Utility of 68Ga prostate specific membrane antigen – positron emission tomography in diagnosis and response assessment of recurrent renal cell carcinoma
Abstract
Introduction
Prostate specific membrane antigen (PSMA) positron emission tomography (PET) is an emerging imaging modality in prostate cancer. However, 68Ga-PSMA-PET may also have diagnostic utility in the setting of renal cell carcinoma (RCC). We investigate the differential role of 18F-fluorodeoxyglucose (FDG) and PSMA-PET/CT scanning in patients with oligometastatic RCC. In particular, we focus on the utility of PSMA-PET for diagnostic evaluation of isolated or limited metastases planned for local surgery or radiation, as well as the potential utility of PSMA-PET for therapeutic response assessment in patients receiving stereotactic ablative body radiotherapy (SABR).
Methods
We present a retrospective series of eight patients in which comparative imaging modalities are evaluated against PSMA-PET scanning. FDG-PET and PSMA-PET scans were performed prior to definitive treatment (either surgery or SABR) of limited recurrent disease. Response assessment after SABR was performed with both PET imaging modalities at multiple time points in a subset of four patients.
Results
Prostate specific membrane antigen uptake is typically more intense than FDG in RCC. In all but two cases, one of which was papillary carcinoma, FDG-PET and PSMA-PET are concordant for detection of sites of disease. We demonstrate for the first time the differential kinetics of post-treatment response using PSMA and FDG-PET, with a more rapid metabolic response observed on FDG-PET. Both modalities demonstrate response earlier than morphological appearances on CT or MRI imaging.
Conclusions
Our series suggests that PSMA shows early promise as a diagnostic and therapeutic response assessment tool in patients with metastatic RCC receiving definitive local therapies.
Introduction
The utility of PSMA directed radionuclide tracers for diagnostic purposes in prostate cancer is being increasingly recognized. Despite the specificity implicit in its nomenclature, PSMA is highly expressed in the cell surface of the tumour microvasculature of several solid tumours including RCC.1 This entity is very heterogeneous, with a broad spectrum of presentations ranging from indolent to aggressively proliferative disease. A subgroup of patients with limited metastatic burden from RCC, termed oligometastatic disease, is increasingly being managed with definitive local therapies. Treatments such as extirpation, thermal ablation and stereotactic ablative body radiotherapy (SABR) are delivered with the aim of long-term disease control and perhaps even cure.2 Identifying those patients with truly isolated or limited metastatic spread necessitates improved modalities over conventional computed tomography (CT) or whole body bone scan. In this context, PSMA-PET may allow for improved diagnostic sensitivity for otherwise radiologically occult metastatic disease. Prior to this analysis, a sum total of seven patients have been reported in the literature via case reports addressing the diagnostic utility PSMA-PET for metastatic RCC.3-5
Stereotactic ablative body radiotherapy is a high-precision radiotherapy technique that involves delivery of ablative doses of radiation in a single or few treatment sessions. In the context of oligometastatic RCC, SABR appears to be associated with high rates of tumour control with relatively few associated side effects.6 The investigation of local treatment modalities in these patients, including SABR, is the subject of numerous scientific enquiries. In this case series, we report the diagnostic utility of 68Ga-PSMA-PET/CT for evaluation of disease extent in patients with putative oligometastatic disease in comparison with conventional and 18F-FDG-PET/CT imaging. Additionally, we focus on the role of response assessment using post-therapy using PSMA-PET.
Methods
This descriptive report outlines the impact of 68Ga-PSMA-11 (HBED-CC) PET/CT on the management of a series of eight patients who underwent screening and/or response assessment investigations. This was a retrospective case series of consecutive patients with oligometastases planned for definitive local therapies. All patients were discussed at a multidisciplinary tumour board and were recommended for SABR when medically inoperable, or when surgery was considered technically high risk or overly morbid. A list of the patient cases can be found in Table 1.
