The Evolution of Mortality Inequality in 11 OECD Countries: Introduction*
Submitted February 2021.
We gratefully acknowledge the support of the ESRC Centre for the Microeconomic Analysis of Public Policy (ES/T014334/1). We thank the authors of all of the papers in this special issue.
I. Introduction
Long life is considered fortunate in every culture, so inequalities in mortality are fundamental to the way we think about whether a society is equitable. Many prominent recent studies argue that although most countries have seen dramatic declines in mortality through the decades, the gains have not been distributed equally.1 Indeed, several studies argue that when measured across educational groups and/or geographic areas, not only are mortality gaps widening, but also overall life expectancy is even falling, at least for some US groups.2 Given that the number of years that an individual can expect to live is such an important indicator of welfare, inequality in mortality is an important dimension in which overall societal inequality may be increasing.
Although inequalities in mortality are a subject of intrinsic interest that are often reflected in media headlines, they are not easy to measure in a consistent way over time or across countries. Currie and Schwandt (2016a) proposed an approach to examining inequalities in mortality that allowed all of the deaths for an entire population to be included (e.g. not only adults with income or education data). They build on a tradition of describing inequality by geographic areas.3 Their method remedies one of the problems in that literature, which is that differential migration can bias comparisons across areas. Also, it allows comparisons of changing distributions over time and across countries. The importance of health inequalities associated with places has recently been underlined by Chetty et al. (2016).
The approach is conceptually simple. First, rank areas from richest to poorest and then group them into 20 ‘bins’ of approximately equal size. The grouping of areas into bins helps to account for migration by ensuring that the analyst is always comparing population groups of fixed size. Age-specific mortality rates can then be examined by age and gender group for each bin in any chosen year for which data are available (e.g. from a census). This procedure allows a consistent comparison of death rates in, for example, counties representing the poorest 5 per cent (or 10 or 20 per cent) of the population with those representing the richest five (or 10 or 20) per cent of the population across years.
The papers in this special issue use this approach to provide a comparison of the evolution of geographic inequalities in mortality in Canada, Czech Republic, Finland, France, Germany, the Netherlands, Norway, Portugal, Spain, the United Kingdom and the United States. As affluent Western democracies, currently these countries all enjoy certain commonalities, and yet their experiences over the past 30 years have been quite diverse in terms of the evolution of both income and health inequalities. In part, this diversity represents the disparate impacts of larger historical forces, such as the fall of communism and global recessions, and in part it reflects different policy choices, such as the construction of the welfare state in Scandinavian countries and the continuing lack of universal health insurance in the US. It is precisely these different histories and differing policy institutions that make international comparisons a potentially fruitful avenue for understanding phenomena such as mortality rates or life expectancy, which depend on risk factors over the entire lifetime of the individuals concerned.4
Each paper of this issue applies the approach of Currie and Schwandt (2016a) to mortality data from around 1990 to around 2018, depending on data availability. We asked each set of authors, when preparing the papers, to begin with a strictly comparable methodology, enabling comparison across the papers. Hence, each paper first carries out an analysis of inequalities in mortality for men and women in six broad age ranges: 0–4, 5–19, 20–49, 50–64, 65–79 and 80+. The authors then delve further into interesting developments within their own countries, motivated by the data they have available and the most relevant policy or institutional context. Several papers (Czech Republic, the Netherlands, Portugal, Spain and the UK) examine trends in avoidable (treatable and preventable) deaths; some focus on specific causes of death, including deaths of despair, external injuries, cancer and infant mortality (Finland, Germany and Norway), and others discuss the impact of the 2008 financial crisis and its aftermath (Finland, Portugal and Spain).
The comparison across countries allows us to draw several broad conclusions. First, although the discussion of trends in the US often dominates academic journals, the US is an outlier. None of the other countries showed increases in age-specific mortality rates for any group. Instead, they saw continuing declines in mortality, though at different rates during different time periods.
