Salpingitis in an Adolescent Female With Constipation and Abdominal Pain
The authors report no conflicts of interest.
Publication costs were generously supported by the Texas Children's Hospital Young Investigators Endowed Fund.
The patient provided assent and her legal guardians provided informed consent for publication of the details of this case.
Abstract
Abdominal pain is one of the most common presenting complaints in the emergency room for pediatric patients. While constipation is one of the most common causes for abdominal pain in pediatrics, serious intra-abdominal pathology must always be excluded. We report a pre-coital post-menarchal adolescent female who presented with severe abdominal pain and constipation and had radiographic findings of salpingitis. It was suspected that uterine and adnexal changes seen on imaging resulted from the fecal mass compressing the genitourinary tract leading to fluid collection manifesting as radiographic evidence of salpingitis. This mechanism is similar to bladder outlet obstruction resulting from compression by intestinal stool burden, leading to urinary stasis, bacteriuria, and ascending urinary tract infection. This case demonstrates how a common pediatric problem, constipation, can lead to a condition rarely found in the pre-coital adolescent population.
INTRODUCTION
Abdominal pain is one of the most common complaints of pediatric patients presenting to emergency center and represents a significant burden to families, contributing to increased health care costs (1-3). A broad understanding of the pathologies and sequelae causing abdominal pain is important to the pediatric gastroenterologist. Constipation accounts for 20% of all cases of pediatric abdominal pain (3). Other serious intra-abdominal pathologies, such as appendicitis and gynecologic conditions, require prompt recognition (4). We present a case of a 12-year-old girl with abdominal pain with radiographic salpingitis associated with fecal impaction.
CASE REPORT
A 12-year-old girl presented to the hospital emergency department for evaluation of acute onset right lower quadrant abdominal pain. It started 3 days prior to presentation and was sharp, constant, and worse with movement. It did not radiate and was 8 of 10 in severity. This pain was accompanied by constipation, anorexia, and dysuria. She had been treated by her pediatrician for chronic constipation complicated by encopresis. She had poor adherence to these medications. Menarche was 10 months prior with regular cycles, and last menstrual period was 2 weeks prior to presentation. In a protected social history, the patient denied romantic partners, sexual activity, or sexual abuse. The remainder of her past medical, surgical, and social history was unremarkable.
On general survey, the patient was anxious and visibly upset. Vital signs were notable for tachycardia with heart rate 108. Physical examination revealed right lower quadrant tenderness with guarding and rebound. Pelvic examination was declined by the patient and her family.
Diagnostic laboratory testing revealed leukocytosis to 16 000 with elevated absolute neutrophil count and elevated C-reactive protein of 5.2. Urine pregnancy test was negative. Urinalysis was suspicious for urinary tract infection (UTI) with evidence of pyuria and urine nitrites. Appendix and pelvic ultrasounds demonstrated an unremarkable appendix, fluid-filled uterus, and bilateral hydrosalpinges with a complex fluid collection in the left fallopian tube (Fig. 1). Findings were reported as consistent with salpingitis. Debris was noted in the urinary bladder and significant stool burden was seen in the rectum, which was also confirmed on upright x-ray.
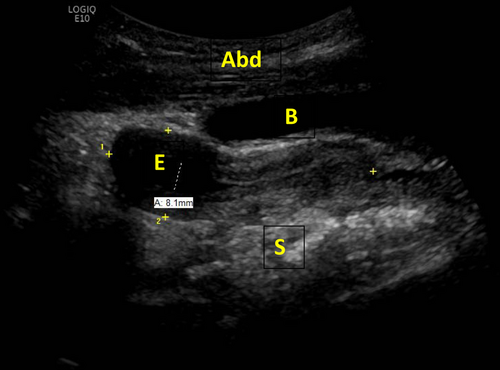
Pelvic ultrasound demonstrating a fluid-filled endometrial canal (E) measuring 8 mm in thickness. Abdominal wall (Abd), stool filled bowel (S), and bladder (B) are also visualized.
Given the findings of fecal impaction, the patient was admitted to the hospitalist service for bowel cleanout. The pediatric gynecology service recommended empiric treatment for Pelvic Inflammatory Disease (PID) and further imaging to evaluate for a Mullerian anomaly to explain an obstruction of the fallopian tubes. A contrast computed tomography (CT) scan of the abdomen and pelvis obtained early in her hospitalization demonstrated bilateral adnexal hyperemia consistent with salpingitis in addition to bladder distension, fluid in the endometrium, and mass effect of distended intestine on gynecologic structures (Fig. 2).
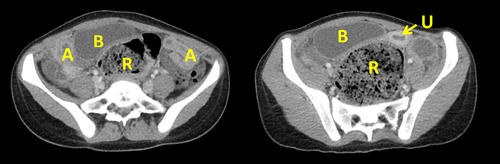
Coronal views of patient's computed tomography (CT) scan demonstrating distended rectum (R) with stool burden, adnexal (A) swelling and hyperemia, displaced and fluid-filled uterus (U), and significant bladder (B) distension.
The patient's initial tachycardia resolved with intravenous hydration and intravenous ketorolac. Empiric intravenous doxycycline and ceftriaxone were started for UTI and PID. A Golytely drip via nasogastric tube was initiated. Abdominal pain quickly resolved with passage of multiple large volume stools. Based on negative gonorrhea and chlamydia testing, antibiotics for PID were stopped. Admission urine culture grew Escherichia coli, so the patient was discharged to complete a course of oral amoxicillin-clavulanic acid. She was also discharged home on a bowel regimen with education on constipation management. She has remained well since that time with no recurrence of symptoms. Her final primary diagnosis was fecal impaction, which explained her clinical picture and radiographic, noninfectious salpingitis.
