Hemithoracic radiation therapy after extrapleural pneumonectomy for malignant pleural mesothelioma: Toxicity and outcomes at an Australian institution
Abstract
Introduction
We aim to report the outcome of patients with malignant pleural mesothelioma who underwent extrapleural pneumonectomy (EPP) and adjuvant hemithoracic radiotherapy with or without chemotherapy at a single Australian institution.
Method
Between July 2004 and March 2013, 53 patients were referred for radiation treatment following EPP, of whom 49 were suitable for adjuvant treatment. Radiation treatment initially involved a 3D conformal, mixed electron/photon technique, delivering 45–50.4 Gy in 25–28 fractions (31 patients) and subsequently a nine-field intensity-modulated radiotherapy technique, delivering 50.4–54 Gy in 28–30 fractions (18 patients). Fifty-five per cent of patients also received pre-operative chemotherapy. We assessed toxicity, disease-specific and overall survival in patients who commenced radiation treatment.
Results
Forty-one patients (84%) completed treatment as prescribed. Six patients stopped prematurely due to toxicity, and two with disease progression. Most patients discontinuing due to toxicity received over 90% of the prescribed dose. Common acute toxicities included nausea, fatigue, anorexia and dermatitis. Severe early toxicities were rare. Late toxicities were uncommon, with the exception of a persistent elevation in liver enzymes in those with right-sided disease. Neither clinical hepatitis nor radiation pneumonitis was documented. With a median follow up of 18.7 months, median disease-free and overall survival were 21.6 and 30.5 months, respectively, and 2-year overall survival was 57.3%.
Conclusion
Hemithoracic radiotherapy following EPP, although associated with significant early toxicity, is well tolerated. Most patients complete the prescribed treatment, and clinically significant late toxicities are rare.
Introduction
Malignant pleural mesothelioma (MPM) is a rare malignancy which has a poor prognosis. Australia has among the highest rates of mesothelioma in the world,1 with a rising incidence expected to peak by 2021.2
Most patients diagnosed with pleural mesothelioma present late, with extensive local or metastatic disease, and are treated with palliative intent. Treatment options include pleurodesis, systemic chemotherapy, local radiation treatment, analgesia or a combination of these. In patients with localised, potentially resectable disease, the optimal management remains controversial. Surgical management is divided between extrapleural pneumonectomy (EPP) or pleurectomy/decortication. EPP involves en bloc removal of the ipsilateral parietal and visceral pleura, lung, and often the pericardium and diaphragm, as well as mediastinal lymph node dissection. This procedure is distinct from pleurectomy/decortication where the lung, or part thereof, is left behind.
Despite the extent of surgery, most surgeons agree that obtaining clear margins is difficult, and local recurrences are common.3 Radiation treatment has been shown to reduce local recurrence following EPP and forms part of a radical, multimodality treatment approach in selected patients with MPM.4, 5 Hemithoracic radiation treatment following EPP poses a significant dosimetric challenge in order to ensure adequate coverage of the target volume while respecting the tolerances of critical structures (especially the contralateral lung, spinal cord, liver and heart). Conventional techniques, often utilising a mix of photon and electron fields, are limited by marked dose uncertainty, and these have been associated with in-field recurrences.6 Intensity-modulated radiotherapy (IMRT) has been employed to optimise dose distribution; however, this has come at a cost of increased lung toxicity, including early reports of fatal radiation pneumonitis.7, 8
In this study, we present a large series of patients treated with adjuvant hemithoracic radiation treatment following EPP at an Australian institution and report on our experiences with tolerability, adverse events and clinical outcomes.
Methods
Inclusion
Patients referred to Royal Prince Alfred Hospital for adjuvant radiotherapy following EPP, with or without, neoadjuvant chemotherapy were analysed. EPP was recommended to patients with good performance, adequate cardiac and pulmonary function, and non-bulky disease limited to the ipsilateral thorax. To be considered for radical intent adjuvant radiation treatment, patients were required to have recovered from surgery adequately, have good performance and have no evidence of disease progression. All patients who received adjuvant radiation treatment with radical intent were included in this review.