Second, while it can be difficult to juggle a mental focus on inequality with an awareness of what is happening to levels of mortality, it is essential to keep the two in mind. There are some instances in which greater equality is the result of a deteriorating health advantage for one group rather than an improvement in health for the disadvantaged group (i.e. levelling down as opposed to levelling up). For example, in most countries, men started with much higher mortality rates than women in 1990, and that gap has narrowed over time. However, in some countries (Spain and the Netherlands) the narrowing gap among older cohorts is partly a result of increases in deaths from preventable causes for women, which may in turn be due to increases in smoking and inadequate access to cancer care.
Third, and perhaps most importantly, these papers demonstrate that there is no mechanical relationship between income inequality and health inequality. Kitigawa and Hauser (1973), and many subsequent papers, have shown that lower socio-economic status is associated with higher mortality, but the relationship varies tremendously over time and across countries. Some countries have virtually eliminated, or even reversed, geographic inequalities in mortality. And while Spain and Portugal were both hard hit by the recession following the financial crisis of 2008, Spain continued to see declining mortality and declining inequality in mortality, while in Portugal inequality in mortality increased.
The rest of this introduction proceeds as follows. After providing a short overview of some of the literature about inequality in mortality and its measurement, we discuss some specifics of the way the analyses were conducted that are common across the papers. We then provide further comments on the lessons to be drawn overall.
II. Measuring inequality in mortality
There is a large body of literature measuring inequality in mortality by educational attainment.5 However, using education as a measure of changes in socio-economic status over time is problematic because median levels of educational attainment have changed dramatically over time.6 For example, in the US, the share of white, non-Hispanic women aged 25–84 with less than a high school education fell 66 per cent between 1990 and 2010. These days, a high school dropout is more likely to be poor and to have underlying health conditions than a high school dropout in earlier decades, which complicates efforts to compare mortality rates by educational groups over time.7 Similarly, dramatic shifts in educational attainment have occurred in all of the countries represented in this special issue. Even if the educational shifts have not occurred in recent history, they will still distort comparisons made across different cohorts or age groups in recent years. Another difficulty is that completed educational attainment is only available for adults above a certain age. Hence, this method does not lend itself to a consideration of trends for children. Yet, if one wants to forecast future population health, indicators of the health of children are especially important.
A second strategy involves examining mortality inequality by relative income levels.8 As income is not reported on death certificates in the US, these efforts in the US have typically used survey data. Longitudinal ageing studies, such as the Health and Retirement Study (HRS) in the US, the English Longitudinal Study of Ageing (ELSA) and the Survey of Health, Ageing and Retirement in Europe (SHARE), include detailed data on income and also link to mortality outcomes. However, these data sets are quite small and, by design, include only older age cohorts. For example, the National Research Council (2015) uses HRS data with a sample that includes 5,740 deaths. These data limitations mean that strong assumptions are required to estimate and project trends in life expectancy.
Relatively few surveys include both income and mortality information. Some authors have attempted to circumvent the data issues by using administrative data, such as tax returns linked to death certificates9 or public pension data.10 While these data bases have rich information about the people who are captured, those with incomplete work histories are less well represented and those without work histories, such as children, are absent. These data limitations are not an issue in Scandinavian countries with full registry data, such as Norway, and the analysis for Norway in this issue exploits such data to consider the extent to which within-area inequalities in mortality remain, even after inequalities between areas have been eliminated.
