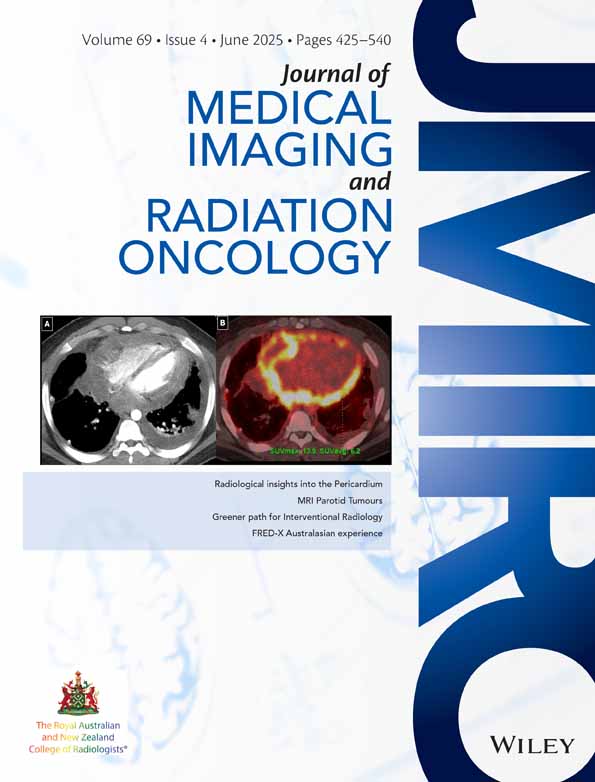
When a serosal layer reflects back upon itself, it is known as a recess, and when it is a fluid channel, it is known as a sinus. The pericardial sinuses connect the pericardial recesses [6]. Routine visualisation of the pericardial recesses on CT is common even in the presence of a normal amount of fluid (Figure 1).
2.1 The Transverse Sinus
The transverse sinus is the space between the aorta and the pulmonary trunk, posterior to the aorta, and above the left atrium. It is divided into superior aortic recesses, inferior aortic recess, right and left pulmonic recesses, and postcaval recess.
2.2 The Oblique Sinus
The oblique sinus is a basin separated from the transverse sinus by a double reflection of serous pericardium. It is located superior to and posterior to the left atrium, and superomedial to the left superior pulmonary vein.
The pericardial cavity drains to both the thoracic duct and the right lymphatic duct (Bogaert).
3 Normal Pericardium in Imaging
The pericardium is not generally visible on chest radiography ‘vide infra’, but it can be seen on CT and MRI. On CT, it appears as a thin band of soft tissue that extends from the great vessels at the top to the diaphragm at the bottom. Its thickness usually ranges from 1 to 2 mm [6, 7], and a measurement of less than 4 mm is considered normal [7]. It is usually not seen over the lateral surface of the left ventricle. Pericardial enhancement is more clearly visible in the portal venous phase (usually 70–75 s after the initiation of intravenous contrast).
On MRI, the normal serous pericardium demonstrates low signal intensity on steady-state free precession, T1-weighted, and T2-weighted sequences [2]. On MRI, pericardial thickness varies from 1.2 mm in diastole to 1.7 mm in systole [2].
4 Conditions of the Pericardium
4.1 Air, Collections, Haemorrhage, and Cardiac Tamponade
4.1.1 Pneumopericardium
Pneumopericardium is the presence of gas in the pericardial space, indicating a breach of pericardial integrity. It is often observed in cases of trauma and iatrogenic settings following surgery. Rarely, intubated patients, particularly children, develop pneumopericardium due to barotrauma associated with positive pressure ventilation [8]. This phenomenon is related to congenital defects in the pericardium as the mediastinal and pericardial spaces do not usually communicate.
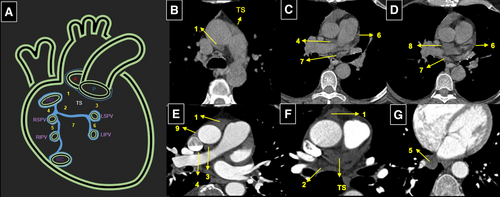
Small amounts of gas in the pericardium may not be detectable on chest radiographs. When there is enough gas, it becomes visible as a radiolucent zone, commonly referred to as a ‘halo’, encircling the heart (Figure 2). CT scans may reveal the underlying cause. MRI is not a practical option for these patients, given the susceptibility of the gas to create artefacts in the pericardial space and degrade image quality.
