Fatigue and Physical Activity Patterns in Children With Inflammatory Bowel Disease
Dr Pierik reports grants and nonfinancial support from Falk Pharma, grants from European commission, grants from ZONMW (Dutch national research fund), grants and nonfinancial support from Takeda, grants and nonfinancial support from Johnson and Johnson, grants and nonfinancial support from AbbVie, nonfinancial support from Ferring, nonfinancial support from Immunodiagnostics, and nonfinancial support from MSD, all outside the submitted work. The remaining authors report no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal's Web site (www.jpgn.org).
Sources of Funding: This work was supported through an unrestricted grant from Vifor Pharma, Glattbrugg, Switzerland; they had no role in the design nor in the collection, analysis, and interpretation of data, the writing of the report, or the decision to submit the paper for publication.
Abstract
Objectives:
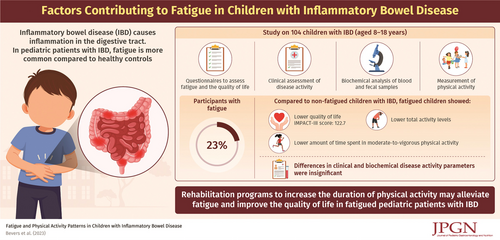
Fatigue is a common symptom in children with inflammatory bowel disease (IBD). Diagnostic tests to evaluate biological causes of fatigue commonly include markers of inflammation and hemoglobin (Hb), yet functional parameters have been inadequately studied in pediatric IBD. In this study, we compared fatigued and non-fatigued children with IBD from both a biological and functional point of view.
Methods:
A cross-sectional study of 104 pediatric IBD patients with mild to moderately active IBD was conducted. Fatigued children were defined as those with a Pediatric Quality of Life Inventory Multidimensional Fatigue Scale z score <−2.0. Non-fatigued children had a z score ≥−2.0. Disease-specific quality of life (measured with IMPACT-III score), C-reactive protein (CRP), fecal calprotectin (FC), hemoglobin z score (Hb z score), and physical activity tests including 6-minute walking distance z score (6MWD z score) and triaxial accelerometry (TA) were evaluated.
Results:
Fatigued children (n = 24) had a significant lower IMPACT-III score than non-fatigued children (n = 80). Hb z scores, CRP, FC, and 6MWD z scores were not significantly different between groups. TA was performed in 71 patients. Wear time validation requirements were met in only 31 patients. Fatigued patients spent significant shorter median time in moderate-to-vigorous activity than non-fatigued patients (18.3 vs 37.3 minutes per day, P = 0.008).
Conclusion:
Biological parameters did not discriminate fatigued from non-fatigued patients. TA possibly distinguishes fatigued from non-fatigued patients; the potential association may provide a target for interventions to combat fatigue and improve quality of life.