A third strategy, and the one we pursue here, is to examine inequality by geographical areas, such as counties. Analyses based on geographic areas are potentially subject to bias due to selective migration. If, for example, the most healthy and able-bodied people tend to leave lower-income counties over time and migrate to higher-income counties, we might expect to see mortality increase in the poor counties and decrease in the rich counties, even if in fact each individual's health remains exactly the same. For example, Wang et al. (2013) find that female life expectancy decreased by 2.68 years in US counties with the sharpest declines in life expectancy between 1985 and 2010, while it increased by 6.16 years in the counties with the largest gains in life expectancy. However, over this period, the population fell by 6 per cent in the counties with the largest mortality increases, while the population grew by an average of 101 per cent in the counties with the biggest improvements in life expectancy, suggesting that these gains were driven by in-migration of healthy people.11
Using US tax data, Chetty et al. (2016) categorise individuals by both income and location.12 They first examine mortality by percentiles of the income distribution for each age from 40 to 76. Their preferred specification uses income from two years ago in order to reduce the chance that their results are driven by reverse causality from health to income inequality. They calculate survival curves and extrapolate them to age 90. Then, they calculate life expectancy at age 40 for each quartile of the income distribution, in different locations. They conclude that ‘low-income individuals live longest in affluent cities with more educated people and higher local government expenditures…’. These results suggest that some features of location boost health at least as much among the poor as among the rich.
Hence, Chetty et al. (2016) suggest an additional reason that we should be interested in the analysis of inequalities in mortality across geographical areas: there may be features of particular areas (e.g. air pollution) that affect everyone living in a particular location. Amenities such as green space and hospitals are better in rich areas and the poor cannot be completely excluded from enjoying these benefits. Similarly, using data on the elderly, Deryugina and Molitor (2020) show that among the generally poor people displaced from New Orleans by Hurricane Katrina, those who went to areas with higher longevity had longer life spans. It will be important for future work to determine which sorts of amenities are most responsible for reducing mortality among the poor in wealthy areas.
III. A few methodological issues
There are a number of issues to be considered in applying the approach of Currie and Schwandt (2016a). First, why focus on age-specific mortality rates rather than a summary measure of life expectancy? Although life expectancy sounds like a measure of the number of years that a person can expect to live, it is not. Suppose we are interested in the life expectancy of the cohort that is currently 20 years old. Life expectancy is computed using the assumption that when this cohort reaches age 40, it can expect to live the same number of years as the cohort that is currently 40 years old. It is easy to see that if age-specific mortality rates are changing over time, then this assumption will be false. Only in a world where mortality rates are static does life expectancy mean what most people think that it does. If, in fact, mortality rates are changing over time, then it makes much more sense to study age-specific mortality rates when examining trends.
A second problem is that poverty, which is used to rank areas, is measured quite differently in different places. The US, for example, uses a measure originally based on the cost of a ‘thrifty food basket’, which is updated over time, whereas many European countries use a poverty standard that is relative to the median income. In some countries, poverty measures are not available at a fine geographic level. In this special issue, the authors have used the prevailing poverty measure of their country (however it is defined) when available, but if it is not available, then they have used a deprivation index that captures levels of unemployment, low educational attainment and substandard housing.13
Another consideration is that although the same broad areas of countries tend to be the poorest over long periods, it is possible for small areas to move around in the distribution from one year to the next. In order to consistently compare the poorest areas with the richest areas, it is necessary to take possible rank-switching into account by re-ranking in each year.
There may also be changes in the age structure within age groups. That is, in a broad age grouping such as adults aged 20–49, a group that has more individuals aged 20 will tend to have lower mortality than one that includes more individuals aged 49. In order to account for changes in the age structure within age groups, mortality rates are age-adjusted using the composition in one particular year as a baseline.14 For example, if 1990 was the baseline, then the age-specific mortality rates in 2000 and 2010 would be applied to the 1990 population, which effectively keeps the age composition within broader age groups constant over time. It also ensures that any changes measured are resulting from changing mortality not from changing population structure.
Finally, the level of geographical aggregation can also matter, certainly for the level of inequality and perhaps also for trends. The papers on Norway and the UK both show that inequality is higher at lower levels of aggregation, as would be expected if the poorest large areas are still heterogeneous in terms of the poverty and deprivation of the smaller areas within them. To the extent possible, we have attempted to align the level of aggregation across the papers. However, the degree to which this is possible is limited by data availability and variation in how countries are organised. Each paper specifies the size of the population in the areas used in the analysis.
