Pathology testing in non-trauma patients presenting to the emergency department with recurrent seizures
Abstract
Objective
Excessive pathology testing is associated with ED congestion, increased healthcare costs and adverse patient health outcomes. This study aimed to determine the frequency, yield and influence of pathology tests among patients presenting to the ED with atraumatic recurrent seizures.
Methods
This was a retrospective cohort study conducted at a level 4 adult ED in Australia and included atraumatic patients presenting to ED with recurrent seizures over a 4-year period (2017–2020). The primary outcome was the frequency of pathology tests. Additionally, the proportion of abnormal pathology test results and the association between pathology tests and change in management were assessed.
Results
Of the 398 eligible presentations, 346 (86.9%, 95% confidence interval [CI] 83.3–89.9%) underwent at least one pathology test. In total 18.3% (n = 517) of pathology tests had an abnormal result which led to 15 changes in ED management among 12 presentations. Patients who had an abnormal pathology test result were more likely to undergo a change in antiepileptic drug management (odds ratio 2.08, 95% CI 1.23–3.65; P = 0.008).
Conclusion
Most patients presenting to the ED with atraumatic recurrent seizures underwent pathology tests. Abnormalities were frequently detected but were uncommonly associated with change in management. Abnormal pathology test results were associated with changes in antiepileptic drug management although rarely led to acute changes in patient management. This study suggests that pathology tests may be excessively requested in this population.
Key findings
- Of patients presenting to the ED with recurrent seizures, 86.9% underwent at least one pathology test.
- In total, pathology tests were abnormal in 18.3% of cases and led to 15 changes in patient management.
- Patients with abnormal pathology testing were more likely to undergo a change in antiepileptic drug management.
Introduction
Seizures are a common presentation among ED patients, accounting for approximately 1% of all ED visits.1 The majority of these patients have a known seizure history and have previously undergone extensive diagnostic workup.2, 3
On presentation to the ED, patients with recurrent seizures may undergo extensive pathology testing of unknown utility. Laboratory test results may identify seizure precipitants, diagnose underlying seizure pathology and inform patient management.4 However, unnecessary testing is associated with ED congestion, healthcare costs and anxiety for patients with needle phobias.5-8
Current seizure guidelines do not address the role of repeat pathology tests in atraumatic recurrent seizure patients presenting to the ED.9-12 A recent systematic review concluded that only one previous study has assessed the yield of blood tests in this population.13 In this study, electrolyte levels were abnormal in 19% of presentations and glucose levels were elevated in 50% of cases.14 No previous study had reported on the incidence or influence of pathology investigations on patient management for this population.13
The aim of this study was to determine the frequency, yield and influence of pathology tests in non-trauma patients presenting to the ED with recurrent seizures. Additionally, we sought to determine the association between pathology tests and change in management, particularly a change to antiepileptic drugs (AEDs). We hypothesised that pathology tests would be commonly requested in this population, but rarely influence patient management.
Methods
Study design and setting
We conducted a retrospective cohort study at a level 4 adult ED with an annual census of approximately 70 000 patients. By definition, this ED has access to a wide range of sub-specialty services and is capable of managing complex conditions.15 It is also the state referral centre for trauma, burns, adult cardio-thoracic transplantation, cystic fibrosis and HIV medicine. This study adhered to the Strengthening the Reporting of Observational Studies in Epidemiology guidelines.16 Ethics approval for this study was obtained from The Alfred Hospital's Human Research & Ethics Committee (Project No. 255/21). The requirement to seek informed consent from patients was waived.
Selection of participants
Patients who presented to the ED between 1 January 2017 and 31 December 2020, and were assigned a primary diagnosis of ‘seizure’ or ‘epilepsy’ on triage-free text were eligible for inclusion. They were excluded if they presented with acute traumatic brain injury (TBI), status epilepticus or a first-time seizure. Patients with significant concurrent illness that would have necessitated pathology testing independent to the seizure presentation were also excluded, as were those who self-discharged, refused investigations or were transferred from another hospital.
Data extraction
Two authors (MB and SS) manually performed an explicit chart review on all eligible patients and extracted demographic information (age and sex), seizure type, AED history, focal neurological deficits on physical examination and past medical history. Past medical conditions of particular interest included stroke, brain cancer, systemic cancer, acquired brain injury and TBI. The suspected precipitant for the seizure was also extracted.