| Case | Age | Sex | Fuhrman grade | SUVmax on PSMA | SUVmax on FDG |
|---|---|---|---|---|---|
| 1 | 76 | F | 2 | 5.3 | 7.0 |
| 2 | 60 | F | 4 | 26.5 | – |
| 3 | 78 | F | 3 | 15.9 | 3.4 |
| 4 | 73 | M | 3 | 8.6 | 3.1 |
| 5 | 60 | M | 3 | 6.7 | 4.0 |
| 6 | 70 | M | 2 | 0 | 0 |
| 7 | 52 | M | 3 | 5.6 | 5.4 |
| 8 | 50 | F | N/A (papillary) | 0 | 3.6 |
68Ga was eluted from an onsite 68Ge/68Ga generator (Isotope Technologies Garching, ITM, Germany or iThemba LABS, Cape Town, South Africa) and compounded on-site with HBED-PSMA11 (Advanced Biochemical Compounds, ABX, Radeberg, Germany) using a manual technique. The product was released following quality control including high performance liquid chromatography (HPLC). 150 MBq ± 50 MBq of 68Ga-HBED-PSMA11 was administered intravenously. Following 60 minutes, images were obtained on a hybrid PET/CT device (General Electric Discovery 690 or Siemen's Biograph 64).
Case 1
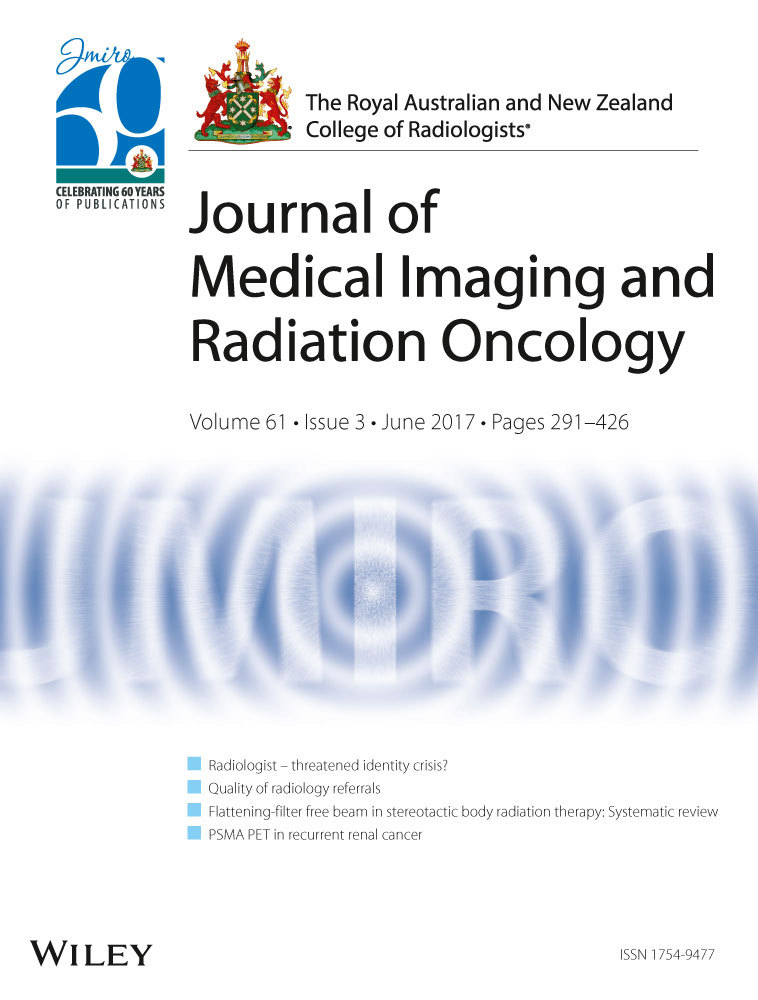
Seventy-six-year-old female with a suspected isolated renal bed recurrence of a Fuhrman grade 2 clear cell carcinoma. FDG-PET demonstrated three sites of disease and the patient was considered a candidate for SABR. The subsequent PSMA-PET demonstrated a total of five sites of disease, and patient was subsequently referred for systemic therapy (Fig. 1).