In the papers that consider preventable and treatable causes of death, this distinction is based on a list of causes of death published by the Organization for Economic Development and Cooperation (OECD)/Eurostat (2019). Unlike previous lists, this list has the advantage that most causes of death are assigned to one list or the other. In cases where the death is considered both preventable and treatable, 50 per cent of deaths were assigned to each list. The specific lists are shown in Table A.1 in the online Appendix. Formally, the OECD does not classify deaths over 74 years as preventable or treatable, so readers should keep this caveat in mind when examining breakdowns for the age group 80+.
IV. Discussion
The papers in this special issue all provide valuable information on trends in mortality and mortality inequalities in each country assessed on an individual country basis. Because the data in each paper are comparable, however, the papers can also provide insights when assessed in comparison with each other. As an illustration of the potential power and interest of cross-country comparative statistics, we briefly highlight some key findings that emerge when comparing this set of papers for three of the age groups: 0–4, 25–49 and 65–79.
Figure 1 brings together data for each of these age groups from nine European countries, taken from the first part of each of the eight single country papers in this special issue, as well as the paper by Baker et al. (2021) with updates on estimates for the US, Canada and France.15 The top two plots for each age group show the mortality rate (per 1,000) separately for men and women for each of the years included in the country analysis. The bottom two plots show the socio-economic inequality in mortality in each of those years; that is, the coefficient of the fitted regression line in the main figure in Part A of each country paper, which shows mortality across areas ranked by deprivation ventile.
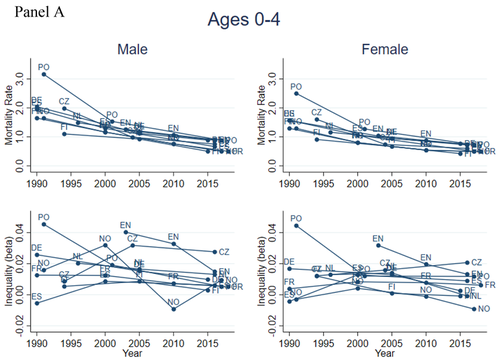
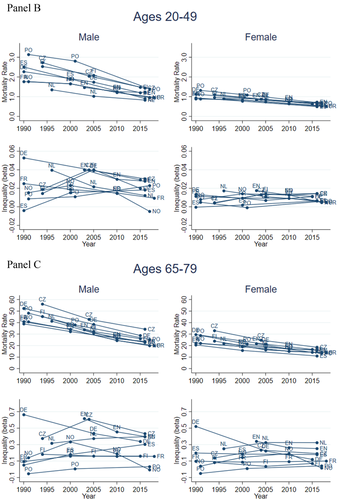
A number of themes emerge from Panels A–C of Figure 1, which can be borne in mind when reading the narratives in each individual country paper. First, the trends in the levels of mortality rates are much more systematic across countries than trends in inequalities. Mortality has improved for all three age groups, with considerable convergence across European countries for the 0–4 and 20–49 age groups. This convergence is driven by the countries with the highest initial mortality rates – the Czech Republic, Portugal and Spain – which have all improved quite rapidly. Improvements for men in these two age groups have also been greater than for women, reducing gender inequalities.
While there has also been improvement in mortality rates for the older 65–79 age group, this improvement has not been accompanied by convergence either across countries or across genders. Indeed, the country trends in mortality rates for these older age groups have been remarkably parallel.
The discussions of the trends in each country in the papers of this special issue encompass issues such as health care policy changes for the 0–4 age group, the impacts of economic recessions over the period on the 20–49 age group, and also trends in different causes of death within this middle-aged adult group.
Comparison of the bottom panels of Figures 1A–C shows that the story with regard to inequalities in mortality is much more mixed: both levels and trends in inequality over the period are heterogeneous. In general, inequalities are higher for men than for women, and more different across countries, although this is less the case by the end of the period for the two adult age groups presented here. Looking at the two older age groups shows that, for both men and women, inequalities are actually rising for some countries and falling for others. The result is some convergence, albeit still with considerable international heterogeneity.