Investigations assessed included full blood examination (FBE) (including white cell count [WCC]), urea electrolytes and creatinine (UEC) levels (including sodium [Na], potassium [K], corrected calcium [Co Ca], magnesium [Mg], phosphate [PO4], estimated glomerular filtration rate [eGFR]), blood sugar levels (BSLs), liver function test (LFT) results and alcohol (ETOH) levels.17 In this study, each of these specific investigations was reported as a distinct test (i.e. a patient who underwent a WCC, Na, K, PO4 and eGFR was recorded as having five separate investigations). The aim of this approach was to optimise generalisability, because different hospitals may include varying combinations of pathology investigations within a single ‘test’.
Only investigations performed during the ED episode of care were collected. In all cases, this was within 24 h of presentation to the ED. The frequency and yield of AED levels were also collected. All investigation results were reported as categorical variables with pathology reference levels used to define normal and abnormal pathology results (Table 1). The chronic kidney disease stages were used to classify eGFR results.18 Results were further classified into acute or chronic abnormalities, when patient's pathology abnormalities were documented as chronic.
| Investigation | Number requested (%) | Normal reference range | Result | n (%) | Mx change (n)† |
|---|---|---|---|---|---|
| Full blood examination | |||||
| WCC (×109/L) | 340 (85.4) | 3.90–12.70 | Low | 12 (3.5) | 0 |
| Normal | 293 (86.2) | 0 | |||
| High | 35 (10.3) | 2 | |||
| UEC levels | |||||
| Na (mmol/L) | 344 (86.4) | 135–145 | Low | 35 (10.2) | 0 |
| Normal | 307 (89.2) | 0 | |||
| High | 2 (0.6) | 0 | |||
| K (mmol/L) | 341 (85.7) | 3.5–5.2 | Low | 24 (7.0) | 4 |
| Normal | 312 (91.5) | 0 | |||
| High | 0 (0) | ||||
| Coagulated | 4 (1.2) | 0 | |||
| Ca (cor.) (mmol/L) | 206 (51.8) | 2.1–2.6 | Low | 6 (2.9) | 0 |
| Normal | 199 (96.6) | 0 | |||
| High | 1 (0.5) | 0 | |||
| Mg (mmol/L) | 279 (70.1) | 0.7–1.1 | Low | 16 (5.7) | 2 |
| Normal | 261 (93.5) | 0 | |||
| High | 2 (0.7) | 0 | |||
| PO4 (mmol/L) | 275 (69.1) | 3.5–7.7 | Low | 83 (30.2) | 3 |
| Normal | 191 (69.5) | 0 | |||
| High | 1 (0.4) | 0 | |||
| eGFR (mL/min/1.73 m2) | 342 (85.9) | Stage 1: >90 | Normal | 247 (72.2) | 0 |
| Stage 2: 60–89 | Mild impairment | 79 (23.1) | 0 | ||
| Stage 3a: 45–59 | Moderate impairment (3a) | 10 (2.9) | 0 | ||
| Stage 3b: 30–44 | Moderate impairment (3b) | 4 (1.2) | 0 | ||
| Stage 4: 15–29 | Severe impairment | 2 (0.6) | 1 | ||
| Stage 5: <29 | End-stage renal failure | 0 (0) | |||
| Blood sugar level (mmol/L) | 322 (81.0) | 3.5–7.7 | Low | 0 (0) | |
| Normal | 295 (91.6) | 0 | |||
| High | 27 (8.4) | 0 | |||
| Liver function test | 243 (61.2) | Normal | 130 (53.5) | 0 | |
| Total protein (g/L) | 60–80 | Abnormal | 113 (46.5) | 1 | |
| Albumin (g/L) | 33–46 | ||||
| Bilirubin (mcmol/L) | ≤21 | ||||
| ALT (units/L) | ≤40 | ||||
| GGT (units/L) | ≤62 | ||||
| ALP (units/L) | 30–110 | ||||
| AED levels (mcmol/L) | 98 (24.6) | Valproate: 350–700 | Low | 50 (51.0) | 13 |
| Carbamazepine: 17–51 | Normal | 41 (42.0) | 9 | ||
| Lamotrigine: 12–55 | High | 6 (6.1) | 2 | ||
| Phenytoin: 40–80 | Unsuitable | 1 (1.0) | 0 | ||
| ETOH levels (mmol/L) | 46 (11.6) | ≤2 | Normal | 38 (82.6) | 1 |
| High | 8 (17.4) | 0 | |||
- † Mx change refers to number of patients with a test result who subsequently underwent a change in management and does not reflect the number of unique management changes that were performed. In some cases, multiple changes of management occurred following a test result while in others one change of management occurred following two abnormal test results. While 14 test results were associated with a management change, there were a total of 15 management changes across 12 unique patients.
