A comparative, retrospective analysis of HIV testing among gay, bisexual and other men who have sex with men in Melbourne, Australia
The authors have stated they have no conflict of interest.
Abstract
Objective: PRONTO!, a peer-led rapid HIV-testing service in Melbourne, Australia, opened to improve HIV testing among gay and bisexual men (GBM). We compared client characteristics and return testing among GBM testing at PRONTO! with GBM testing at Melbourne Sexual Health Centre (MSHC).
Methods: All GBM attending PRONTO! and MSHC for HIV testing between August 2013 and April 2016 were included. We describe the number of tests, percentage of clients who returned during follow-up, the mean number of tests and median time between tests at the two services.
Results: At PRONTO!, 33% of 3,102 GBM and at MSHC 50% of 9,836 GBM returned for a further HIV test at least once. The mean number of tests per client was 1.7 and 2.5 at PRONTO! and MSHC (p<0.01), respectively. A majority of clients at both services reported behaviours that would recommend up to quarterly testing, however, the median time between tests was 20.0 and 17.0 weeks at PRONTO! and MSHC (p<0.01), respectively.
Conclusions: A greater proportion of clients returned and returned frequently at MSHC compared to PRONTO!, however, at both services HIV testing frequency was suboptimal.
Implications for public health: Novel HIV testing services should provide convenient and comprehensive sexual health services.
Enhancing HIV testing coverage and frequency is a key component of Australia's response to the HIV epidemic, with testing a priority area for action in the national HIV strategy.1 HIV testing is typically offered in four health service types in Australia: primary care (general practice), tertiary care (hospitals), sexual health centres and, more recently, community-based (non-clinical) HIV testing services. These service types differ in the source of funding (federal, jurisdictional, client co-pay), staffing (medical doctors, nurses, peers) and tests offered (conventional serology, rapid point-of-care (RPOC) tests).2-5 It was not until 2011 that regulatory changes in Australia permitted the use of RPOC tests and testing outside clinical settings.6 These changes resulted in the implementation of new HIV testing models, including trials of RPOC testing services in most Australian jurisdictions.3, 7, 8
PRONTO! is a stand-alone HIV testing service located in an inner suburb of Melbourne, Australia, that is funded by the Victorian Government to offer testing to gay, bisexual and other men who have sex with men (GBM). The model is designed to facilitate frequent testing in line with national testing guidelines.9 To achieve this the service counters a range of testing barriers reported by Australian GBM such as a lack of time, fear of judgement and anxiety waiting for a result.10-12 Service features including operating outside of business hours, an online booking system, testing performed by trained peer staff and immediate results delivery are designed to overcome barriers to HIV testing.
To evaluate the effectiveness of PRONTO! in facilitating HIV testing for GBM and help guide service refinement we compare HIV testing among GBM at PRONTO! and at Melbourne Sexual Heath Centre (MSHC), the largest clinical service provider of HIV testing in Melbourne. Specifically, we compare the characteristics of GBM attending PRONTO! and MSHC for HIV testing, the return HIV testing rates and the characteristics of GBM returning for HIV testing within six months.
Materials and methods
Description of the service models
PRONTO!
The PRONTO! model has been described in detail elsewhere.13 Briefly, PRONTO! is funded by the Victorian government to provide peer-led HIV RPOC tests to GBM in a shop-front service. PRONTO! operates in an inner northern suburb of Melbourne, outside standard business hours (4–8pm weeknights, 10am–2pm Saturday). Opening in August 2013, the PRONTO! model evolved over time, initially providing only HIV RPOC tests. Syphilis RPOC tests were introduced as part of standard practice in June 2014. Comprehensive STI and parallel conventional HIV serology testing was introduced in February 2016. PRONTO! provides free RPOC HIV tests to all clients and free STI testing to those who are Medicare (Australia's publicly funded universal health care system) eligible. SMS reminders to alert clients when they are due for routine HIV testing were also implemented in February 2016.
