Evaluation of Neutrophil Activity Before and After Granulocyte and Monocyte Adsorptive Apheresis in Patients With Pustular Psoriasis
Funding: This work was supported by Hamamatsu Photonics K.K. (Grant FLP-H4200b).
ABSTRACT
Introduction
Activated neutrophils play a crucial role in the development of neutrophilic dermatoses, including pustular psoriasis. Adsorptive granulocyte and monocyte apheresis (GMA) is an effective treatment for skin disorders. Although previous basic research has demonstrated neutrophil activation, no efficient method exists to assess it in clinical settings.
Methods
We measured neutrophil activity in patients with GPP who underwent GMA therapy using the FLP-H4200, a newly developed neutrophil activity evaluation system. Blood samples were collected before the first and after the fifth GMA session.
Results
In Case 1, which responded to GMA, the neutrophil activation value decreased from 118 603 to 26 234, reaching the normal range. In Case 2, the response to GMA was poor, and the neutrophil activation value decreased from 140 623 to 76 780, which remained significantly above the normal level.
Conclusion
These results suggest that the neutrophil activity evaluation system may be useful for assessing disease severity and therapeutic efficacy.
1 Introduction
Generalized pustular psoriasis (GPP), a clinical phenotype of psoriasis, is characterized by the sudden appearance of generalized sterile pustules and fever lasting several days [1]. It can potentially lead to life-threatening complications, such as capillary leak syndrome, necessitating appropriate treatment to prevent such developments. Treatments for GPP include oral medications such as etretinate, cyclosporine, and methotrexate, as well as biologics targeting TNFα, IL-17, IL-23, and IL-36 signaling [2]. Adsorptive granulocyte and monocyte apheresis (GMA), a non-pharmacological intervention that selectively removes activated granulocytes and monocytes, is another treatment option for GPP. Clinical trials have shown that GMA is effective for GPP, and the results indicated that activated myeloid lineage leukocytes are major pathological factors in the disease [3].
When neutrophils are activated, they migrate, generate reactive oxygen species (ROS), form neutrophil extracellular traps, and secrete mediators [4]. This neutrophil activation process has been elucidated well in basic research, and the development of an efficient method to assess the neutrophil activation state in clinical settings has been highly sought after. It has been reported that ROS are produced excessively in psoriasis and that ROS production is reduced by treatment [5, 6]. In this study, we assessed neutrophil activation by measuring ROS generation and investigated whether it could be used to evaluate skin symptoms. Although neutrophils are involved in the pathology of pustular psoriasis, the severity of pustular psoriasis is only reflected by the white blood cell count. As GMA is a treatment that removes granulocytes and monocytes, we hypothesized that it would be possible to evaluate neutrophil activation and its association with disease activity more precisely in patients with GPP. We used the FLP-H4200, a newly developed neutrophil activity evaluation system, to assess neutrophil activity in patients with GPP who underwent GMA therapy [7]. Neutrophil activity is evaluated based on the production level of hypochlorite ions (OCl−) by neutrophils, which is known to increase in activated neutrophils [8]. The FLP-H4200 [7] is an improved version of FLP-H3200 [9], a popular model developed for the medical market as an inexpensive and simple tool for measuring only OCl−, as opposed to CFL-H2200 [7-11], a model developed for researchers that enables them to simultaneously monitor O2 −· and OCl− over time. The fluorescence sensitivity of FLP-H4200 is higher than that of FLP-H3200 because of approximately threefold excitation light intensity [7]. The secondary metabolite OCl− is more strongly associated with inflammation than the primary metabolite O2 −, helping reflect more subtle changes in the physical condition [7, 8, 10-12].
In this study, we measured neutrophil activity before and after GMA treatment using a newly developed neutrophil activity evaluation system [7] and assessed its relationship with disease severity.
2 Methods
2.1 Patients
Neutrophil activity was measured in two patients with GPP treated with GMA. GMA was performed five times at seven-day intervals. Blood samples were collected before the first and after the fifth GMA session. By GMA, blood is dialyzed using an Adacolumn at a flow rate of 30 mL/min for 60 min. An 18-gauge dialysis needle was inserted into the cubital vein to remove blood, and another 18-gauge venous needle was inserted into the opposite cubital vein to return blood. Nafamostat mesylate was administered as an anticoagulant, at 0.5 mg/kg/h during apheresis. The GPP severity score was used to determine disease severity [3]. The total GPP severity score ranged from 0 to 17 points, which can be categorized as follows: < 6, mild; 7–10, moderate; and 11–17, severe. In the subscoring system [3], the extent (percent of total body surface area) of erythroderma, pustules on an erythematous background, and edema is given a score of 0–9 points with 3 points (maximum) each reflecting ≥ 75% erythroderma, ≥ 50% erythema with pustules, or ≥ 50% edema, whereas 0 indicates normal-appearing skin. Other relevant variables, including body temperature, white blood cell counts, serum albumin (ALB), and the inflammation marker C-reactive protein (CRP), were scored from 0 to 7. Thus, a maximum score of 2 points was assigned as follows [3]: body temperature ≥ 38.5°C = 2, white blood cell count ≥ 15 000/L = 2, CRP ≥ 7 mg/dL = 2, and ALB < 3 g/dL = 2. A score of 0 was assigned for body temperature < 38.5°C, white blood cell count < 10.000/μL, CRP < 0.3 mg/dL, and ALB ≥ 3.8 g/dL. Informed consent was obtained from all the participants before the initiation of the study. The study protocol was approved by the Institutional Ethics Committee of Kagoshima University Hospital (No. 220036).