Radiotherapy technique
Between July 2004 and January 2010, patients were treated using a 3D conformal, mixed electron (9–16 MeV) and photon (6 MV) technique (EPT), adapted from the Memorial Sloan Kettering Cancer Center technique.9 The prescribed dose was 45–50.4 Gy in 25–28 fractions. Five patients received a boost of 5.4–10 Gy to areas of involved margin or otherwise deemed to be at high risk of local recurrence, determined in close collaboration with the operating surgeon.
From March 2010, we introduced a nine-field IMRT technique using six MV photons (Fig. 1). The beam arrangement limited entry beams to within a 200-degree radius on the ipsilateral side, leaving 160 degrees free from entrance beams. This technique allows maximal sparing of the contralateral lung.10 The prescribed IMRT dose was 50.4–54 Gy in 28–30 fractions. A focal boost of 5.4–12 Gy was also used in four cases.
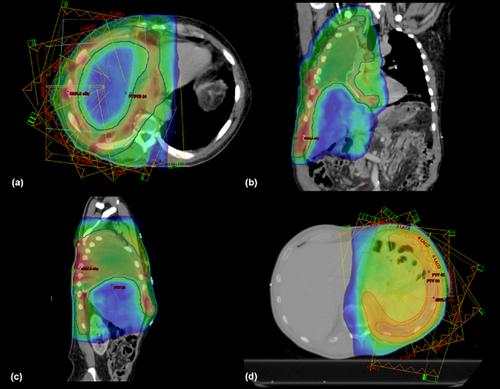
Field arrangement and dose distribution in right-sided disease, axial (a) coronal (b) sagittal (c). Field arrangement and dose distribution in left-sided disease (d). Note sparing of liver, contralateral lung and abdominal contents.
All patients underwent CT planning with vacuum bag immobilisation. The clinical target volume (CTV) included the entire pleural bed over the chest wall, mediastinum, pericardium and diaphragm (including the retrocrural spaces), as well as the thoracotomy scar and any drain sites. If available, PET imaging was fused with the planning CT to assist in volume delineation and identification of areas at high risk of residual disease. The planning target volume was generated as a 1 -m isotropic expansion of the CTV. Bolus (0.5 cm) was applied to the thoracotomy scar and drain sites.
Mean dose to the remaining lung was limited to less than 8 Gy (MLD < 8 Gy). The lung V20 was limited to 10%, and the V5 to 60%. The mean liver dose was kept below 31 Gy, and the V30 to less than 30%. The ipsilateral kidney mean dose was limited to 30 Gy and the V30 to less than 50%, while the mean dose to the contralateral kidney was below 12 Gy, V15 less than 15% and V45 less than 10%. Dose to the spinal cord was less than 50 Gy. The heart V45 was limited to 30%, and mean heart dose to 40 Gy.
Assessment and statistical analysis
Toxicity was assessed using the Common Terminology Criteria for Adverse Events version 3.0. Early toxicity was assessed weekly during radiation treatment and included physical examination and laboratory studies (full blood count and electrolytes). For patients with right-sided disease, this also included weekly liver function tests. Following completion of radiation treatment, patients were reviewed three-monthly for the first year, and six-monthly thereafter. Follow-up included clinical examination and chest x-ray. Routine chest CT was introduced in 2007, and other imaging modalities were performed upon clinical indication. PET-CT was not used routinely for follow up but was employed where other imaging was equivocal for disease recurrence.
Local recurrence was defined as any clinical or radiological evidence of disease in the ipsilateral thorax, while distant metastases included any disease outside the ipsilateral thorax. Local relapse-free survival (LRFS), distant metastasis-free survival (DMFS), disease-free survival (DFS) and overall survival (OS) were estimated using the Kaplan–Meier method, calculated from first day of treatment (chemotherapy or EPP). Differences in local recurrence and survival for prognostic and treatment factors were tested for significance by the log-rank test. Prognostic factors included age, gender, histology, tumour laterality and stage. Treatment factors that were assessed included chemotherapy use, radiation technique (EPT or IMRT) and radiation dose delivered. The threshold for significance was P < 0.05. Factors found significant were then tested in a multivariate model using Cox proportional hazards regression.