Melbourne Sexual Health Centre (MSHC)
MSHC is the main publicly funded STI testing service in Victoria and its model of operation has been described in detail elsewhere.14 Briefly, MSHC is located in an inner northern suburb of Melbourne (approximately 3km from PRONTO!) and operates during standard business hours and until 7pm on Thursday. The service almost exclusively operates a walk-in system, with specific GBM clinics available by appointment. MSHC offers conventional HIV serology and comprehensive STI testing in addition to other sexual health clinical services. Triage occurs at reception with consultations managed by doctors and nurses. MSHC is funded by the Victorian Government and provides free HIV and STI testing to all clients. MSHC diagnoses approximately one-fifth of new HIV cases in Victoria.15 MSHC has made evidence-based changes to practice to encourage testing16-18 and utilises SMS reminders, electronic reminders and express services within their standard clinical practice.
Data collection
Data collection at PRONTO!13 and MSHC19 has been described previously. Briefly, all clients attending PRONTO! are invited to complete a behavioural survey in the waiting area prior to each appointment. The survey was updated from paper to an electronic tablet in September 2014. Clients attending MSHC are invited to complete a computer-assisted self-interview (CASI) in the waiting area prior to each visit. Clients returning within three months of their previous visit at MSHC are not invited to complete CASI.19 At the first attendance at each site clients are assigned a unique numerical identifier that facilitates linking test and behavioural data at each appointment and between appointments for clients within each service over time. Surveys at both sites contain sections on demographics, test history and sexual risk behaviour. All PRONTO! sexual risk behaviour questions have a six-month recall whereas MSHC utilise 12-month recall.
Variable creation
Categorical variables derived from the two data sources included age group (16–29, 30–39, 40+ years), Australian born (yes, no) Aboriginal &/or Torres Strait Islander status (yes, no), any HIV testing history (yes, no). Among those with testing history, previous test within the past six months (yes, no) was generated based on a self-report for those with no testing history at the service and also clinic records for those with a previous test at the service.
PRONTO! clients are asked a single question about number of anal sex partners. MSHC clients are asked the number of casual partners (count) and whether they have a current regular partner (yes/no). To derive a single measure of the number of sex partners at MSHC, one partner was added to the casual sex partner count for GBM reporting a current regular sex partner. To account for six-month and 12-month recall periods, the number of sex partners was categorised as none, one, 2–10, 11+ at PRONTO! and none, one, 2–20, 21+ at MSHC.
PRONTO! clients are asked a single question about condom use with casual partners. At MSHC clients are asked about condom use with casual partners separately for insertive or receptive anal sex. For both sites we derived measures of condom use with casual partners as consistent, inconsistent, no anal sex. When MSHC insertive and receptive condom use differed a hierarchy was used; any inconsistent condom use was given highest priority, then consistent and finally no anal sex.
Mean number of tests per individual and median time between tests within each service was calculated based on clinic records.
Analysis
All clients reporting any male-to-male sex ever, testing at each service between 15 August 2013 and 30 April 2016, and aged 16 years and over were included in the analysis. In line with previous return testing analyses,20, 21 tests within 30 days of a previous HIV test were considered a single testing episode and dropped from analyses.
We report the total number of HIV tests and the number of individuals testing for HIV at each service. We also describe demographic, HIV testing history and sexual risk characteristics among GBM using the first behavioural surveillance survey matched to a HIV test record during the reporting period.
For each site, we describe the number of individuals with at least one return HIV test, the mean number of HIV tests per person, the proportion of tests where a follow-up test was conducted within six months (182 days), and the median number of weeks between tests within each service during the reporting period. As HIV-testing frequency guidelines in Australia are risk-based we separately report these return testing outcomes among GBM reporting behaviours categorised as high-risk according to testing guidelines9 (condomless anal sex or greater than 10 anal sex partners in six months at PRONTO! or greater than 20 sex partners in 12 months at MSHC). To estimate six-month return testing we calculated the number of tests between 15 August 2013 and 30 April 2016 with a return test within six months (182 days). The final test for each individual in the last six months of data collection (1 November 2015–30 April 2016) was excluded from the denominator for return testing.