- AED, antiepileptic drug; ALP, alkaline phosphatase; ALT, alanine transaminase; Ca (cor.), corrected calcium; ETOH, alcohol; GGT, gamma-glutamyl transferase; K, potassium; Mg, magnesium; Mx, management; Na, sodium; PO, phosphate; WCC, white cell count.
Investigations were considered to influence patient management when abnormal investigation findings led to a change in patient management in the ED. A change in patient management was defined as an intervention in the ED that was a direct result of an abnormal investigation. A change in acute management included changes in disposition (i.e. hospitalisation), medical management (e.g. treatment for electrolyte abnormality, or change in AED type or dose), referral (i.e. emergency referral) and further diagnostic assessment.
Outcome measures
The primary outcome assessed was the frequency of pathology tests performed. Secondary outcomes were the proportion of abnormal pathology tests and the proportion of patients who had their management changed as a result of pathology results.
Data analysis
Continuous variables were reported using means and standard deviations (SDs) and compared using the Student's t-test. Categorical variables were reported using proportions and compared using χ2-tests. Associations with a P-value <0.05 were considered statistically significant. Univariable logistic regression was performed to determine the clinical variables associated with pathology test frequency and abnormalities. Additionally, multivariable analysis was performed to assess the clinical variables associated with changes in acute management. Statistical analysis was performed using R and R Studio® (Version 1.4.1106, Boston, MA, USA).
Results
Of the 4365 records screened, 398 visits related to 313 unique patients met the pre-specified inclusion criteria. The most common reasons for exclusion were a non-seizure presentation (1052 patients), a first seizure presentation (529 patients) and a concurrent head trauma presentation (448 patients). A summary of the patient selection process is presented in Figure 1.
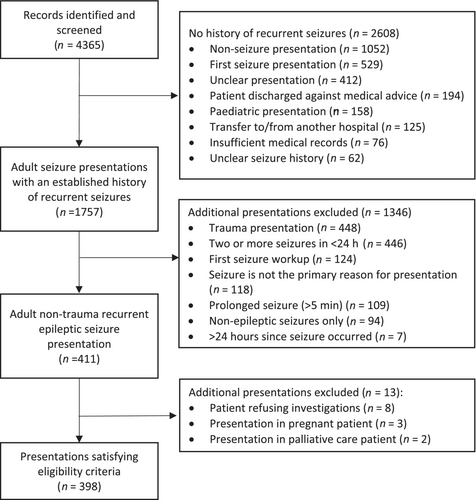
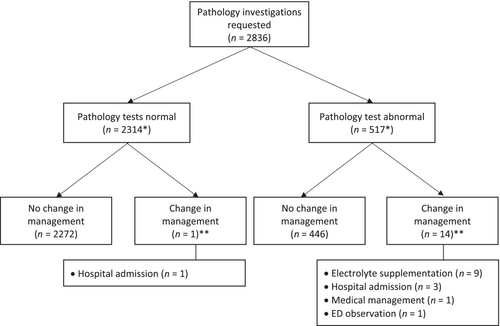
Of the 313 eligible patients, 172 were male (55.0%) and 141 (45.0%) were female. The mean age of the study cohort at the time of ED presentation was 40.9 years (SD 19.0, range 18–94). The baseline characteristics of this cohort are presented in Table 2. A summary of the study outcomes is presented in Figure 2.
| Characteristic | Total (n = 398) |
|---|---|
| Age, mean (SD)† | 40.9 (19.0) |
| Sex, n (%)† | |
| Male | 172 (55.0) |
| Female | 141 (45.0) |
| Seizure type, n (%) | |
| Generalised seizure | 216 (54.3) |
| Focal seizure | 18 (4.5) |
| Unknown seizure | 164 (41.2) |
| Potential precipitant, n (%)‡ | |
| AED non-compliance | 79 (19.8) |
| Sleep deprivation/stress | 77 (19.3) |
| Alcohol or drug use§ | 68 (17.1) |
| Cancer progression | 5 (1.3) |
| Possible infection | 4 (1.0) |
| Hypoglycaemia | 2 (0.5) |
| Other | 22 (5.5) |
| Unknown/not documented | 178 (44.7) |
| AED prescription, n (%)¶ | 318 (79.9) |
| Medical history, n (%) | |
| Brain cancer | 34 (8.5) |
| Systemic cancer†† | 4 (1.0) |
| Stroke | 29 (7.3) |
| TBI | 16 (4.0) |
| ABI | 9 (2.3) |
- † Age and sex statistics have been calculated for the 313 unique patients involved in this study.