Results
Fifty-three patients were referred for radiation treatment following EPP between July 2004 and March 2013 (Table 1). Twenty-seven patients (55%) had received neoadjuvant chemotherapy, consisting of pemetrexed and a platinum agent. Adjuvant treatment was not recommended for four patients (three patients had poor post-operative performance and one patient developed disease progression); thus, 49 patients commenced radiotherapy.
| Characteristic | Value | % |
|---|---|---|
| Gender (n) | ||
| Male | 43 | 87.8 |
| Female | 6 | 12.2 |
| Age (years) | ||
| Median | 63 | NA |
| Range | 33–76 | NA |
| Laterality (n) | ||
| Right | 26 | 53.1 |
| Left | 23 | 46.9 |
| Histological subtype (n) | ||
| Epithelial | 41 | 83.7 |
| Biphasic | 8 | 16.3 |
| Pathological stage (n) | ||
| Stage I–II | 17 | 34.7 |
| Stage III–IV | 32 | 65.3 |
| T stage (n) | ||
| T1 | 8 | 16.3 |
| T2 | 15 | 30.6 |
| T3 | 24 | 50 |
| T4 | 2 | 4.1 |
| N stage (n) | ||
| N0 | 35 | 71.4 |
| N1 | 2 | 4.1 |
| N2 | 12 | 24.5 |
| Neoadjuvant treatment (n) | ||
| Induction chemotherapy | 27 | 55.1 |
- NA, not applicable.
Patients were aged from 33 to 76 years (median 64 years) and were predominantly male (88%). The majority of patients had epithelioid histology (84%), the remainder having biphasic tumours; 71% (35 patients) were lymph node negative. Forty-one patients (84%) completed treatment as prescribed. Six patients stopped treatment prematurely due to toxicity (of whom five received more than 90% of the prescribed dose) and two due to disease progression. Only one patient required a treatment break due to a thoracic cavity infection; however, he ultimately completed the prescribed course.
Thirty-one patients (63%) were treated with a mixed EPT and received doses of 9.0–55.0 Gy, with a median dose of 45 Gy. The 18 patients (37%) treated with IMRT received 5.4–63.8 Gy with a median of 54 Gy (Table 2).
| EPT | IMRT | |
|---|---|---|
| Patients (%) | 31 (63.3) | 18 (36.7) |
| Dose prescribed | ||
| Range (Gy) | 40–55 | 50.4–66 |
| Mean (Gy) | 46.7 | 54.4 |
| Median (Gy) | 45.0 | 54.0 |
| Fractions | 25–30 | 28–30 |
| Dose delivered | ||
| Range (Gy) | 9–55 | 5.4–63.8 |
| Mean (Gy) | 45.2 | 50.5 |
| Median (Gy) | 45.0 | 54.0 |
- EPT, electron/photon technique; IMRT, intensity-modulated radiotherapy.
Early toxicity
Commonly seen toxicities are summarised in Table 3. Low-grade nausea, anorexia and fatigue were near universal; however, severe (grade 3) skin toxicity, nausea and oesophagitis were 8%, 6% and 2%, respectively. The reasons for early cessation of treatment were nausea (two), biochemical (subclinical) hepatitis (one), grade 3 oesophagitis (one) and thrombocytopenia (one). One patient developed a Pneumocystis carinii pneumonia shortly after completion of radiation treatment and required intensive care admission. There were no cases of radiation pneumonitis. One patient developed a thoracic cavity infection and required intravenous antibiotics.