Associations between testing service site and GBM client characteristics were assessed using chi-squared test of proportions for categorical variables and t-tests and Wilcoxon rank sum tests assessed differences in the mean and median for continuous variables, respectively. Temporal trends in six-month return testing were assessed quarterly within each calendar year (index tests assigned to each quarter between 2013 quarter 4 (Q4) and 2015 quarter 3 (Q3)) using a Wilcoxon rank-sum test for trend.
Data were analysed using Stata Statistical Software: Release 14 (StataCorp, TX) and cut-off for statistical significance was p<0.05 for all analyses.
Ethics
This project was approved by the Alfred Health Research Ethics Committee (project number 297/13 and project number 331/16).
Results
Client characteristics
Between 15 August 2013 and 30 April 2017, 4,937 HIV RPOC tests were conducted at PRONTO! among 3,102 GBM compared to 23,938 conventional HIV tests among 10,488 GBM at MSHC. The age and country of birth profiles of GBM testing at PRONTO! and MSHC were similar and few clients reported being Aboriginal and/or Torres Strait Islander. Almost one in five (18%) PRONTO! and MSHC clients reported never previously testing for HIV, and among those with a testing history PRONTO! clients were more likely to report their previous HIV test was less than six months prior (Table 1). While the proportion of GBM reporting high rates of partner turnover (>10 partners in six months at PRONTO! or >20 partners in 12 months at MSHC) were similar, GBM testing at PRONTO! were more likely than those at MSHC to report only one sex partner over the recall period (p<0.01). GBM at PRONTO! were less likely to report recent casual partners and less likely to report condomless sex with these partners compared to those testing at MSHC (p<0.01). Over the reporting period, 43 (0.9%) HIV tests at PRONTO! and 237 (1.0%) HIV tests at MSHC were positive (p=0.43, Table 1).
|
PRONTO! n (%) |
MSHC n (%) |
p-value |
|---|---|---|---|
Number of tests Number of individuals Individuals with matched surveys |
4,937 3,102 3,099 |
23,938 10,488 9,836 |
|
Median age (years, IQR) |
30 (25–37) |
29 (25–36) |
0.51 |
Born in Australia |
1,704 (57.2) |
5,317 (57.1) |
0.85 |
Aboriginal &/or Torres Strait Islander |
60 (2.0) |
79 (0.9) |
<0.01 |
Ever tested for HIV |
2,546 (82.3) |
7,926 (82.3) |
0.98 |
Tested for HIV in previous six monthb |
1,124 (39.0) |
2,556 (26.6) |
<0.01 |
Any sex partner in the past six or 12 monthsc |
2,798 (91.1) |
8,402 (99.0) |
<0.01 |
Number of sex partnersc,d |
|
|
|
One 2–10 PRONTO!, 2–20 MSHC 11+ PRONTO!, 21+ MSHC Any casual partnerc,d Any inconsistent condom use with casual partnersc,e |
601 (21.5) 1,869 (66.8) 328 (11.7) 2,686 (91.7) 1,163 (47.3) |
757 (9.0) 6,926 (82.) 719 (8.6) 8,173 (96.6) 3,558 (51.8) |
<0.01 <0.01 <0.01 |
HIV test result Negative Positive |
4,894 (99.1) 43 (0.9) |
23,701 (99.0) 237 (1.0) |
0.43 |
- Notes: a: Missing responses were excluded: country of birth PRONTO!:122 (3.9) MSHC:518 (5.3%); Aboriginal and/or Torres Strait Islander PRONTO!:50 (1.6), MSHC: 921 (9.4); ever tested for HIV PRONTO!: 4 (0.1), MSHC: 203 (2.1); number of sex partners PRONTO!:29 (0.9), MSHC: 1,352 (13.8); any casual sex partner PRONTO!: 171(5.5), MSHC: 1,374 (14.0); condom use with casual partner PRONTO!:225 (8.4), MSHC:1,308 (16.0). b: Among those reporting ever previously testing for HIV c: Recall period PRONTO! six months, MSHC twelve months d: Among those reporting any sex partner in the previous six or twelve months e: Among those reporting any casual partner in the previous six or twelve months
Return HIV testing
Over the 33-month data collection period approximately one-third of PRONTO! GBM returned for a HIV test compared to approximately half of MSHC GBM and the mean number of tests per individual was lower at PRONTO! compared to MSHC (p<0.01). The frequencies of return testing were more similar between services, however, the proportion of tests at PRONTO! (28%) followed by a return test within six months was still significantly lower compared to MSHC (47%) (p<0.01). Among returning GBM, the median time between tests was 20.0 weeks at PRONTO! and 17.7 weeks at MSHC (p<0.01). Similar return testing patterns were observed when analysis was restricted to clients reporting higher risk for HIV transmission (Table 2).