4.1.2 Pericardial Effusion
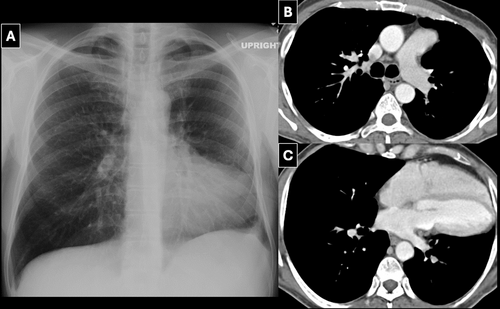
Similar to pleural effusion, pericardial effusion can be an early sign of heart disease. The normal volume of pericardial fluid is usually less than 50 mL [9]. Effusions less than 200 mL are usually not visible on a chest radiograph [10, 11]. The following conditions may be seen with pericardial effusion: systemic lupus erythematosus, rheumatoid arthritis, Sjogren's syndrome, dermatomyositis, acute viral or bacterial infections, tuberculosis, cardiac and renal failure (uremia), radiation, surgery, hypothyroidism, malignancy, myocardial infarction, and trauma [8]. Pericardial effusion can be classified as either transudates or exudates. Transudates tend to resorb on their own, while exudates can lead to loculation, calcification, and/or constriction [12].
Enlargement of the cardiac silhouette, depicting a globular configuration (water bottle), is the most sensitive sign for detecting a pericardial effusion on radiography [10] (Figure 3). When an effusion is large, the most peripheral centimetre of the cardiac silhouette may be less dense (owing to the lack of heart in this zone). This finding is known as the ‘variable density’ sign.

On a lateral projection, the expansion of the pericardium can be observed through the loss of the retrosternal space and posterior bulge signs. The pericardial fat stripe is the depiction of fluid density between the epicardial and pericardial fat, which is typically more prominent adjacent to the right ventricle. This can be seen on lateral radiography and is described as the ‘Oreo cookie or sandwich sign’ [13, 14]. Loculated pericardial effusion may occur due to adhesions and may cause pericardial tamponade [15].
4.1.3 Hemopericardium and Pericardial Hematoma
Hemopericardium may follow a ruptured ascending aortic aneurysm, type A aortic dissection, trauma, myocardial infarction, iatrogenic injury, anticoagulant therapy, and malignancy [8]. Patients typically present with acute chest pain. Rapid accumulation of fluid can cause cardiac tamponade.
CT can demonstrate increased density (usually above 30 HU) and may also provide clues for potential causes of bleeding within the pericardium. High signal intensity on T1-weighted MR images usually indicates the presence of haemorrhage [16].
4.1.4 Pericardial Collections
Pericardial collections may have a mass-like appearance, particularly in cases related to iatrogenic, postsurgical, or traumatic causes. In the absence of recent surgery, the presence of gas may be indicative of infection (Figure 4) or a fistula.

4.1.5 Cardiac Tamponade
The presence of fluid, gas, or soft tissue in the pericardium can increase intrapericardial pressure, leading to a concomitant decrease in left ventricular filling and stroke volume. Tamponade development depends on the volume, rate of accumulation, and stiffness of the pericardium [17]. The most common causes are related to trauma, rupture after a myocardial infarction, ruptured ventricular or coronary aneurysm, or aortic aneurysm/dissection [17].
The CT findings may include enlargement of the superior and inferior vena cava, periportal edema, and reflux of contrast material to the inferior vena cava and azygos vein. Enlargement and retrograde contrast reflux of the renal and hepatic veins have also been reported [17]. Compression of the coronary sinus may indicate the onset of cardiac tamponade. Other signs to look out for include early diastolic collapse of the free right ventricular wall (notch), late diastolic collapse of the right auricle wall, and impaired heart relaxation of the constriction [17]. Secondary signs may include a large inferior vena cava, fluid level in the inferior vena cava, and venous retrograde collateral pathways. A useful diagnostic indicator is a flattened heart sign, which is characterised by a decreased anteroposterior diameter and flattened anterior surface [17]. Focal tamponade could occur secondary to pericardial collections.