DISCUSSION
Efficient triage and treatment of patients with abdominal pain is an important skill for pediatricians. Acute gynecologic conditions are not an uncommon cause for emergency center visits in children and adolescents (5). In addition to PID adnexal complications, including tubal ectopic pregnancy, ovarian torsion, or cyst rupture can present similarly with lower abdominal or pelvic pain, nausea, and/or vomiting. Differentiation is accomplished largely by clinical history and imaging as the physical examination can be similar for each of these conditions. A patient with pain, tenderness, and free fluid on imaging would need emergent surgery for ruptured ectopic pregnancy if their urine pregnancy test was positive; however, the same patient with a negative pregnancy test would be a candidate for conservative treatment if it were believed they had a ruptured ovarian cyst.
Although not well described in the literature, this patient's uterine and adnexal changes resulted from the fecal mass compressing reproductive structures and obstructing normal outward drainage. This mechanism resembles bladder outlet obstruction, a more commonly encountered effect of constipation, in which urinary retention leads to bacteriuria and can result in ascending UTI that was also seen in this patient (6). In addition, it was hypothesized that translocation of enteric bacteria, for which constipation is a risk factor, directly to adnexal structures also contributed to localized inflammation (7). In our patient, the radiographic finding of salpingitis was alarming, and even raised concern for sexual abuse, but was ultimately due to constipation rather than an underlying infectious process.
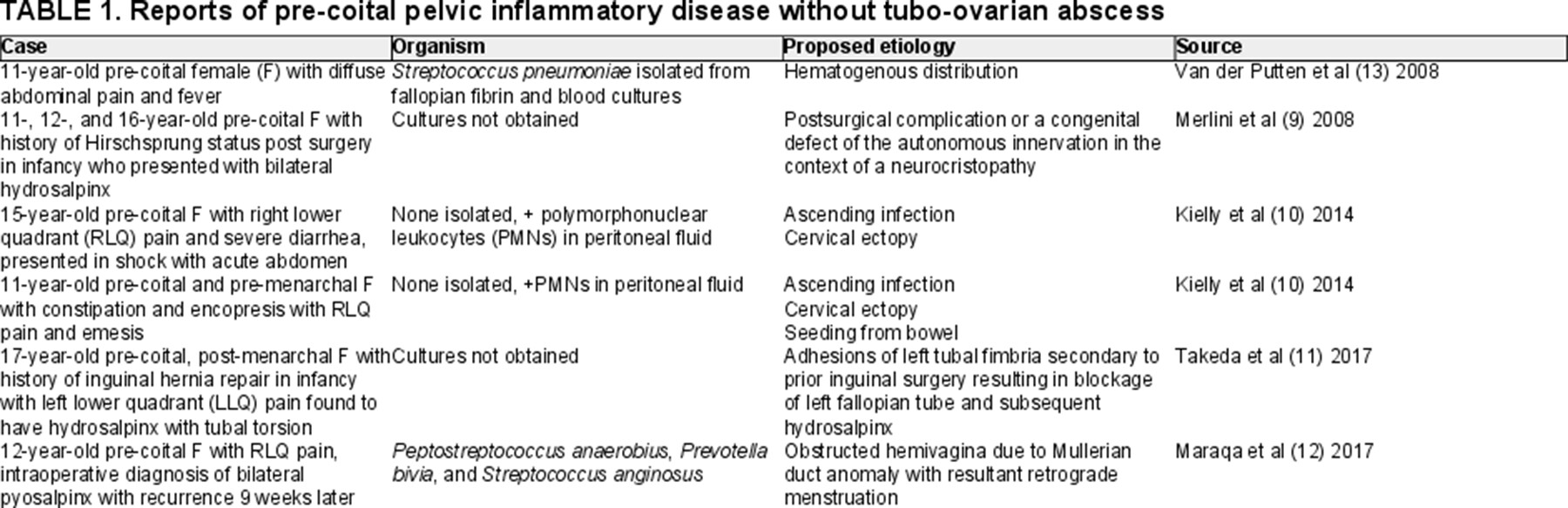
Classically, PID is defined as inflammation of the cervix, uterus, or adnexa and can include endometritis, salpingitis, tubo-ovarian abscess (TOA), and pelvic peritonitis (8). Although typically caused by sexually transmitted infections chlamydia or gonorrhea, PID can be considered a polymicrobial infection from ascending bacteria from the vagina or cervix. Approximately 15% of PID cases described are not sexually transmitted and are associated with enteric or respiratory pathogens that have colonized the lower genital tract. While the majority of published cases of pre-coital PID are those with TOA, several prior studies have identified cases of pre-coital PID without TOA in patients who presented with surgical abdomen requiring intraoperative treatment (Table 1) (9-13). Some of these cases were found to be sterile inflammatory processes, although applicability of literature review to our patient is limited, as all published cases were severe enough to require surgical treatment.
In our patient, a sterile process was suspected and the gynecology team recommended against antibiotic treatment for salpingitis. While it is possibile that a nascent infection was present in the tubes from either ascending vaginal flora or translocation of bacteria from the intestine, her rapid improvement with bowel cleanout argues that mass effect from impacted feces was the primary cause of fluid build-up and sterile inflammation, resulting in salpingitis.
This case adds to the few reports that constipation can result not only in urinary stasis and ascending UTI but also in obstruction, congestion, and inflammation of the reproductive organs.
ACKNOWLEDGMENTS
G.B. and M.R.C. participated in data collection and analysis, drafted the initial article, and reviewed and revised the article. A.L.D. conceptualized and designed the study, assisted in drafting the initial article, and reviewed and revised the article. All authors approved the final article as submitted and agree to be accountable for all aspects of the work.