Diagnostic spectrum and therapeutic efficiency in teledermatology–Results of the largest cohort study to date
Abstract
Timely and comprehensive dermatological care is a major challenge. Digitized medical consultation offers a possibility to overcome this problem. Here, we studied the diagnostic spectrum and treatment success in teledermatology in the largest cohort to date. Over 12 months, 21 725 individuals received a diagnosis and therapeutic advice using the asynchronous image-text method. In the context of quality management, 1802 individuals (~10%) of both sexes with a mean age of 33.7 years (SD 15.36) received a follow-up 3 months after the initial consultation to assess the treatment outcome. Of these, 81.2% did not require a face-to-face consultation. Therapeutic efficiency could be ascertained in 83.3% of the patients, whereas 10.9% did not improve, and 5.8% did not provide an information on the course of therapy. Teledermatology is a useful tool in digitalized medicine and complements the classical in-person dermatological examination, as shown by the high degree of treatment efficacy in this study. Although face-to-face consultations can not and should not be completely substituted by teledermatology it reflects a significant contribution to patient care and justifies the further expansion of digital structures in dermatological care.
1 INTRODUCTION
Dermatological care is characterized by average waiting times for an appointment of about 4.9 weeks. In this context, teledermatology offers a solution to provide patients with fast and readily accessible care using a digital approach.1
In teledermatology, the communication between patient and physician can take place either synchronously (live interactive video conference) or asynchronously using the store-and-forward (SAF) technology, based on clinical pictures and electronic case files, which are usually uploaded via an app.1
Despite the increasing use of teledermatology, particularly since the onset of the COVID19 pandemic, there are only a few studies on its preciseness and treatment efficacy.2 Moreover, the majority of studies have mostly focused on one dermatological diagnosis only and/or a relatively small number of patients.3, 4
Here, we sought to evaluate via a standardized follow-up consultation in the context of quality assessment the diagnostic spectrum and therapeutic efficiency of teledermatology in the largest cohort with varied dermatological diseases studied to date.
2 METHODS
From October 10, 2020 to November 01, 2021, 21 725 individuals with a skin disease received a diagnosis and a therapeutic advice within 24 h via a certified teledermatology app provider (Dermanostic, inc.; https://dermanostic.com). The teledermatological consultation could be requested either by downloading an app from the Google Play Store/Apple App Store or by using the WebApp directly in the browser (no download necessary). Based on a standardized protocol and the SAF method, each patient submitted three clinical pictures and answered a short questionnaire (Table 1). In ambiguous instances, the app provider free of charge offered the further evaluation of such inconclusive cases by an expert panel consisting of three board-certified dermatologists with at least 30 years of professional experience.5
| Teledermatological consultation questionnaire | |
|---|---|
| 1 | How can we help you? |
| 2 | When did the skin condition appear? |
| 3 | Do you feel any itching? |
| 4 | Do you feel pain? |
| 5 | Where is the skin condition located? |
| 6 | Do you have any pets? |
| 7 | Do you have known allergies? |
| 8 | Are you aware of any pre-existing conditions? |
| 9 | Have you taken any medications in the last 2 weeks? |
| 10 | Have you had sexual intercourse in the last 3 weeks? |
| 11 | What is your occupation? |
| 12 | What is your biological gender? |
| 13 | Are you pregnant/could you be pregnant or are you breastfeeding? |
For quality management, the app provider also continuously conducted a random follow-up of 10% of the patients, which was performed over the phone by trained study nurses using a standardized questionnaire (Table 2). All individuals in this study provided informed consent, in accordance with the ethical principles of the Declaration of Helsinki. The aims of the follow-up interview were: (i) to inquire if the treatment recommendations have been followed, (ii) to find out if there was an improvement of the condition, (iii) to ask if the patient has seen another physician for an additional face-to face (FTF) examination in the meantime, and (iv) to check whether the diagnosis could be confirmed, if the latter was the case.
| Follow-up questionnaire | |
|---|---|
| 1 | Have you adhered to the treatment recommendation? |
| 2 | Has the skin condition improved? |
| 3 | Have you seen a physician face-to-face after the initial teledermatological consultation? |
| 4 | If so, has the physician confirmed the teledermatological diagnosis? |
| 5 | Optional: Do you need a follow-up prescription? |
3 RESULTS
A total of 1802 (8.3%) patients received a follow-up consultation. The average time from initial patient-contact to follow-up was 90.3 days. Due to technical difficulties, poor imaging or incomplete documentation, 71 (3.9%) cases were excluded. Eventually, a complete data set for evaluation was available for 1731 (96.1%) patients, comprising 1004 (58%) males and 727 (42%) females. 61% of the subjects were aged between 20 and 40 years (mean 33.7 years, SD 15.36) (data not shown).
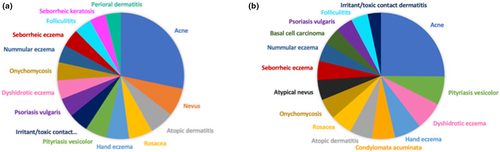
The overall diagnostic spectrum in the initial study population (n = 21 725) included436different dermatological diseases, of which the 15 most frequent ones are depicted in Figure 1a. In contrast, the spectrum of dermatological disorders in the follow-up cohort comprised 213 distinct diagnoses, of which the 15 most common are specified in Figure 1b.