|
PRONTO n (%) |
MSHC n (%) |
p-value |
|---|---|---|---|
Number of tests |
4,937 |
23,938 |
|
Number of individuals |
3,102 |
10,488 |
|
Number of individuals reporting higher risk |
2,046 |
6,216 |
|
Individuals ever return (15 August 2013–30 April 2016) |
1,024 (33.0) |
5,253 (50.1) |
<0.01 |
Tests with return test within six monthsa |
1,146 (28.1) |
9,216 (46.9) |
<0.01 |
Tests with return test within six month (high risk clients only)a,b |
895 (30.8) |
6,790 (51.5) |
<0.01 |
Median number of weeks between tests (IQR) |
20.0 (12.3–35.0) |
17.7 (11.7–30.4) |
<0.01 |
Median number of weeks between tests (high risk clients only, IQR)b |
20.0 (12.0–35.5) |
17.0 (11.4–29.8) |
<0.01 |
- Notes: a: Among those tests with a return test. Excludes the last test for each client in the last six months of data collection (1 November 2015–30 April 2016) b: high risk includes clients ever reporting any condomless sex or greater than 10 sex partners in six months (PRONTO!) or 20 partners in 12 months (MSHC)
Over the observation period, the number of HIV tests conducted at PRONTO! increased from 251 in Q4 2013 to 527 in Q3 2015, but there was no evidence of an increase in the proportion of GBM re-testing within six months at PRONTO! (Q4 2013:24.7%, Q3 2015:26.8%, p=0.78). At MSHC, the number of HIV tests conducted increased from 1,784 in Q4 2013 to 2,477 in Q3 2015, with a significant increase in the proportion re-testing within six months at MSHC (Q4 2013: 42.9%, Q3 2015:48.1% p<0.01, Figure 1).
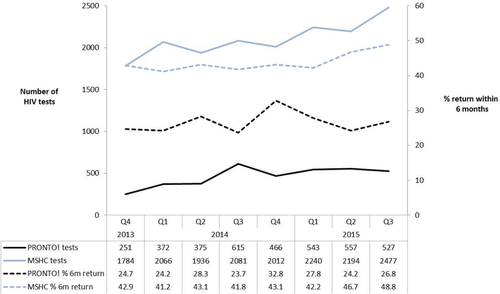
Proportion of tests with a return test within six months (182 days) by calendar year quarter at PRONTO! and MSHC, 1 October 2013–31 September 2015.
Discussion
While there is extensive literature reporting on the acceptability and uptake of testing at peer-led22-24 and RPOC25-28 testing services, to our knowledge, this is the first paper to report comparative testing frequencies between this model of testing and to other more conventional testing services. While the PRONTO! model demonstrated high service acceptability,29 and was designed to overcome many barriers to testing reported by Australian GBM,10-12 test frequency remained suboptimal with significantly fewer PRONTO! clients ever returning and the median time between tests two weeks longer at PRONTO! compared to MSHC.