| Toxicity (grade) | Patients | % |
|---|---|---|
| Early | ||
| Skin (≥2) | 23 | 47 |
| Skin (≥3) | 4 | 8 |
| Nausea (≥3) | 3 | 6 |
| Oesophagitis (≥3) | 1 | 2 |
| Late | ||
| Liver (≥2) | 14 | 29 |
| Liver (≥3) | 6 | 12 |
| Pneumonitis | 0 | 0 |
Late toxicity
Persistent elevation in the liver enzymes alkaline phosphatase (ALP) and gamma-glutamyltransferase (GGT) was a common late finding. Of those treated with right-sided disease (26 patients), nine (35%) developed elevations in ALP or GGT of greater than 2.5 times the upper limit of normal (grade ≥ 2). Grade 2–3 liver toxicity was more common in patients treated with a conventional technique (50%) versus IMRT (10%) (Fisher's exact P = 0.087). No patients developed clinical hepatitis.
One patient with long-standing ureteric dilatation developed progressive pelvico-ureteric junction obstruction. He was initially planned for pyeloplasty; however, significant perinephric fibrosis precluded this procedure and he ultimately required a right nephrectomy 15 months after completion of radiotherapy. Radiotherapy was to the right hemithorax, with the right renal hilum and ureter receiving up to 35 Gy. One patient with left-sided disease presented with signs and symptoms of biventricular failure 3 months following completion of radiation, and was found to have a pericardial effusion and constrictive pericarditis. The diaphragmatic patch was removed, and although initially the patient had a good response to therapy, he ultimately succumbed to right heart failure 12 months later, without evidence of recurrence. Mean heart dose was 38.3 Gy, V45 was 44%, and no volume received more than 47 Gy. Both of these patients were treated with the conventional EPT technique. Finally, there was one case of suspected myelitis 10 months after radiation treatment, in a patient presenting with lower limb paraesthesia. Magnetic resonance imaging demonstrated subtle signal change in the thoracolumbar spine and thickening of the proximal cauda equina. Maximum dose over this length of cord did not exceed 40 Gy in 30 fractions. The patient's symptoms proved self-limiting, and he remains free of any neurological compromise and without evidence of disease.
Clinical outcomes
Median follow up was 18.7 months. Nine patients (18.4%) developed a local recurrence at a median of 7 months (range 1–34 months) from radiation treatment. Sufficient imaging was available in five patients to adequately assess the site of recurrence. Three patients recurred in the costophrenic recess, in areas of field junctioning and dose uncertainty. One patient failed in-field at the ipsilateral diaphragmatic crus, 16 months after completion of radiation. Treatment in this patient was stopped early at 45 Gy due to anorexia and psychological distress. There was one out-of-field recurrence along a drain site within the ipsilateral breast tail. LRFS at 1 year and 2 years was 91.0% and 85.0%, respectively; 23 patients (46.9%) developed distant metastases. Fifteen patients relapsed in the abdomen, predominantly with peritoneal disease or malignant ascites. One patient had liver metastases at first failure, and one patient presented with a splenic metastasis. Seven patients failed in the contralateral hemithorax, and three patients were found to have bony metastases at first progression. DMFS at 1 year and 2 years was 75.5% and 54.6%, respectively, with a median DMFS of 32.4 months.
DFS at 2 years was 46.1%, and median DFS was 21.6 months. OS at 1, 2 and 3 years was 83.7%, 57.3% and 42.2%, respectively (Fig. 2). Median survival was 30.5 months. Seven patients (14%) were still alive beyond 5 years.
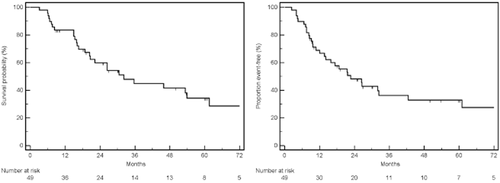
Kaplan–Meier curves of overall survival (left) and disease-free survival (right).
There was a trend for longer DFS in the node negative patients, 26.6 months, versus 10.8 months in those with positive nodes. This difference did not reach statistical significance (log-rank P = 0.07). Female gender was associated with increased local recurrence on univariate analysis (P = 0.03); however, this association was not maintained in the multivariate model. Only pathological stage was found to be a statistically significant predictor of outcome. The use of neoadjuvant chemotherapy, radiotherapy technique (EPT or IMRT) or delivered radiation dose did not predict for local or distant control or OS.
