Endoscopic Balloon Dilatation-Based Membrane Resection for Membranous Duodenal Stenosis
A Feasibility and Safety Study (With Video)
The authors report no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.jpgn.org).
X.W. and K.L. contributed equally to the article.
Abstract
Objectives:
Surgery is generally considered as the first-line therapy for membranous duodenal stenosis (MDS) in children. However, abdominal surgery leaves permanent scars and may even cause intestinal adhesion. Therefore, an effective, safe, and minimally invasive method is urgently needed. This study aimed to evaluate the safety, efficacy, and feasibility of endoscopic balloon dilatation-based membrane resection (EBD-MR) to treat MDS in children.
Methods:
We retrospectively reviewed patients with MDS treated with EBD-MR in Shanghai Children’s Hospital from May 2016 to August 2021. Primary study outcome was clinical success, defined as weight gain and complete remission of vomiting, without the need for repeat endoscopic or surgical intervention during follow-up. Secondary outcomes included technical success, diameter changes of the membrane opening, and adverse events.
Results:
Nineteen children (9 females, mean age 14.5 ± 11.2 months) received endoscopic treatment for MDS, and clinical success was achieved in 18 of 19 patients (94.7%). No bleeding, perforation, and jaundice occurred. Diameters of the membrane opening increased from 2.97 ± 2.87 mm to 9.78 ± 1.27 mm after the treatment, symptoms of vomiting did not reappear during 10–73 months of follow-up, and body mass index of the children increased from 14.9 ± 2.2 kg/m2 (pre-operation) to 16.2 ± 3.7 kg/m2 (6 months after operation). One patient required surgical revision because of existence of a second web; three patients received 2–3 sessions of endoscopic treatment to obtain the final remission.
Conclusions:
The EBD-MR technique is safe, effective, and feasible for MDS, which provided an excellent alternative to surgical management for the disease in pediatric patients.
What Is Known
-
Surgery is the most common modality to treat membranous duodenal stenosis (MDS) in children; permanent scars are inevitable.
-
Minimally invasive treatments of pediatric gastrointestinal strictures have become popular.
What Is New
-
This study indicates that the endoscopic balloon dilatation-based membrane resection technique is safe, effective, and feasible for MDS.
-
Accurate localization of the Vater papilla is a critical step in the process of membrane resection.
-
This is the first study clearly demonstrating how to safely and effectively remove different types of membrane endoscopically.
Membranous duodenal stenosis (MDS) is one of the common pediatric gastrointestinal (GI) abnormalities with an incidence of 1:10,000–40,000 (1.). Recurrent vomiting and malnutrition are the most dominant clinical signs of the disease; the appearance of clinical presentation depends on the size of the fenestrations of the membrane. Traditional management has been open surgery with bypass or resection of the membrane (2.); even in the relatively minimally invasive laparoscopic surgery, duodenal wall still needs to be cut open during the operation, which may result in postoperative anastomotic leakage or intestinal adhesions (1.,3.). Besides, due to the position relationship between membrane and the Vater papilla is difficult to judge accurately in some cases, imprudently incision of duodenum may even lead to serious consequences of accidental injury to the Vater papilla.
It has become a new development trend that maximally excising the lesion with the greatest possibility while preserving the integrity of tissue anatomical structure and ensuring organ’s normal function (4.). Endoscopic techniques have shown great advantages in the treatment of the disease which is both minimally invasive and cosmetically satisfying. There have been some sporadic reports of endoscopic management of MDS. However, previous literatures were majorly case reports (2.,5.,6.). In addition, there is variation in the position relationship between the Vater papilla and membrane among different children. To date, no studies have clearly demonstrated how to safely and effectively remove different types of membrane endoscopically. We applied endoscopic balloon dilatation-based membrane resection (EBD-MR) technique to treat MDS in 19 children, and the results were encouraging.
METHODS
Patients
This was a retrospective study including 19 children with MDS who were treated endoscopically at a single center over a 5-year period; all children had varying degrees of vomiting. Body mass index (BMI) was used to assess nutritional status of the children. Preoperative upper GI tract radiography revealed markedly dilated of duodenum bulb or incomplete duodenal obstruction (Figure S1, Supplemental Digital Content 1, http://links.lww.com/MPG/D185). B-ultrasound, computerized tomography (CT), or magnetic resonance imaging were conducted to exclude diseases like annular pancreas and intestinal malrotation; MDS were finally confirmed by gastroscope. All the participating children had no prior history of surgery; written informed consents were signed by their parents. Children were fasted for 12 hours before operation, and all procedures were performed under general anesthesia through orotracheal intubation. Flow diagram of endoscopic treatment in the 19 children are given in Figure 1. The study protocol was approved by the institutional review board of Shanghai Children’s Hospital (2020R051-E01).