2.2 Reagents
Phorbol 12-myristate 13-acetate (PMA) and dimethyl sulfoxide (DMSO) were purchased from Sigma-Aldrich (Tokyo, Japan). The fluorescent reagent aminophenyl fluorescein (APF) was purchased from GORYO Chemical Inc. (Sapporo, Japan). PMA (0.1 mM) was dissolved in DMSO and stored at −80°C as a PMA stock solution. The solution was diluted to a ratio of 1:20 (v/v) with Ringer's-4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES) buffer (154 mM NaCl, 5.6 mM KCl, and 10 mM HEPES, pH 7.4) immediately prior to its use [8].
2.3 Measurement of Neutrophil Activities
The production of hypochlorite ions (OCl−) from stimulated white blood cells was measured using blood samples as previously described [7]. Briefly, 3 μL of whole blood was incubated in a reaction mixture containing APF on a dedicated fluidic chip. Subsequently, fluorescence (FL)-OCl− levels were monitored for 1500 s using FLP-H4200, which is manufactured at Hamamatsu Photonics K.K., Hamamatsu, Japan [7]. The samples were then stimulated with PMA for 150 s. The increased fluorescence signal after PMA stimulation was calculated using dedicated original analysis software [13] and used as an evaluation value [7].
3 Results
3.1 Case 1
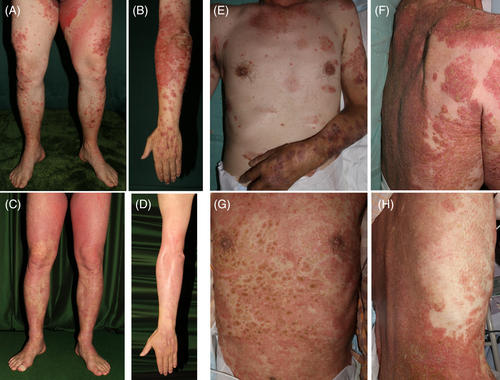
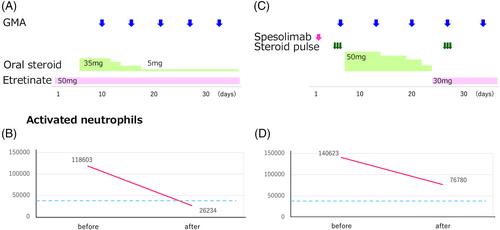
A 49-year-old Japanese man who had been diagnosed with psoriasis several years earlier and treated with topical medications visited our department with high fever and pustules that appeared 10 days prior. During the initial examination, erythematous plaques and pustules were observed on his trunk and extremities, with a high fever of > 39°C (Figure 1A,B). Histopathological examination revealed the presence of subcorneal and Kogoj spongiform pustules. His white blood cell count was 19 930/μL, serum albumin level decreased to 2.6 g/dL, and C-reactive protein (CRP) level was elevated to 31.14 mg/dL (Table 1). A diagnosis of GPP was made, and GMA was administered in combination with etretinate 50 mg and oral prednisolone (Figure 2A). Following the initiation of GMA therapy, the prednisolone dosage was gradually decreased as the patient's symptoms improved. After undergoing GMA, the pustules disappeared, and the skin symptoms improved (Figure 1C,D). The GPP severity score was 13 prior to GMA, improving to 4 following GMA (Table 1). The skin score improved from 5 to 3, his body temperature fluctuated from 36°C to 39.5°C, and all his blood test findings improved. Neutrophil activity (118 603 prior to GMA treatment) decreased to 26 234 following GMA treatment (Figure 2B).