Discussion
Our series of 49 patients, recruited over 8 years and treated definitively, is large for this rare disease, which often presents at a late stage when aggressive local treatment is inappropriate. Most published series have reported on fewer than 40 patients receiving radiation treatment.11-15 We analysed outcomes for all patients who commenced radiotherapy with a long median follow-up of 18.7 months. This represents the largest such series published in Australia.
Our data indicate that radiation treatment following EPP is well tolerated, with only 12% of patients discontinuing treatment early due to toxicity, the majority of those receiving at least 90% of the prescribed dose. A West Australian series12 reported on 36 patients referred for tri-modality therapy with adjuvant chemotherapy and radiotherapy, of whom 22 ultimately had EPP, and 15 received adjuvant radiotherapy. One patient (6.7%) discontinued radiotherapy early due to disease progression. In a recent prospective Italian series, 32 patients received adjuvant radiation treatment with 10 (31%) stopping prematurely.14 De Perrot et al. described 35 patients receiving hemithoracic radiotherapy, of whom five (14%) failed to complete the prescribed treatment.11
Despite EPP and hemithoracic radiation being intensive treatments, with patients often requiring lengthy post-treatment recovery, long-term treatment complications were uncommon. Most patients experienced low-grade nausea and fatigue, and the majority required anti-emetics during radiation treatment. However, only two patients in this series required inpatient supportive care. Highly conformal IMRT has been used to spare organs at risk (especially spinal cord, liver and heart), at the expense of increased contralateral lung dose. The adoption of IMRT was initially associated with high rates of severe radiation pneumonitis at some centres.10, 16 A large series of 86 IMRT patients has reported rates grade 3 or higher pulmonary toxicity of 11.6%.17 This series also reported three deaths from radiation pneumonitis. With a heightened awareness of this toxicity, and the adoption of conservative dose constraints to the remaining lung,18 we have had no cases of radiation pneumonitis in this series.
Maintaining adequate dose coverage, especially in the posterior costophrenic recess, while observing liver tolerance is a significant dosimetric challenge for right-sided disease. Subclinical hepatitis, with elevations of liver enzymes greater than 2.5 times ULN, was common, seen in 35% of patients treated for right-sided disease. There were, however, no cases of clinically evident hepatitis, and in the majority of patients, enzyme levels normalised within 2 years. There have been at least two reported cases of fatal hepatitis following hemithoracic radiotherapy19, 20; however, the pattern of subclinical changes in liver enzymes have not been previously described. One study demonstrating radiological changes in the liver following hemithoracic IMRT found the majority of these resolved on follow-up imaging, up to 54 weeks.21 Following the implementation of IMRT, our incidence of grade 2 or higher liver toxicity was reduced by 21% (from 53% with EPT to 11% with IMRT).
Other late toxicities were uncommon. We report one case of perinephric fibrosis and pelvico-ureteric junction obstruction, which has not been described previously. Constrictive pericarditis, seen in one patient in this series, is a recognised complication after EPP and is seen both with and without postoperative radiation.19, 22, 23
Our low rate of local recurrence (18%) is consistent with other series of adjuvant hemithoracic radiation treatment. The largest series of 86 patients treated with IMRT reported a 16% recurrence rate within the ipsilateral thorax.17 A recent retrospective case-control series from Switzerland compared highly conformal radiotherapy (IMRT or VMAT) with a conventional 3D conformal technique and reported improved local control with IMRT/VMAT.15
Median survival times following trimodality therapy have ranged from 12.8 to 46.9 months.24 Our median survival of 31 months is similar to that found by Van Schil and colleagues,13 who reported a median survival of 33 months in the subset of patients who completed trimodality therapy. Only one of 38 patients in that study failed to complete radiotherapy. Median DFS and 2-year DFS in our study were 21.6 months and 57.3%, respectively. The Canadian series reported 5-year DFS of 54% in node-negative patients.11 We noted a trend to longer DFS in patients without pathologically involved nodes, with 5-year DFS of 31% versus 18% in the node-negative and node-positive patients, respectively. These data should be considered in the context of a predominantly epithelioid, node-negative population.