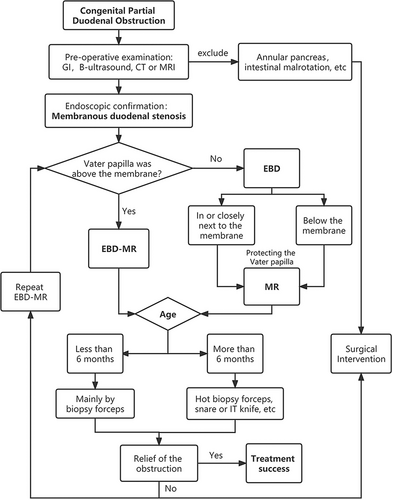
Flow diagram of endoscopic treatment in the 19 children with membranous duodenal stenosis.
The EBD-MR Procedure
It can be divided into the following main steps (Fig. 2, Video S1, Supplemental Digital Content 2, http://links.lww.com/MPG/D186):
-
Exploration of the membrane and estimation of its thickness by using a zebra guide wire and biopsy forceps.
-
Clarify the position relationship between the Vater papilla and membrane, especially if the Vater papilla was not above the membrane, balloon dilation of the membranous stenosis was needed to facilitate the passage of a gastroscope to identify location of the Vater papilla; right middle abdominal compression would also be helpful.
-
Treatment of the membrane, since the membrane was relatively thin for children under 6 months, so the treatment was dominated by EBD, after that, the sheet-like membrane tissue could be removed by using biopsy forceps. For children more than 6 months, the membrane was relatively thick and may contain a muscular layer, an endoscopic scissor was employed to radially separate the mucosa (avoid the 8–11 o’clock direction), and then the remaining membrane after EBD could be resected by a hot biopsy, snare, or an insulated-tip knife. Always keep in mind that all endoscopic treatments should be conducted on the basis of protecting the Vater papilla.
-
Resected tissues were sent for pathologic examination, and a nasojejunal tube was placed if necessary.
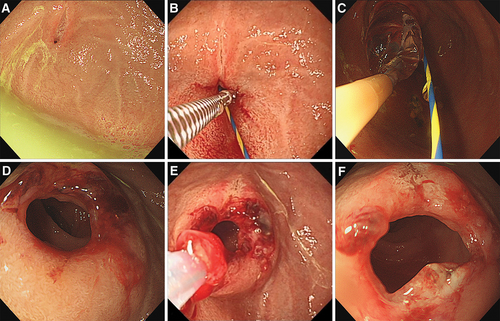
Endoscopic views of endoscopic balloon dilatation-based membrane resection (EBD-MR) procedure in a 9-month-old child. (A) Dilated duodenum bulb accompanied with bile retention; an eccentric opening about 2 mm in diameter was in the 11 o’clock direction. (B) Radial incisions of the membrane using an endoscopic scissor. (C) A 12 mm balloon dilator was employed to dilate the stenosis. (D) The stenosis was obviously enlarged after balloon dilation. (E) The residual membrane tissue was resected by a snare. (F) The opening was enlarged to 1.2 cm in diameter after the treatment. EBD-MR = endoscopic balloon dilatation-based membrane resection.
Outcome Measurement and Follow-Up
Anti-infection, acid suppression, and rehydration therapy were given to the children; abdominal X-ray were performed to exclude perforation during the operation if necessary or the same day after operation; serum amylase and lipase were examined the next day. They could drink water after being fasted for 12 hours, then started on a liquid diet 48 hours later, and gradually advanced to a normal diet 3 days after the operation; symptoms of hematemesis, melena, and jaundice were recorded. During the follow-up period, the changes of body weight and dietary structure were monitored at 3 and 6 months after the operation, respectively. Upper GI examinations were made to check the changes of duodenal obstruction, and subsequent follow-up was achieved via telephone to record whether vomiting reappeared.
Statistical Analysis
The statistical analyses were performed using SPSS Statistics v23.0 (IBM Corp., Armonk, NY). The mean and standard deviation were calculated for quantitative variables and frequency (%) was used for qualitative variables.