The resurgence of interest in inequality in mortality has followed growing public discussion about income inequality. The two types of inequality are often linked in the media, and many academics have argued for a causal connection between the two.16 However, this association between socio-economic status and mortality does not mean that these move in lock step. In fact, given that much of the recent increase in economic inequality is at the very top of the income distribution, it is not clear why it should have any causal impact on deaths in other groups, except through the impact of inequality on the political process. That is, those at the top of the income distribution may lose interest in paying taxes to provide public services if they can opt into privately provided services of higher quality.
The idea that increases in income inequality generally lead to rising inequality in mortality has been vigorously disputed in the literature. Gravelle (1998) argues that places with higher income inequality also tend to have more poverty, and that poverty rather than income inequality drives higher mortality rates. Deaton and Paxson (2001) have shown that the relationship between trends in income inequality and trends in mortality actually moved in the opposite direction over most of the 20th century, with mortality falling rapidly in several periods when income inequality rose. Many of these declines in mortality were driven by advances in public health, such as the provision of clean water, universal vaccination programmes and the development of cheap and effective drugs such as antibiotics. All of these developments represented policy choices to support improvements in public health.
Smith (1999, 2005, 2007) argues that when socio-economic status and health do move together, it may be health that causes income differences among adults rather than the reverse. In their reanalysis of the famous Whitehall studies of British civil servants, Case and Paxson (2011) show that poor childhood health (proxied by adult height) causes lower job ranks in adulthood, rather than vice versa. This result may reflect the continuation of health trajectories that are established early in childhood.17 It is important to keep in mind that some mortality differentials between adults, summarised in Figures 1B and 1C, may have their roots in events decades ago.
Perhaps we should not be surprised then that trends in inequality in mortality have evolved so differently both within countries over time and across countries, as the policy environment differs tremendously within and across countries, particularly with regard to health care.
One area where there is suggestive evidence in these papers relates to the organisation and extent of the welfare states established after World War II, especially regarding differences in the provision of health insurance and the financing of health care systems, which may be among the most important policy differences. Most of the European countries have established quite extensive welfare states including publicly funded social insurance and health care systems. The Scandinavian model is a ‘cradle-to-grave’ version of a publicly funded, universal welfare state including progressive taxation, universal health care, generous day care and parental leave policies, free college, and strong labour market institutions. As an outlier on the other side is the US, where most social insurance programmes are not universal but means-tested.
One takeaway from the country studies included in this special issue, evident from Figure 1, is that the two Nordic countries, Finland and Norway, with extensive welfare states including publicly funded and universal health care, have seen strong improvements in health in general. By the 2000s, health inequalities across regions ranked by poverty level had disappeared for most age groups. Moreover, as shown in Butikofer et al. (2021) for Norway, the reduction in health inequality as measured by infant deaths in the richest and poorest municipalities took place at the same time as publicly funded infant health care centres were rolled out across Norway in the 1960s. As the authors also show, this does not necessarily mean that the socio-economic gradient in health immediately disappears within regions, as there may still be a within-area difference in the take-up of the services, the adoption of new technologies, etc.
Another indication that the publicly funded health care system is important in explaining economic gradients in health mortality is the finding in Banks et al. (2021) that most of the reduction in mortality rates by age in the UK took place in the first decade of the second millennium when the UK health system was well funded. In the aftermath of the 2008 financial crisis and a reduction in funding, less progress in reducing inequality was observed.
Within the US, there are large differences across age groups in how well covered individuals are by the health system. For instance, the two groups that continued to see mortality declines in the US are those who are most comprehensively covered by public health insurance: the old and the very young. Also, the US opioid crisis has been fuelled by a medical system that created certain incentives to prescribe, along with few controls on providers.