The only previous assessment of the impact of RPOC testing on HIV test frequency in a developed country was conducted at MSHC, and there are no published comparisons of peer-led and non-peer-led RPOC testing services. The RPOC trial at MSHC showed that an initial increase in testing frequency among participants receiving RPOC testing was not sustained,30 ultimately contributing to the decision to not implement RPOC testing at that site. The limited impact of RPOC testing in this setting may relate to a lack of perceived benefit relative to conventional testing that was offered at the same site, with previously reported barriers to testing, such as waiting times and difficulties finding and attending clinic appointments, consistent across both RPOC and conventional testing. While PRONTO! may have attenuated some of these barriers, we have previously shown that the absence of STI testing at the service created a barrier to returning, some clients reporting returning to testing for HIV at other services after their first test at PRONTO!.31 The lack of STI testing at PRONTO! likely contributed to the difference in the proportion of GBM returning for a HIV test at PRONTO! compared with MSHC. STI testing was implemented as standard practice in February 2016 and an ongoing evaluation will determine if there was a shift in repeat testing following this service-level change.
While some GBM may have elected not to return to PRONTO! at all due to the lack of STI testing, previous surveys of clients also indicated ongoing HIV testing at PRONTO! alongside intermittent HIV testing elsewhere.31 Intermittent testing at PRONTO! may relate to a variety of factors. PRONTO! clients may have initially tested due to curiosity associated with a peer-led RPOC testing that was novel in the local setting and initial and intermittent testing may also relate convenience associated with opening times and appointment availability. Additionally, the peer-led and rapid-result delivery may have been especially attractive to clients testing following a specific risk event; in the first 12 months, 27% of PRONTO! clients reported a recent risk event as their reason to test.13 This may have been especially appealing with well-established clinics such as MSHC being at or near capacity, resulting in long wait times for walk-in clinics and delays in obtaining appointments at appointment-based services.
Other factors at MSHC may have contributed to higher return-testing rates. A significantly greater proportion of GBM attending MSHC reported specific HIV risk behaviours, and the greater proportion reporting either no or only one recent sex partner may have influenced return testing following risk-related counselling during testing. There is also strong evidence that SMS reminders, used to alert clients when they are due for routine HIV/STI test at MSHC throughout the study period but not introduced at PRONTO! until February 2016, increased HIV and STI testing frequency.32 The implementation of an express clinic for asymptomatic GBM clients in 201518 may have also positively impacted return HIV testing at MSHC. These innovations may have contributed to the increasing trend in return testing seen at MSHC that was not observed at PRONTO!.
There are limitations in this study. First, individuals' repeat tests could only be linked within each service and not between services, resulting in a likely underestimate of testing frequency. Repeat testing data at PRONTO! may have been particularly susceptible to this limitation given clients' need to access multiple services for comprehensive STI testing. Second, the impact of the introduction of STI testing in February 2016 at PRONTO! on return HIV testing was not measured in this study. Analyses that specifically explore the impact of this change are underway. Third, survey questions and data collection methods differed between the two sites and these differences are most pronounced in behavioural indicators of sexual risk. In particular, MSHC clients returning within three months are not invited to complete another behavioural survey by the CASI system, and recall and partner definition differs between the sites. While efforts were made to harmonise variables, these differences may have impacted comparisons of client characteristics.
PRONTO!, a peer-led RPOC testing service was designed to reduce barriers to frequent testing reported by Australian GBM. When compared to the largest sexual health clinic in Victoria, PRONTO! clients returned less frequently for HIV testing, although six-monthly return testing at both sites was sub-optimal. While the introduction of STI testing and SMS reminders at PRONTO! in early 2016 may contribute to increased return testing and will be the focus of ongoing monitoring of return testing rates, our findings also suggest a need for innovations to encourage GBM at risk of HIV to test frequently. The recent approval of a HIV self-test by the Australian Therapeutic Goods Administration33 may provide an opportunity to encourage more frequent testing among GBM and may be particularly appealing to clients familiar with RPOC technologies used in self-testing devices.
Funding
The Victorian Department of Health and Human Services funds the evaluation of PRONTO! and ongoing surveillance projects within the Burnet Institute.