RESULTS
Patient Characteristics
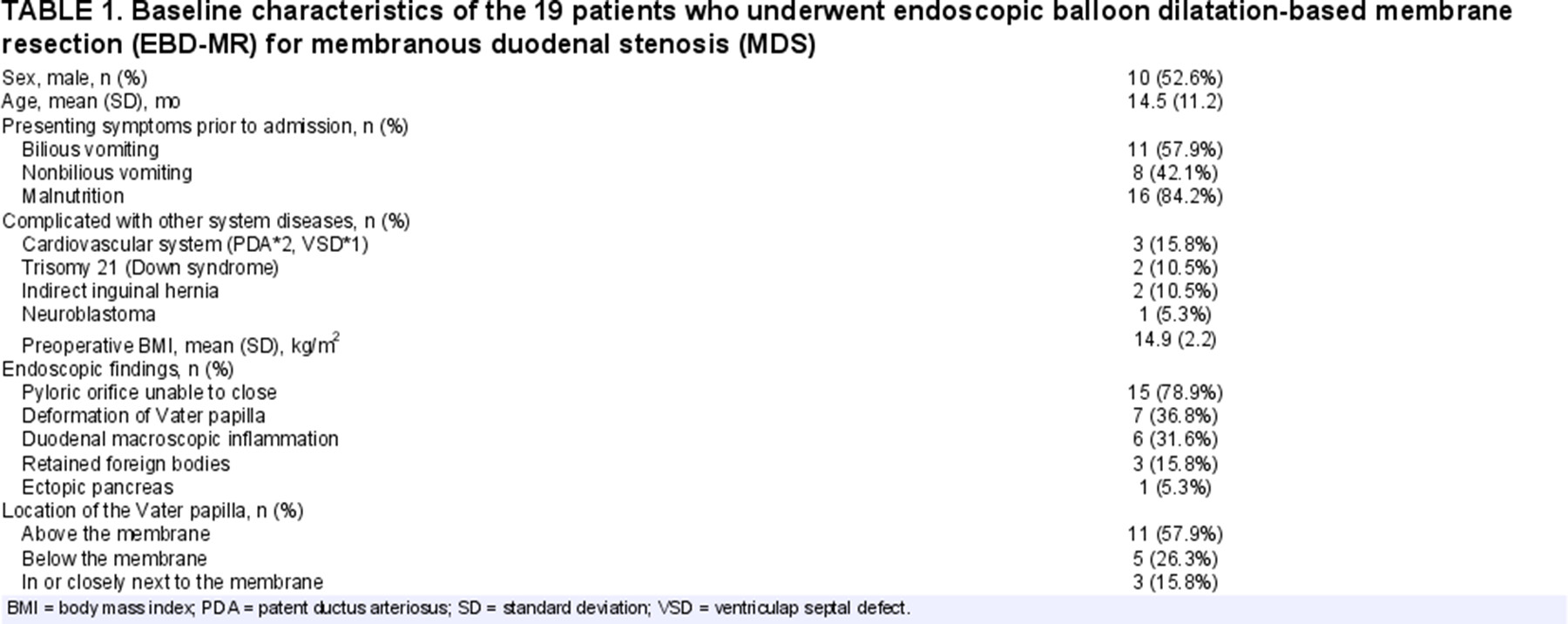
A total of 19 children (9 females) ranging in age from 17 days to 39 months (mean age 14.5 ± 11.2 months) were enrolled in the study. General information of the children was shown in Table 1. All patients presented with a history of recurrent vomiting prior to admission; 11 of them were bilious vomiting and 8 of them were nonbilious vomiting, 16 children (84.2%) had malnutrition, and 6 cases (31.6%) were complicated with other system diseases. Preoperative BMI was 14.9 ± 2.2 kg/m2. Gastroscopy revealed pyloric orifice unable to close (15/19), deformation of Vater papilla due to traction (7/19), duodenal macroscopic inflammation (6/19), retained foreign bodies (3/19), and ectopic pancreas (1/19) (Figure S2, Supplemental Digital Content 1, http://links.lww.com/MPG/D185). Among the 19 children, the Vater papilla were located above the membrane in 11 cases, below the membrane in 5 cases, and 3 cases were located in or closely next to the membrane (Figure S3, Supplemental Digital Content 1, http://links.lww.com/MPG/D185).