Seven hundred and twenty two (41.7%) patients received a topical therapy, 334 (19.3%) patients a combined topical and systematic treatment, 25 (1.4%) patients a systemic therapy solely, and 335 (19.4%) patients other forms of therapy, e.g. hygiene and/or behavioral recommendations. Moreover, 315 (18.2%) patients received a combination of the aforementioned therapies.
The random follow-up could be evaluated in 1731 individuals. Of these, 1370 (79.1%) patients adhered to the therapy prescribed, whereas 171 (9.9%) individuals did not. In 190 (11%) cases, no specific therapy was required. In 1141 (83.3%) patients, treatment led to an improvement, whereas 149 (10.9%) did not observe a therapeutic effect. 80 (5.8%) of the patients did not provide information on the therapeutic outcome.
Based on the initial teledermatological advice, 1405 (81.2%) patients did not require an additional FTF consultation, whereas 289 (16.7%) patients were advised to seek an immediate personal dermatological examination. 37 (2.1%) patients were asked to see a dermatologist for a FTF follow-up examination after 3 months. All individuals were advised to have a dermatological FTF examination if symptoms persisted or worsened.
4 DISCUSSION
Demographic data regarding gender and age of patients seeking teledermatological advice are scarce, and only a few previous publications have delineated these aspects.3, 4 We could not detect a specific sex predominance in this study, which is in line with the data of previous investigations.3, 4, 6 In our cohort, the mean age of the majority of the patients was 33.7 years. This is in accordance with the results of other groups who evaluated the age distribution of patients with varied skin disorders seeking teledermatological advice.4, 6
The most common diagnosis in this study was acne, both in the overall cohort and in the follow-up cohort. These results are consistent with those of traditional office-based FTF outpatient dermatological care.7 Interestingly though, a recently published German S2k guideline on teledermatology (https://www.awmf.org/uploads/tx_szleitlinien/013-097l_S2k_Teledermatologie_2021-03.pdf) does not cover acne at all although there are numerous reports and recommendations on the management of acne patients via telemedicine (for a review see Gu L et al.8 in 2022). Thus, this guideline could probably benefit from a timely update. Surprisingly, the second most common diagnosis in the follow-up cohort was pityriasis versicolor. This finding, however, points out one of the imitations of teledermatology in general and also of our study since a diagnosis of pityriasis versicolor should not be made merely on the basis of clinical findings but always include a microscopic examination of skin scales. Not surprisingly, the group of eczema, including atopic dermatitis, hand eczema, seborrheic eczema, dyshidrotic eczema, nummular eczema, and seborrheic eczema in its entirety reflected 16.9% of all diagnoses in the overall study population, which is largely in line with previous results from the USA.9 Again interestingly in this context, the current German S2k guideline on teledermatology only covers atopic eczema (https://www.awmf.org/uploads/tx_szleitlinien/013-097l_S2k_Teledermatologie_2021-03.pdf) and does not provide any statement or advice on the other forms of eczema. Unfortunately, we could not perform any comparative subgroup analysis on the frequency of individual diagnoses since the currently available scientific work on teledermatology does not allow for any statement in this regard.10
During the follow-up, 83.3% of the diagnoses made via teledermatology in this study showed an improvement of the condition under the prescribed therapy, thus indirectly confirming the original teledermatological diagnosis. This corroborates previous results of other groups who reported a diagnostic accuracy in the range of 70%–85%.11, 12 To the best of our knowledge, the efficiency of a therapeutic regimen prescribed following a teledermatological consultation has not been systematically assessed to date. However, this aspect certainly is one of the major factors underlying patient satisfaction with teledermatology services.11 Therefore, it might be worth paying more attention to this issue in the future.
In the current study, 81.2% of the individuals who sought a teledermatological consultation did not require an additional FTF examination, in spite of the fact that each patient was encouraged to see a dermatologist in person if symptoms persisted or worsened. This is in line with previous reports or even better than the results of other groups and suggests a high level of patient satisfaction with the dermatological services provided, in particular the unique feature of a second opinion by an expert panel of highly experienced board-certified dermatologists that was provided in ambiguous and difficult cases.10, 11 Here, 326 individuals (18.3%) were deliberately referred for an additional FTF dermatological examination. As in previous studies by other groups, 92 of these individuals (28.2%) were patients with a suspected diagnosis of a skin tumor who required further diagnostic work-up.13
Taken together, we report on the largest telederamtological follow-up study on varied dermatological diseases in the context of quality assessment. Our results show that teledermatology is a valuable digital complement to the traditional dermatological FTF examination that is easily accessible for the patient at any time and associated with a high degree of therapeutic efficiency.
ACKNOWLEDGMENT
Open Access funding enabled and organized by Projekt DEAL.
CONFLICT OF INTEREST STATEMENT
All authors declare that economic interests had no influence on the preparation of the manuscript. H.L. and T.B. are student assistants at Dermanostic, Inc. J.F. is a senior consultant at Dermanostic, Inc. and an associate partner at medi-login, Inc.