- ‡ In 29 cases, two potential precipitants were identified; in four additional cases, three potential precipitants were identified.
- § Alcohol and drug use precipitants included alcohol exposure in 37 cases, drug use in 25 cases and alcohol withdrawal in 14 cases.
- ¶ This figure includes patients not currently compliant with medication.
- †† In this study, systemic cancer history does not include patients with secondary brain metastasis.
- ABI, acquired brain injury; AED, antiepileptic drug; SD, standard deviation; TBI, traumatic brain injury.
Frequency of pathology tests
In total, 346 of the 398 (86.9%, 95% confidence interval [CI] 83.3–89.9%) ED encounters underwent at least one pathology blood test. Of these, Na (86.4%), eGFR (85.9%), K (85.7%), WCC (85.4%) and BSL (81.0%) were most frequently requested. AED levels were requested in 98 cases (24.6%). Additionally, AED prescription history was associated with a reduction in requests for all pathology tests except AED levels. The frequency and yield of pathology tests are presented in greater detail in Table 1.
Yield of pathology tests
Among the 2836 pathology investigations requested, four yielded a coagulated result, and one did not return a result. Of the remaining investigations 18.3% (517/2831) had an abnormal result. This included 57.7% (56/97) of AED levels, 46.5% (113/243) of LFTs, 13.8% (37/340) of WCCs, 11.8% (170/1445) of electrolyte levels and 8.4% (27/322) of BSLs.
Association of pathology tests and change in management
Pathology test results were associated with 15 changes in ED management across 12 unique patient presentations (Table 1). Of these, one change of management occurred following a normal alcohol level. These changes of management included electrolyte supplementation (n = 9), hospital admission (n = 4), medical management (n = 1) and extended ED observation (n = 1).
WCC results led to a change of management for two patients, both of whom had leucocytosis. One patient was given antibiotics and admitted for workup of a fever of unknown origin. The other patient was observed in the emergency short stay unit and was subsequently discharged home without further management changes.
Eight patients received electrolyte supplementation following UEC studies. This included four cases of hypokalaemia, three cases of hypophosphataemia and two cases of hypomagnesaemia with one of these patients having two electrolyte abnormalities. Three of these patients also had additional investigation abnormalities, including renal function impairment, alcohol withdrawal and leucocytosis, as well as a history or examination finding of clinical relevance and were admitted to hospital. There were no cases where sodium, corrected calcium, hyperkalaemia, hypermagnesemia or hyperphosphataemia results led to a change of management. While eGFR results were abnormal in 27.8% of cases, this test led to a change in management in only one patient. This patient had an eGFR of 28 and an electrolyte abnormality and was admitted to hospital.
LFTs resulted in a change in management in one instance for a patient with a high gamma-glutamyl transferase level and who was found to have a pre-existing, untreated HIV diagnosis on further history taking. This patient was admitted to hospital.
In one case, a normal alcohol level influenced patient management for a patient suspected of having an alcohol withdrawal seizure. Following this result, this patient was admitted to hospital and received IV diazepam. While 13 other patients were suspected of having alcohol withdrawal seizures, alcohol investigations did not lead to a change in management in these cases. Elevated alcohol levels influenced patient management in zero cases.
In the ED setting, there were no cases where BSL results led to a change in patient management. Two patients in this study presented with hypoglycaemia as the suspected precipitant of their seizure. In both, patients underwent BSL testing during ambulance transfer to the ED and received glucose supplementation from paramedics. Neither patient underwent further management in the ED.