Treatment Outcomes
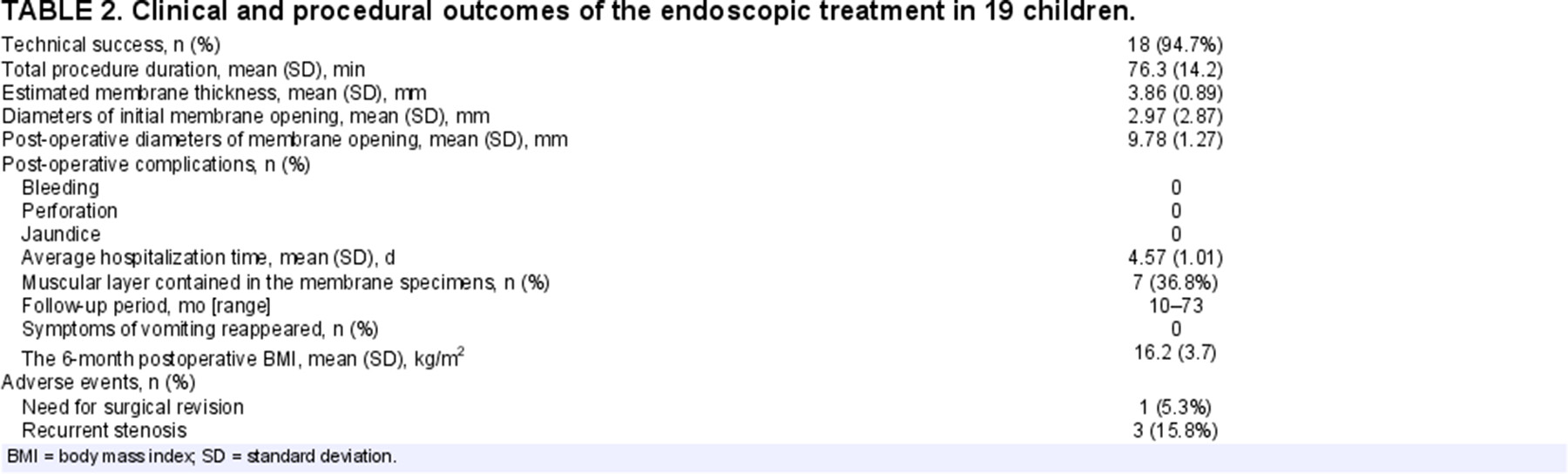
The operation time ranged from 47 to 103 minutes (mean 76.3 ± 14.2 minutes) and the estimated membrane thickness ranged from 2 to 6 mm (mean 3.86 ± 0.89 mm). Diameters of initial membrane opening ranged from 1.5 to 5 mm (mean 2.97 ± 2.87 mm), while they were enlarged to 7–12 mm (mean 9.78 ± 1.27 mm) after the operation, and a standard endoscope (8.9 mm, GIF-H290, Olympus, Japan) could pass through without resistance. No complications like bleeding and perforation occurred during and after operation; the results of serum amylase and lipase were within normal limits. Pathological results showed muscular layer was found in 7 cases of the membrane specimens (Figure S4, Supplemental Digital Content 1, http://links.lww.com/MPG/D185). The average hospitalization time was 4.57 ± 1.01 days.
During the follow-up period of 10–73 months, no vomiting, abdominal distension, and jaundice appeared in all patients; the 6-month postoperative BMI had increased to 16.2 ± 3.7 kg/m2. Upper GI examinations showed significant improvements of the duodenal obstruction than before (Figure S5, Supplemental Digital Content 1, http://links.lww.com/MPG/D185). The dietary structure, growth, and development of the children gradually returned to normal.
Adverse Events
One patient required surgical revision for a second web exist distal to the first one, and the guidewire was unable to traverse through the second membrane. Three patients aged more than 15 months received 2–3 sessions of endoscopic intervention to obtain final remission, however, the degree of stenosis in the second or third time was significantly alleviated than the previous one. Details of clinical and procedural outcomes of the endoscopic treatment were shown in Table 2.
DISCUSSION
MDS (also known as fenestrated duodenal web) is one of the important causes of duodenal obstruction in children (7.). Incomplete recanalization of the duodenal epithelium during the 4th and 5th weeks of gestation is believed to be an important cause of the disease. Membrane can appear at any site of the duodenum, but it is most commonly located near the duodenal ampulla; it was reported that 69% of the duodenal papilla are located near the inside and anal side of the adherent site of the web (8.). Surgery is the only effective treatment for patients with MDS. Currently, laparoscopically longitudinal duodenotomy with excision of the membrane and transverse closure of the duodenotomy is the most prevalent approach for duodenal web in department of pediatric surgery (9.), although the trauma has been greatly reduced compared with open surgery; some complications like intra-abdominal adhesions were reported (10.). As minimally invasive and effective modalities, modern endoscopic techniques have revolutionized the management of duodenal membranes.