Case 2
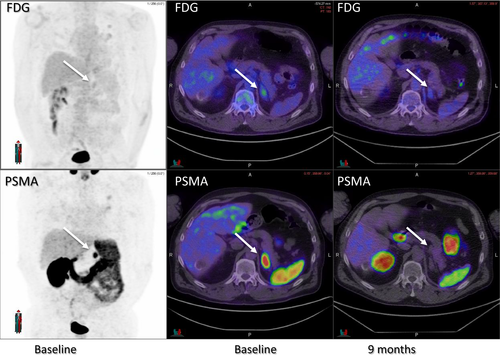
Sixty-year-old male who initially underwent left nephrectomy and left lower lobectomy for synchronous presentation of solitary metastasis of a Fuhrman grade 3 clear cell carcinoma. At 9 months after the initial presentation, he received SABR for two further pulmonary metastases, and at 18 months he presented with an enlarging left adrenal metastasis. This lesion was mildly FDG-avid and intensely PSMA avid (Fig. 2), without evidence other sites of disease, and subsequently received a single fraction of 26 Gy of SABR. This lesion demonstrated a complete PSMA-PET response at 9 months.
Case 3
Seventy-eight-year-old female with a biopsy proven right renal bed recurrence of Fuhrman grade 3 clear cell carcinoma (Fig. 3). The cancer had low FDG-avidity, and intense PSMA avidity. After treatment with 42 Gy in three fractions of SABR, slowly evolving reduction in PSMA activity is demonstrated over 12 months.
Case 4
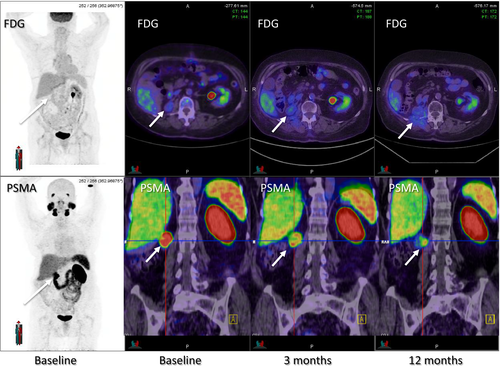
Seventy-three-year-old man with two left lower lobe pulmonary metastases from Fuhrman grade 3 clear cell carcinoma, treated with 48 Gy in four fractions of SABR. The cancers were moderately FDG-avid and intensely PSMA avid at baseline, with a differential pattern of response at 3 and 9 months on both imaging modalities. Inflammatory PSMA and FDG uptake in surrounding lung parenchyma post-SABR was noted (Fig. 4).
Case 5
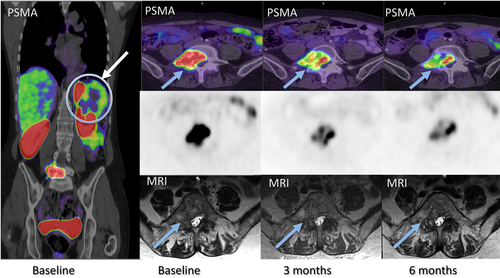
Sixty-year-old female with solitary biopsy confirmed L5 metastasis with synchronous 75 mm Fuhrman grade 4 left primary clear cell carcinoma. PSMA-PET demonstrated intense avidity within L5 and excluded occult metastatic disease, and therefore this lesion was treated with 30 Gy in three fractions of SABR in an effort to obtain durable local control. Complete resolution of the patient's neuropathic pain and ongoing reduction of PSMA activity at 3 and 6 months was noted despite stable correlative MRI appearances (Fig. 5).
Case 6
Seventy year old presented with an enlarging 40 mm right adrenal metastasis after previous clear cell carcinoma resected 17 years prior. Despite no uptake on both FDG and PSMA-PET scan, a core biopsy confirmed Fuhrman grade 2 clear cell carcinoma. The patient was deemed medically inoperable due to cardiovascular and respiratory comorbidities. The patient subsequently underwent SABR to a dose of 42 Gy in three fractions.
Case 7
Fifty-two-year-old male presented with a symptomatic metastasis in left greater trochanter and synchronous Fuhrman grade 3 right primary clear cell carcinoma. The metastasis was isolated and avid with both FDG and PSMA-PET scans, with greater FDG-intensity. Patient underwent cytoreductive nephrectomy, received 30 Gy in three fractions of SABR with symptomatic improvement and had no evidence of disease recurrence 8 months later on surveillance with FDG-PET.
Case 8
Fifty-year-old female with a 45 mm renal bed recurrence 4 years after nephrectomy for a right papillary RCC. The lesion was isolated and was FDG-avid; however, the lesion was not avid on PSMA-PET scanning. The patient subsequently underwent surgical resection that confirmed recurrent papillary RCC.