In contrast to the important effects of policy, it is unlikely that differences in health behaviours such as smoking, drinking, unhealthy eating or obesity can explain the trends in the cross-country differences that we see. In an earlier comparison, Banks et al. (2006) show that British citizens have lower morbidity than Americans, even though they tend to smoke and drink more and are almost equally likely to be overweight. Looking at the evidence in this special issue, it seems unlikely that differences in health behaviours across countries (some pairs of which are very similar, such as Portugal and Spain or Finland and Norway) or trends in such health behaviours can explain the large heterogeneity in the levels and trends of mortality inequalities.
Some of the differences between cohorts within countries in cancer deaths may possibly be explained by things such as historical differences in smoking patterns, because past smoking can have long-term negative consequences even among people who have not smoked for many years. But health behaviours are also shaped by public policy. Declining smoking rates in the US reflect many years of multi-pronged efforts ranging from higher cigarette taxes, to public service announcements, to bans on smoking in workplaces and public spaces. Note also the finding in Butikofer et al. (2021) of a reduction in low weight births potentially explained by a reduction in maternal smoking during pregnancy.
Finally, we should note that the studies in this special issue delineate trends in mortality rates and inequality in mortality that were in effect before the COVID-19 pandemic. In countries such as the US and the UK, the COVID-19 pandemic has brought inequalities in mortality rates into even sharper focus, as disadvantaged groups have been disproportionately affected. This reality underlines the importance of documenting these inequalities and how they have evolved over time, thus setting any subsequent trends related to COVID-19 in an appropriate historical perspective. Such basic information is key to identifying vulnerable areas and will allow us to understand whether the pandemic has fundamentally changed geographic inequalities in mortality. We predict that underlying drivers of inequality in mortality will reassert themselves after the pandemic and that countries with lower levels of investment in public health will continue to see a much stronger relationship between socio-economic status and health than those that are committed to health equity.
References
- 1 See, for example, Murray et al. (2006), Cutler et al. (2011), Olshansky et al. (2012), Wang et al. (2013), National Research Council (2015), Case and Deaton (2015, 2017) and Chetty et al. (2016).
- 2 Murray et al., 2006; Olshansky et al., 2012; Wang et al., 2013.
- 3 Murray et al., 2006; Singh and Siahpush, 2006; Kulkarni et al., 2011; Wilmoth, Boe and Barbieri, 2011; Wang et al., 2013.
- 4 See Banks and Smith (2012).
- 5 See, for example, Mackenbach et al. (2016).
- 6 Bound et al., 2014; Dowd and Hamoudi, 2014; Hendi, 2015; Goldring, Lange and Richards-Shubik, 2016.
- 7 Some other studies that examine mortality by education groups include Pappas et al. (1993), Preston and Elo (1995), Elo and Preston (1996), Meara, Richards and Cutler (2008), Montez and Zajacova (2013) and Montez and Berkman (2014). Bound et al. (2014) address the issue by categorising education in terms of relative rank in the overall distribution and by focusing on the bottom quartile of the education distribution. Unlike some of the other studies, they find no evidence that survival probabilities declined in the bottom quartile of the education distribution.
- 8 Pappas et al., 1993; Mellor and Milyo, 2002; Waldron, 2007, 2013; Bosworth and Burke, 2014; Pijoan-Mas and Rios-Rull, 2014; National Research Council, 2015.
- 9 See, for example, Chetty et al. (2016) for the US.
- 10 See Milligan and Schirle (2021) for Canada.
- 11 See Table A2 in the online Appendix of Currie and Schwandt (2016b) for these calculations.
- 12 A limitation of the approach taken by Chetty et al. is that income is not observed for non-earners.
- 13 Note that even if the education distribution is changing over time as discussed above, one can still rank areas from lowest to highest average educational attainment.
- 14 The baseline varies across papers. For example, the papers on the Czech Republic, Norway and the UK use the last year of the analysis, while the paper for the Netherlands uses the first year of the analysis.
- 15 Given our focus on Europe, we do not include data for the US and Canada in this figure.
- 16 Marmot et al., 1991; Wilkinson, 1996; Lynch et al., 2004.
- 17 Currie and Almond, 2011.