AED management was changed in 24 (24.5%) of the 98 patients who underwent AED level testing and 63 (21.0%) of the 300 cases where AED levels were not measured (Table 3). Patients whose AED levels were measured were not more likely to receive a change in AED management compared to those who did not have AED levels measured (odds ratio [OR] 1.22, 95% CI 0.71–2.09; P = 0.47). Patients who had an abnormal pathology test result were significantly more likely to undergo a change in AED management (OR 2.08, 95% CI 1.23–3.65; P = 0.008).
| Clinicodemographic variable | OR (95% CI) | P-value | aOR (95% CI) | P-value |
|---|---|---|---|---|
| Age | 1.01 (0.98–1.04)† | 0.529 | 1.01 (0.98–1.04) | 0.427 |
| Male sex | 2.33 (0.68–10.64) | 0.211 | 1.92 (0.50–7.43) | 0.344 |
| AED prescription | 0.18 (0.05–0.59) | 0.0047 | 0.20 (0.06–0.65) | 0.007 |
- † OR relates to a 1-year incremental increase in age. Bold values have been used to highlight relationships of statistical significance P-value < 0.05.
- In instances where one value of the contingency table was zero, a univariable analysis could not be performed. This was the case for variables ‘focal neurological deficit’, ‘brain cancer history’, ‘other cancer history’, ‘stroke history’, ‘TBI history’ and ‘ABI history’.
- ABI, acquired brain injury; AED, antiepileptic drug; aOR, adjusted odds ratio; CI, confidence interval; OR, odds ratio; TBI, traumatic brain injury.
The influence of clinical and demographic factors on changes in management after pathology investigations was considered (Table 3). Among patients who underwent a pathology test, those with an AED prescription history were significantly less likely to undergo an acute change in management. Age and sex were not associated with statistically significant differences in changes in management following pathology testing.
Discussion
Among patients presenting with atraumatic recurrent seizures to the ED, pathology tests were requested in 86.9% of cases and 18.3% of these results were abnormal. These high rates of abnormalities support one prior study on this topic that examined a limited selection of pathology tests. Sever et al. reported that 17% of patients presenting with recurrent seizures had hyponatraemia, 2% had hypernatraemia and 50% had high blood sugar readings.14 These results were higher than our study findings which is likely because Sever et al. only examined patients who also underwent a computed tomography of the brain (CTB) scans and these patients were therefore more likely to be acutely unwell compared to our cohort.
Sever et al. also reported that AED levels were requested in 27.5% of patients using AEDs, which was similar to our study (30.2% of patients using AEDs). AED levels do not appear to be high yield. Patients who underwent AED testing were not more likely to undergo a change in AED management compared to those who did not undergo AED level testing. Instead, abnormalities in other pathology test results guided changes in AED management. These results support current evidence and suggest that routine reflexive AED testing should be avoided in epilepsy patients.19 In patients presenting with recurrent seizures, AED levels should instead only be performed if clinically indicated (e.g. to monitor the effectiveness of new medication and to test for AED compliance).
Three clinical variables – age, brain cancer history and stroke history – were associated with higher pathology test abnormalities in our study (Appendix S1). This finding is unsurprising and is unlikely to be of meaningful value in determining which patients may derive benefit from pathology testing. Age is likely associated with pathology test abnormalities given the higher rates of disease that occur in older patients. Additionally, brain cancer history and stroke history are more common in older patients and likely reflect poor overall patient health. This may explain the apparent association between these variables and BSL and eGFR abnormalities.
A key finding from our study is that pathology tests appear to be frequently requested and abnormal but have minimal influence on ED management. Only 14 patients underwent a non-AED change in management as a consequence of pathology tests. While nine patients received electrolyte replacement it is unlikely that this management had significant implications on patient outcome. In the four cases where patients were admitted to hospital following FBEs, UECs or alcohol testing, three patients had multiple pathology abnormalities, and all four patients had significant history or examination findings that necessitated further investigation and management.
Similarly, LFT results were frequently abnormal (46.5%) in our study but only resulted in a change in management for one patient who also had historical findings of significance. Elevation in liver biomarkers is common among patients receiving AEDs and rarely represents a finding of clinical significance in the otherwise asymptomatic patient. Although AED prescription history was associated with a reduction in pathology testing for all studies (except AED levels), the majority of patients who underwent pathology tests had an AED prescription history. It is therefore possible that a large proportion of abnormalities in LFTs and other pathology tests in this study is the result of AED prescriptions rather than new underlying pathology.19
Phosphate levels were also frequently abnormal with 30.2% of those tested yielding a low phosphate result. Among patients presenting with a reported generalised seizure and who underwent phosphate testing, 36.6% (53/145) yielded a low phosphate result. These results support existing literature that suggests that hypophosphatemia is frequently observed in patients presenting to the ED with generalised seizures and may represent a potential biomarker for these patients.20 The broader clinical significance of detecting a low phosphate remains unclear.