Discussion
Published literature regarding the utility of PSMA-PET in metastatic RCC is scarce. A case of 68Ga-PSMA-avid biopsy confirmed lymph nodal metastases from RCC was recently reported in the context of a patient having recurrent prostate carcinoma.3 Another single patient report described more intense 68Ga-PSMA than FDG-avidity in sites of metastases.4 In five patients with metastatic RCC, PSMA-PET detected more sites of disease than conventional imaging. Similar to our series, a broad variability of PSMA uptake intensity was observed,5 reflecting the inherent biological heterogeneity of RCC.
A unique aspect of our series is that we directly compared the diagnostic utility of FDG and PSMA radiotracers in the evaluation of disease extent. While FDG-PET/CT can reliably identify extra-renal sites of RCC with a reported pooled sensitivity of 91% and specificity of 88% on meta-analysis, indeterminate lesions are still common, particularly as lesion size decreased and with lower tumour grade.7 It is not in common use for RCC as FDG production is expensive, resource intensive and requires the use of cyclotron-based radiopharmaceutical production. By comparison, 68Ga generators are cheap, easy to manufacture and readily available with production analogous to the near ubiquitous Technetium generators found in most nuclear medicine departments.8 In our series, of the patients who had both PET imaging modalities (n = 7), the majority (n = 6) had concordant discrete sites of metastases on both FDG and PSMA scans. However, in one case the detection of additional sites of metastases through PSMA-PET had a significant impact on clinical management, as this patient was offered palliative systemic therapy rather than localized SABR. Furthermore, we typically observed higher uptake on PSMA uptake as compared to FDG uptake. Thus, from a diagnostic perspective, 68Ga-PSMA-PET and may be potentially more sensitive than FDG-PET for RCC while being easier and cheaper to perform. In men with elevated serum PSA readings and PSMA-avid bone metastases, particularly when sclerotic, bone biopsy could be considered in order to exclude the differential diagnosis of prostate cancer.
For the first time, we report the different kinetics of treatment response with FDG and PSMA-PET after radiotherapy. While monitoring treatment response with FDG-PET in metastatic RCC may have some utility, its role has not clearly been established.9 In particular, we observed that in FDG-avid metastases, PET response typically occurred within 3–4 months post-treatment. By comparison, the evolution of PSMA-PET responses was delayed, with ongoing decreases in PSMA intensity noted 6–12 months post-treatment. While the biological processes underlying these functional imaging differences are yet to be elucidated, we postulate that metabolic processes appear to be more sensitive to early disruption by ablative doses of radiation than established tumour neovasculature. This is consistent with well-established observations of morphologically persistent RCC metastases after stereotactic radiotherapy including contrast enhancement in vasculature on CT or MRI despite apparent long-term tumour control.10
Increased metabolic uptake in surrounding normal tissue as demonstrated on FDG-PET is a well-recognized effect of SABR. We have previously shown dose-dependent increase in the FDG-avidity of normal lung parenchyma routinely predates the radiological appearance of fibrosis on CT.11 While the increased FDG uptake is explained by metabolic inflammation, the biological mechanism of increased PSMA uptake in normal tissue secondary to radiation is not yet understood and warrants further investigation.
This preliminary case series demonstrates the utility of PSMA-PET/CT for imaging metastatic disease in RCC. Importantly in the context of this cohort of RCC, often with planned or prior nephrectomy, PSMA-PET scanning was not associated with nephrotoxicity. This is because PSMA-11 is a peptide-like compound administered in microgram ‘tracer’ doses. Similarly, no adverse events have been reported in the literature or clinical experience in the more common setting of prostate cancer. PSMA avidity was typically more intense than FDG-avidity, which is particularly important in the context of oligometastatic disease where improved diagnostic sensitivity may impact on management decisions regarding local therapies. Given that production is considerably easier than FDG as it does not require a cyclotron, 68Ga-PSMA-PET/CT is an attractive alternative for diagnostic functional imaging of patients with limited recurrence of RCC. Nevertheless, FDG-PET may remain complementary in the context of assessment of treatment response due to earlier reduction in post-treatment activity. At present, neither imaging technique is currently standard in RCC, but might be promising. The high uptake on PSMA observed in some patients also suggests possible utility of Lu-177-PSMA radionuclide therapy, an emerging treatment for prostate cancer, in selected patients with RCC and widespread disease not amenable to local therapies.