Pancreatitis-Associated Medication Use in Hospitalized Pediatric and Young Adult Patients With Acute Pancreatitis
The authors report no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.jpgn.org).
Sources of Funding: This study was supported by the National Institute of Diabetes and Digestive Kidney Diseases of the National Institutes of Health (award number T32 DK0074477 to LVC).
Abstract
Objective:
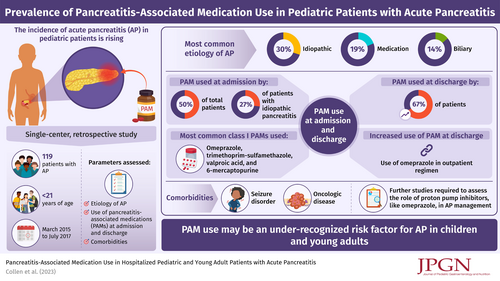
The objective of this study is (1) to describe the prevalence of pancreatitis-associated medication (PAM) use at admission and discharge in pediatric and young adult patients hospitalized with acute pancreatitis (AP) and (2) to describe the prevalence of PAM use at admission in patients classified as having idiopathic AP.
Study Design:
A single-center retrospective study of patients <21 years who were hospitalized with AP or acute recurrent pancreatitis from March 2015 to July 2017 was performed. Charts were reviewed for demographic data, etiology of pancreatitis, comorbidities, and use of PAMs at admission and discharge. PAMs were defined and scored based on an evidence-based classification system, with class I PAMs having strongest evidence for causation. Standard descriptive statistics were used to report prevalence data.
Results:
Our cohort was comprised of 119 patients; 50% of patients were using a PAM at admission and 67% were taking a PAM at discharge, reflecting a significant change (P = 0.0009); 44% of patients classified as having idiopathic pancreatitis were taking a PAM on admission, reflecting a possibly missed role of medication in their presentation. Comorbidities significantly associated with PAM use included seizure disorder (P = 0.005) and oncologic disease (P = 0.005). The most commonly used class I PAMs were omeprazole, trimethoprim-sulfamethazole, valproic acid, and 6-mercaptopurine. The increase in prevalence of PAM use at discharge compared to admission was partially driven by addition of omeprazole to the outpatient medication regimen during the hospital stay (P = 0.07).
Conclusion:
Medications likely play an under-recognized role in pediatric AP. The practice of using proton pump inhibitors in management of AP warrants further study.