4.2 Acute and Chronic Pericarditis
Pericarditis is an inflammation of the pericardium, which can be caused by various etiologies such as infection, connective tissue disorders, radiation, uremia, myocardial infarction, and idiopathic [18, 19]. Symptoms of acute pericarditis depend on the severity of inflammation but typically include pleuritic-type retrosternal chest pain that worsens with inspiration, accentuated in the supine position [20]. CT and MRI commonly show pericardial thickening and effusion [17]. Pericardial thickening on CT is associated with homogeneous enhancement of the pericardium best seen on portal venous phase. On MRI, STIR images show high signal of pericardial fluid or pericardial edema [17]. Pericardial enhancement and epicardial fat enhancement are also visible. Enhancement of the visceral and parietal pericardium suggests pericarditis (split pericardial sign) [12].
Chronic pericarditis is defined as lasting more than 3 months [21, 22]. The gradual accumulation of fluid over time in chronic pericarditis can cause pericardial distention, allowing for more fluid to develop before tamponade occurs [23]. Irregularity or nodular thickening of the pericardium, with or without calcification, highly suggests chronic pericarditis [13]. Exuberant epicardial fat stranding may also indicate chronic pericarditis.
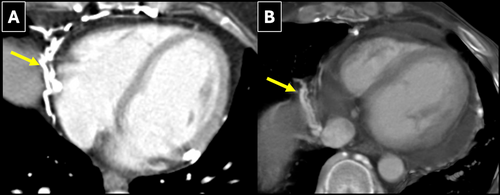
4.3 Constrictive Pericarditis
Constrictive pericarditis is a slow process caused by a non-elastic pericardium due to thickening (fibrosis or calcification) of the serosal layers [2]. This condition is a consequence of previous episodes of pericarditis or could be related to other causes such as TB, cardiac surgery, and radiotherapy [12, 24]. It is clinically significant because it impairs left ventricular diastolic filling, resulting in elevated systemic venous pressures and low cardiac output. Symptoms that resemble cardiac failure are present [2]. Constrictive pericarditis frequently affects the parietal pericardium, but it can occasionally involve the visceral layer. Thickening of the pericardium (> 4 mm) and/or calcification are indicative signs, but not always specific [7]. Diastolic interventricular septal flattening has a sensitivity of 62%–81% and specificity of 93%–100% for constriction [25]. The amount of calcium required for constriction is variable. The absence of pericardial thickening or calcification does not exclude the diagnosis; functional MRI may be useful for diagnosis, demonstrating loss of pericardial compliance. Although not specific, ventricular septal bounce (in diastole) can solidify the diagnosis when accompanied by other concomitant findings. This bounce can be exaggerated during deep inspiration and is known as interventricular interdependence, a finding highly suggestive of constriction [25].
Rarely, a subacute pericardial effusion will impede diastolic relaxation because of its thick, jelly-like consistency. This effusion is not as acute or large as one that results in tamponade and is not as chronic as constrictive pericarditis. This intermediary condition is known as ‘effusive constriction’. Its diagnosis can impact management. Whereas tamponade is acutely drained and constrictive pericarditis may be referred for surgical pericardial stripping, the diagnosis of effusive constriction will result in a change of medications to try and prevent progression to constriction [25].
4.4 Pericardial Neoplasms
The pericardium and the pleura share some characteristics, one of which is that primary neoplasms are rare and metastatic disease is more common [2, 17].