The high rates of seemingly low-yield pathology test requests in this study may be the consequence of ED clinicians practicing a reflexive approach to recurrent seizure management and ordering a ‘baseline’ panel of blood tests. A meta-analysis found that within hospitals, pathology tests are inappropriately ordered in 20% of cases.21 In the ED, this rate may be as high as 63%.22 Excessive testing may also represent clinician uncertainty and a fear of missing a life-threatening diagnosis. Recurrent seizures may be precipitated by lethal metabolic, neurological and nephrogenic condition.19 It is possible that a clinician's concern of these diseases together with the absence of diagnostic guidance on this topic may contribute to excessive pathology requests.23
Excessive investigations can result in worse patient health outcomes. ED pathology tests can increase a patient's ED length of stay (LOS) by up to 72.5 min which can lead to ED crowding, delays in treatment and increased mortality rates.6, 24 The accumulation of seemingly inexpensive blood tests can also contribute a significant economic burden to the healthcare system while causing severe anxiety for patients with needle phobias.8
Our results mirror research on first seizure patients and suggest that basic blood tests, including FBEs, UECs, BSLs and LFTs are of low yield in recurrent seizure patients and are not necessary in otherwise well-recurrent seizure presentations.19, 25-27 We recommend that pathology testing should not be routinely performed in atraumatic recurrent seizure patients in the emergency setting and instead be guided by clinical gestalt and patient history and examination.
Research investigating outcomes from the Choosing Wisely campaign has shown that excessive investigations can be reduced through developing clinical decision-making pathways, redesigning electronic medical records and through audits and feedback to clinicians.28-30 In our study population, these aforementioned strategies as well as clinician education and using electronic records to screen for and alert patterns of reflexive blood test requesting may offer a strategy for reducing unnecessary blood tests. We recommend that future research validate our study findings with a prospective study and consider testing the utility of these strategies (e.g. a diagnostic guidance tool) in this population.
To the authors' knowledge, no prior studies have comprehensively assessed the utility of pathology tests in this population and these results may have important implications on how clinicians investigate this population.
Limitations
This study may be limited by selection bias as only patients with a discharge diagnosis of seizures or the term ‘seizure’ in triage notes were screened for eligibility in this study. While a comprehensive search of free text was conducted, it is possible that not all recurrent seizure patients were initially identified for the screening process. However, it is unlikely that missing patients would have had different clinical characteristics and management.
Additionally, the retrospective nature of this study made the interpretation, of data difficult. As this study relied on information previously documented by clinicians in the medical record it was not always possible to determine which investigation abnormality led to a change in management. This was the case for the three patients who were admitted to hospital with multiple investigation abnormalities. Analysis involving these presentations was therefore interpreted with caution.
This study also had a limited sample size (n = 398). As a consequence of our limited sample size, some clinical variables associated with high yields of investigation abnormalities may have poor statistical power. Additionally, it is possible that the generalisability of our study results may be limited as this study was conducted at a single level 4 ED although we believe that this limitation is likely mitigated by the standardisation of ED training across Australia.
Conclusion
A substantial proportion of atraumatic recurrent seizure presentations to the ED underwent pathology tests and results were frequently abnormal although rarely resulted in changes in patient management. This study is the first of its kind to comprehensively assess pathology tests in this population and suggests that pathology tests may be excessively requested in this population. We recommend that clinicians rely on patient history and examination findings in conjunction with clinical gestalt when deciding on which investigations to request for this population.
Acknowledgement
Open access publishing facilitated by Monash University, as part of the Wiley - Monash University agreement via the Council of Australian University Librarians.
Author contributions
MB was responsible for study concept and design; acquiring, interpretation and analysis of data; and drafting the manuscript. SS was responsible for acquiring data. RM contributed to drafting and revising the manuscript. BM conceived the study design and was responsible for drafting/revision of the manuscript for content in statistical analysis and revision of the manuscript.
Competing interests
BM is a section editor for Emergency Medicine Australasia.
Open Research
Data availability statement
Data available on request from the authors.