The reported survival and recurrence outcomes must be interpreted with caution, given the issue of selection bias in a population selected and referred for adjuvant radiotherapy following EPP. Data from phase II feasibility studies have shown that only 52–65% of patients initially considered for trimodality therapy ultimately complete adjuvant radiation.13, 25 In the Western Australian study, of the 36 patients referred for trimodality therapy, only 14 completed the full course.12 Those that successfully complete radiation treatment then are a highly selected cohort of good performance patients who have failed to progress through multiple lines of treatment. An additional limitation of our study is the likely under-reporting of local recurrences as chest CT was initially not performed routinely, but on development of new symptoms.
Many of our patients (55%) had also received neoadjuvant chemotherapy. Combination chemotherapy with cisplatin and a folate antagonist has been demonstrated to significantly improve survival.26, 27 Cisplatin and pemetrexed have become standard first-line chemotherapy for mesothelioma. We found no difference in any outcome measure between those that received or those that did not receive neoadjuvant chemotherapy.
While local recurrence rates have appeared to improve with radiation treatment when compared with historical controls, recent results from a Swiss Phase II trial (SAKK 1704), published in abstract form, appear to contradict this.28 Median LRFS was 7.6 months without, and 9.4 months with adjuvant radiation, which did not reach significance. There was no difference in OS. Due to slow accrual, the study was closed early with only 54 patients randomised and was therefore underpowered for its primary endpoint of local DFS. In addition, radiotherapy dose and fractionation were not standardised, and radiotherapy details have not yet been reported.
Finally, the optimal surgical approach to localised MPM is also controversial. A randomised, multicentre feasibility study (MARS)29 has suggested EPP may have a survival detriment over no EPP. Criticism of this study has centred on the speculative conclusions drawn from a study primarily investigating the feasibility of randomisation to EPP, as well as the small numbers and higher-than-expected mortality. A retrospective review comparing EPP to pleurectomy/decortication, a procedure with lower morbidity and mortality, found in favour of pleurectomy.30 These findings have led to pleurectomy gaining favour among thoracic surgeons as the preferred surgical technique.
Local failure remains the predominant pattern of relapse following pleurectomy, and efforts are underway to optimally integrate radiotherapy with this surgical technique. Traditionally, radiotherapy following pleurectomy has been associated with inferior local control as a result of the lower doses required to spare the intact lung.31 Recent series have begun to demonstrate the feasibility of hemithoracic radiation in this setting, albeit with rates of pneumonitis consistently around 20%. One series of 36 patients treated with IMRT reported rates of Grade 3 pneumonitis of 20%, including one death.32 A recent series of 20 patients treated with helical tomotherapy following pleurectomy demonstrated a low rate of local recurrence (15%) using doses of 50–60 Gy. Five patients developed Grade 2–3 pneumonitis.33 A prospective trial of post-pleurectomy IMRT is ongoing, with an interim analysis reporting acceptable toxicity.34 With the overwhelming shift in surgical approach away from EPP, our institution has begun to explore hemithoracic IMRT to the post-pleurectomy lung. Nonetheless, we would urge caution with this technique until mature prospective data is available.
Conclusion
Adjuvant hemithoracic radiation treatment following EPP, although associated with significant early toxicity, is reasonably well tolerated. The majority of patients complete the prescribed course of treatment, and clinically significant late toxicities are rare. In patients with right-sided disease, persistent elevations in liver enzymes are common. We have reduced the incidence of subclinical hepatitis via the adoption of IMRT. With meticulous treatment planning and strict dose constraints to the remaining lung, we have seen no cases of radiation pneumonitis.
Our local control and survival outcomes compare favourably with other international series, and we have demonstrated a low local recurrence rate. The predominant pattern of relapse remains distant, highlighting the need for improved systemic therapies to improve the long-term outlook for patients with this rare disease.