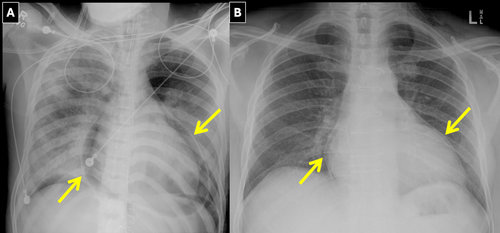
Metastases may be hematogenous as in breast, lung, kidney, melanoma, and myeloma [17, 26]. They may also be from direct extension, most notably thymoma and lymphoma. Mesothelioma represents the most common pericardial primary tumour. Others include sarcoma, lymphoma, malignant teratoma, and hemangioendothelioma [17]. Pericardial effusion is the primary sign in both etiologies. Up to 1/3 of patients have a known history of asbestos exposure [1]. Spread to the pericardium can occur through lymphatic channels or direct invasion [17]. Nodular and/or irregular thickening of the pericardium with enhancement is usually seen. Some of these nodules may be seen extending into the epicardial fat akin to stalactites. Effusion, often large, is associated and sometimes may be hemorrhagic. Masses and nodules, diffuse plaques, and hemorrhagic pericardial effusion are seen in mesothelioma, and it should be noted that pericardial mesothelioma is the most common primary malignant tumour of the pericardium [2]. Most neoplasms have low signal intensity on T1-weighted images and high signal intensity on T2-weighted images. Metastatic disease may be hematogenous or by direct extension; it tends to progress rapidly. Metastatic pericardial implants are often small (Figure 5). They may be difficult to visualise on MR [2]. FDG increased uptake could be seen.
4.5 Congenital Lesions
4.5.1 Congenital Absence of the Pericardium
It is considered to be premature atrophy of the left common cardinal vein resulting in loss of blood supply to the left pleuropericardial membrane. A complete absence of the pericardium on the left side is more common than a partial defect. 30% to 50% of pericardial defects may be associated with congenital anomalies of the heart, lungs, chest wall, and diaphragm [27, 28]. Complete absence of the parietal pericardium is a benign condition compatible with normal life expectancy. In rare cases, herniation of the heart or its appendages through the defect can cause arrhythmias, angina, syncope, and, rarely, sudden death due to strangulation.
It can present on radiographs as a leftward and posterior rotation of the heart, as most defects are left-sided [28]. On CT, a sharp distinction between the main pulmonary artery and the transverse aorta is due to the interposition of the lung. In cases of partial absence, a bulge around the left atrial appendage may be the only radiographic finding (Figure 6). On CT and MRI, the heart is typically rotated toward the left chest with the lung interposed between the aorta and pulmonary artery. Lack of visualisation of the pericardium is not sufficient for diagnosis, as the entire pericardium is not normally seen.
4.5.2 Pericardial Cysts
Benign mesothelial line cysts occur in 1 in 100,000 patients [12]. Most occur at the right cardiophrenic angle [12]. On chest radiograph, the cyst usually appears as a round or oval opacity touching the hemidiaphragm and anterior chest wall.
On CT and MRI, pericardial cysts commonly appear as thin-walled, round or ovoid lesions with uniform internal attenuation or signal. A pericardial diverticulum has a similar appearance; however, it maintains a small communication with the pericardial space.
4.6 Mimics of Pericardial Disease
4.6.1 Pericardial Varices
The pericardial veins are part of the deep venous drainage of the thorax. Varices may be secondary to obstruction of the upper thoracic and cervical venous systems and portal hypertension among others [29-31]. They should not be confused with mediastinal masses or lymph nodes (Figure 7).
4.6.2 Infarcted Fat Pad
Sometimes known as pericardial fat pad necrosis or epipericardial fat pad necrosis, this condition represents an inflammatory process of the mediastinal fat surrounding the heart and pericardium. It presents with acute chest pain and is rarely associated with trauma and ischaemia [32]. An area of necrosis appears as an encapsulated fat-density mass with surrounding inflammatory changes that has an appearance similar to fat necrosis in other parts of the body [32].
5 Conclusions
Pericardial diseases encompass a broad range of conditions. CT and MRI are increasingly used as complementary imaging techniques for the assessment of pericardial diseases. They can provide valuable clinical information in addition to echocardiography. CT, MRI, and conventional radiology can detect subtle signs of pericardial disease and may provide relevant information for an accurate diagnosis.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The authors have nothing to report.