Open Primary Button Versus Laparoscopic Percutaneous Endoscopic Gastrostomy
Results From a Case-control Study
An infographic is available for this article at http://links.lww.com/MPG/B902.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal's Web site (www.jpgn.org).
J.R.D. carried out this work while part-funded as an NIHR Academic Clinical Fellow at the UCL-GOS Institute of Child Health. All research at UCL Great Ormond Street Institute of Child Health is made possible by the NIHR Great Ormond Street Hospital Biomedical Research Centre. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
The authors report no conflicts of interest.
ABSTRACT
Objectives:
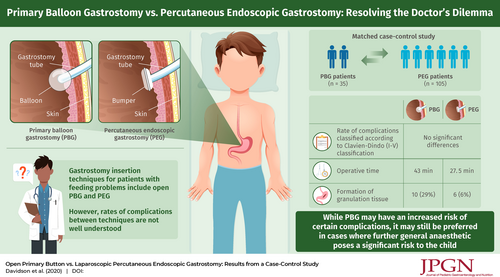
Open primary balloon gastrostomy (PBG) presents a potential alternative to percutaneous endoscopic gastrostomy (PEG) in children as it obviates the need for change under general anaesthetic; however, the complication profile of PBG compared to PEG is not well defined. Previous series comparing the two have been hampered by the groups not being equivalent. Our paediatric surgical centre has offered PBG as an alternative PEG since 2014. We used a matched case-control study to compare outcomes for PBG and PEG.
Methods:
Patients undergoing PBG were used as “cases” and matched 1:3 by age and diagnosis to patients undergoing PEG, demographics, and clinical data as “controls.” Primary outcome was rate of complications classified according to Clavien-Dindo (I-V). Secondary outcomes included time to feed and length of stay. Non-parametric, categorical and multivariate logistic regression analyses were performed. Data here presented as median with interquartile range (IQR).
Results:
We included 140 patients (35 PBG:105 PEG). The 2 groups were comparable for sex, weight at surgery, and follow-up duration. Median operative time was longer for PBG (43 min [IQR 36.5–61.5] vs 27.5 min [18.25–47.75], P < 0.001). Multivariate analysis demonstrated a statistically significant, higher incidence of symptomatic granulation tissue in PBG (10 [29%] vs 6 [6%], P = 0.0008), this remained significant on multivariate analysis (OR 7.56 [2.33–23.5], P = 0.001), no other complication remained significant. The overall complication rate was not statistically different.
Conclusions:
PBG and PEG have similar overall complication rates; however, PBG appears to have a higher incidence of granulation tissue. This observation must be weighed against the need for further general anaesthetic which is not insignificant in medically complex children.