Compared with traditional surgery, endoscopic therapy could treat the lesion through a natural orifice under direct vision, with no abdominal scars and less disturbance to extraluminal organs. In 1989, Okamatsu et al (11.) first reported excision of the duodenal membrane by gastroscopic electrocauterization. With the development of endoscopic techniques, cases of endoscopic treatment of duodenal membrane gradually increased in both adults and children. Nose et al (12.) reported on the use of a snare electrocoagulation technique to resect the membrane by trapping it into a suction sleeve, however, such approach was considered to be effective only for “windsock” deformity. There are other clinicians reported membrane resection using laser, papillotome or polypectomy snare via gastroscope in adults (13.-15.). Nevertheless, considering the narrow space and thinner walls of duodenum in children, membranectomy cutting technique without balloon dilatation is potentially hazardous. On one hand, the preoperative relationship between the location of the duodenal papilla and the web is unclear in most cases of duodenal web (15.). And on the other hand, there exists a certain degree of traction on duodenal mucosa as gastroscope enters the duodenum, direct electrocoagulation resection increases the risk of intestinal perforation or injury to the Vater papilla (16.). It is worth mentioning that although no perforation occurred in our study, we had pediatric surgeons stood by in case of any unforeseen complications during the operation.
Recently, Poddar et al (17.) reported using balloon dilatation alone to treat 3 children with MDS; each balloon dilatation lasted for 3 minutes and the procedure was repeated every 3 weeks; success was achieved after repeated 2–4 sessions of dilatation. Similarly, in our study, 3 patients aged more than 15 months received 2–3 sessions of endoscopic intervention to obtain final remission. We speculated that there might be 2 reasons, the initially 1–2 treatments in the 3 cases were mainly occupied by endoscopic balloon dilatation, and the dilated membrane openings after the treatment were narrowed due to the scar contracture, resulting in recurrence of the vomiting symptoms. Moreover, muscular layer was found in 2 cases of their membrane specimens, which made the membrane relatively difficult to remove. Therefore, balloon dilatation, needs to be further combined with membrane resection to achieve a stable therapeutic effect.
Accurate localization of the Vater papilla is a critical step in the process of membrane resection, which has not been emphasized in previous studies. In our study, there are 8 children whose Vater papilla could not be identified directly by gastroscopy, except for 5 cases were below the membrane, the rest were just located in or closely next to the membrane. As for them, we first used a balloon of appropriate size for fully effective dilation so that the narrow openings were enlarged for passage of an endoscope, then accompanied by right middle abdominal compression; generally, the Vater papilla could be identified on inner side of the duodenal lumen with bile or bubbles flowing out (18.). For excision of the membrane, we chose 6 months as the boundary to select different approaches, considering that children under 6 months old were mainly fed with breast milk or formula, whereas for children more than 6 months, membrane might be thickened and expanded passively with the addition of complementary foods. Especially, the endoscopic treatment for neonates was a challenge for both anesthesiologists and endoscopists; both an ultrafine endoscope and 8 mm balloon dilator were employed, and membrane tissue was removed by using biopsy forceps instead of an electric knife (Figure S6, Supplemental Digital Content 1, http://links.lww.com/MPG/D185). Besides, a second web exist distal to the first one was found in a patient; this rare deformity has also been reported previously (19.,20.), which needs our considerable attention before operation.
During the endoscopic procedures, there are still some specifics should be noted. The zebra guidewire functioned as support while performing cold radially incision of the membrane with an endoscopic scissor; 8–11 o’clock direction should be avoided as the opening site of the duodenal papilla may located in that direction behind the membrane. The balloon size varies according to the age of the child and different size of the membrane opening, typically, 8–10 mm dilators were suitable for neonates or infant aged less than 6 months, while 12–16 mm dilators were more preferable for children older than that. Each balloon dilatation lasted 2 minutes, and the step was repeated 2–3 times with an interval of 3 minutes; the dilated area should be closely observed for bleeding and perforation during the procedure. In addition, the operation required delicate endoscopic manipulation so that the endoscopist should have extensive experience in pediatric endoscopic interventions and be skilled of various endoscopic tools.
Although to our knowledge we present the largest series of endoscopic management of MDS in children to date, it was a single-center, retrospective study with a relatively small number of children. Furthermore, the EBD-MR technique was only suitable for fenestrated duodenal web. Therefore, further studies with multicenter, larger number of cases are necessary to assess the superiority and limitations of this method.
CONCLUSIONS
In conclusion, EBD-MR is feasible, safe, and effective to treat MDS in children. Accurate localization of the Vater papilla is one of the critical steps in the EBD-MR technique, and all steps should be conducted delicately on the basis of protecting the Vater papilla. Overall, the EBD-MR technique may provide an excellent alternative to surgical operation without abdominal scars. It is worthy of wide application in pediatric patients.