| Before | After | |
|---|---|---|
| Severity score | 13 | 4 |
| Skin score | 5 | 2 |
| Body temperature (°C) | 39.5 | 36.9 |
| WBC (/μL) | 19 930 | 6260 |
| Neutrophils (/μL) | 16642 | 3310 |
| CRP (mg/dL) | 31.14 | 0.35 |
| Albumin (g/dL) | 2.6 | 3.6 |
| Neutrophil activity | 118 603 | 26 234 |
| Neutrophil activity/neutrophils | 7.13 | 7.92 |
3.2 Case 2
A 71-year-old Japanese man who had skin symptoms on his entire body and had been receiving topical medications for psoriasis for 4 months visited our department because of a fever and the appearance of pustules 6 days prior to his first visit. Edematous and erythematous plaques were present on his entire body, along with pustules and crusts. He had a high fever (> 39°C) (Figure 1E,F). Histopathological examination revealed the presence of Kogoj spongiform pustules. The white blood cell count was 19 000/μL, serum albumin level was 2.7 g/dL, and the CRP level was 6.88 mg/dL (Table 2). Based on these findings, GPP was diagnosed. Despite the administration of spesolimab, the patient's symptoms worsened. Steroid pulse therapy was initiated, followed by oral prednisolone (SL) (Figure 2C). GMA was initiated immediately after the pulse therapy. Oral PSL was tapered off and etretinate was introduced because his symptoms improved. However, the pustules relapsed after the discontinuation of PSL, and steroid pulse therapy was repeated. Despite repeated pulse therapy, the erythematous area expanded, and the pustules persisted (Figure 1G,H). The severity score of pustular psoriasis remained moderate at 10 before and 9 after the GMA (Table 2). Neutrophil activity decreased from 140 623 before the start of treatment to 76 780, after which it remained elevated (Figure 2D).
| Before | After | |
|---|---|---|
| Severity score | 10 | 9 |
| Skin score | 4 | 4 |
| Body temperature (°C) | 37.8 | 38.7 |
| WBC (/μL) | 19550 | 8750 |
| Neutrophils (/μL) | 18810 | 7350 |
| CRP (mg/dL) | 6.88 | 1.67 |
| Albumin (g/dL) | 2.7 | 2.0 |
| Neutrophil activity | 140 623 | 76 780 |
| Neutrophil activity/neutrophils | 7.19 | 10.45 |
4 Discussion
In this study, we measured neutrophil activity in patients with GPP who underwent GMA therapy using the FLP-H4200. We established a reference range and reported an upper limit of 10 630 OCl− values in healthy adult males, based on a large clinical study involving 2677 volunteers using the FLP-H3200 [9]. The upper limit for adult males using the FLP-H4200 was determined by calculating the correlation coefficient (y = 2.9027x + 5616) between the FLP-H4200 and the FLP-H3200, yielding a value of 36500 [7]. In Case 1, GMA was found to be effective, and the neutrophil activation value decreased from 118 603 to 26 234, eventually reaching the normal range. In Case 2, the response to GMA was poor, with neutrophil activation decreasing from 140 623 to 76 780, which remained significantly above the normal level. These results indicated that neutrophil activity reflects the disease severity and therapeutic effectiveness of GMA.
Oxidative stress is an important factor in neutrophil-driven inflammation. Stimulated neutrophils activate their NADPH oxidase to generate large amounts of superoxide, which acts as a precursor to hydrogen peroxide and other ROS that are generated by their heme enzyme myeloperoxidase (MPO) [14]. The development of psoriasis is associated with the overproduction of ROS, which activate immune cells and keratinocytes, as well as modulate various signaling pathways within those cells [5]. IL36RN was identified as a gene responsible for the development of GPP in 2011 [15]. Since then, a growing number of genetic mutations, including CARD14, AP1S3, MPO, and the SERPIN family, have been identified as causative genes of GPP. These genes are involved in the activation of neutrophils. The association between MPO deficiency and pustular skin disease was first recognized by Vergnano et al. with phenome-wide association studies [16]. In vitro functional studies showed that mutations in the MPO gene lead to increased neutrophil accumulation and activity [17]. Neutrophil counts are commonly used to measure inflammation, including in GPP. However, the diversity of the genetic background of GPP suggests that neutrophil counts alone may not directly reflect the severity of the disease. Our previous reports also showed that the neutrophil count did not demonstrate the whole picture of oxidative stress [8, 12]. In Case 2, although neutrophil activity was reduced by almost half, the value obtained by dividing neutrophil activity by neutrophil count increased (Table 2). It is speculated that, although neutrophil count decreased, the neutrophils remained activated. While neutrophil count alone cannot fully reflect the pathological condition, measuring neutrophil activity allows for a more objective assessment. By measuring OCl− production, we can evaluate treatment effectiveness and determine whether to continue GMA or switch to another treatment. Discontinuing ineffective treatment is also meaningful from a healthcare economics perspective.
The mechanisms underlying GMA have been investigated extensively. GMA not only removes activated neutrophils and monocytes but also induces functional changes to leukocytes that pass through the column, resulting in the inhibition of neutrophil activity [18].
In previous clinical trials of GMA for pustular psoriasis [3], clinical efficacy was evaluated for 2 weeks post-treatment. In this study, we evaluated neutrophil activation immediately after the fifth GMA session considering the short lifespan of neutrophils. Future studies are needed to determine the optimal timing for assessing neutrophil activation.
In the present study, changes in white blood cell and neutrophil counts were similar in both cases. In contrast, the rate of decrease in neutrophil activity differed between groups, indicating the presence of pathologically activated neutrophils. Based on these observations, we propose that evaluation of neutrophil activity is useful for assessing disease activity and treatment efficacy.
Ethics Statement
The study protocol was approved by the Institutional Ethics Committee of Kagoshima University Hospital.
Conflicts of Interest
Kimiko Kazumura: Employee of Hamamatsu Photonics K.K.