Intestinal Rehabilitation Programs in the Management of Pediatric Intestinal Failure and Short Bowel Syndrome
R.J.M. holds stock in Abbott Labs, Abbvie, Johnson & Johnson, is a retiree from Abbott Labs and is a clinical site investigator for Shire Pharmaceuticals. B.W.W. serves on the Scientific Advisory Board for Prolacta Biosciences and is serving on a Data Safety and Monitoring Board for Shire Pharmaceuticals. P.S.G. has served as a consultant for Fresenius Kabi and Nutricia and is serving on a Data Safety and Monitoring Board for Shire Pharmaceuticals. V.C. has served on Speakers Bureaus for Abbott Nutrition and Nutricia. The remaining authors report no conflicts of interest.
ABSTRACT
Intestinal failure is a rare, debilitating condition that presents both acute and chronic medical management challenges. The condition is incompatible with life in the absence of the safe application of specialized and individualized medical therapy that includes surgery, medical equipment, nutritional products, and standard nursing care. Intestinal rehabilitation programs are best suited to provide such complex care with the goal of achieving enteral autonomy and oral feeding with or without intestinal transplantation. These programs almost all include pediatric surgeons, pediatric gastroenterologists, specialized nurses, and dietitians; many also include a variety of other medical and allied medical specialists. Intestinal rehabilitation programs provide integrated interdisciplinary care, more discussion of patient management by involved specialists, continuity of care through various treatment interventions, close follow-up of outpatients, improved patient and family education, earlier treatment of complications, and learning from the accumulated patient databases. Quality assurance and research collaboration among centers are also goals of many of these programs. The combined and coordinated talents and skills of multiple types of health care practitioners have the potential to ameliorate the impact of intestinal failure and improve health outcomes and quality of life.
What Is Known
- Intestinal failure is a debilitating condition that presents both acute and chronic medical management challenges.
- Intestinal Rehabilitation Programs exist in multiple sites across North America and Europe.
What Is New
- Management of intestinal failure by Intestinal Rehabilitation Programs is the current state of the art, with limited but highly encouraging, supporting data on their medical efficacy.
- NASPGHAN endorses management of patients with intestinal failure by, or in consultation with, centers with intestinal rehabilitation programs and encourages further research on the medical efficacy, patient satisfaction and quality of life, and financial impact of intestinal rehabilitation programs.
PEDIATRIC INTESTINAL FAILURE AND SHORT BOWEL SYNDROME
Intestinal failure (IF) is a rare, potentially life-threatening and debilitating condition that presents both acute and chronic medical management challenges. IF is a clinical disorder resulting from intestinal obstruction, dysmotility, surgical resection, congenital defect, or disease-associated loss of absorption and is characterized by the inability to maintain protein, energy, fluid, electrolyte or micronutrient balance. IF is an umbrella term for conditions requiring parenteral support either in the form of parenteral nutrition (PN) or intravenous hydration (1.-3.). Short bowel syndrome (SBS) is the most common cause of IF. The vast majority of pediatric patients experience onset of their condition at birth or during early infancy. Wessel and Kocoshis (4.) made an important distinction between IF and SBS in that SBS is associated with significant loss of absorptive surface area, whereas IF is a lack of satisfactory absorption. Therefore, patients who have SBS may have IF, whereas patients who have IF may not have SBS. This article focuses on SBS with associated IF. Some SBS patients with global bowel dysfunction from massive intestinal loss are at risk for irreversible, chronic intestinal failure, a highly disabling condition.
Definitions of SBS-associated IF have included 2 important concepts: a shortened length of intestine and a need for prolonged PN. The Canadian Association of Pediatric Surgeons defined SBS as the need for PN greater than 42 days after bowel resection or a residual small bowel length of <25% expected for gestational age (3.). The Pediatric Intestinal Failure Consortium defined IF as the need for PN for >60 days due to intestinal disease or dysfunction (5., 6.). The use of percentage expected bowel length has been used by others to define SBS and for reporting clinical outcomes of SBS patients. The late Daniel Teitelbaum's group used the <25% expected bowel length definition (7.); this group and others have reported outcomes based on the percentage of residual small bowel length (8., 9.).
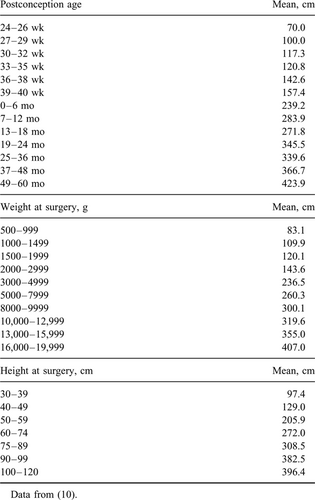
Reference values based on multiple autopsy studies have been generated and published for intestinal length in children of all ages (10.). More recently, measurements from living children up to 5 years were prospectively done and reference tables developed (11.) (Table 1) (10.). In general, the coefficient of variation for the 108 measurements standardized for post-conception age, length or weight was <10%. The curve fits for these determinants were non-linear. Based on the need for standardization, the experience of Wales et al(3., 11., 12.)and advocacy for this method by others(7., 13.), we recommend that reference values based on the child's height (preferably), weight or age be used as the standard for expressing the percentage of small bowel that remains.
Based on usage in recent clinical publications and the need for a commonly accepted definition of intestinal failure and SBS, North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN) recommends a definition of intestinal failure as the need for PN for >60 days due to intestinal disease, dysfunction, or resection. The recommended definition of SBS is the need for PN for >60 days after intestinal resection or a bowel length of <25% of expected. It is further recommended that patients who meet one or both of these criteria have access to an Intestinal Rehabilitation Program for consultation or clinical management.
The incidence of SBS is approximately 24.5 per 100,000 live births per year (3.). The prevalence has increased over the past several decades with improved survival of affected children due to advances in nutrition support (7., 14.) and neonatal intensive care, anesthesia, and surgical techniques. Among pediatric SBS patients, the most common etiologies are necrotizing enterocolitis (NEC), gastroschisis, volvulus, intestinal atresia, complicated meconium ileus, and aganglionosis. In 1 study of infants, NEC was the etiology of SBS in 35% of the patients, and the next most common cause was gastroschisis (18%) (15.). These percentages are similar at most centers, but can vary by geographic location (4., 6., 16.).
Intestinal “adaptation” is the innate response of the small intestine that normally follows sudden loss of intestinal absorptive surface area, such as from surgical resection (17., 18.). It is characterized by progressive anatomic and physiologic changes that improve fluid, electrolyte, and nutrient absorption and allow progress toward normal growth, body composition, and enteral autonomy. Adaptation begins shortly after intestinal resection and is generally complete within 24 to 60 months (6., 13., 14., 19.-24.). Intestinal rehabilitation (IR) seeks to maximize this response through medical and surgical interventions that lead to enteral autonomy.
Morbidity in patients with SBS and IF includes derangements in fluid and electrolytes, complications of central venous catheters, including central venous line-associated blood-stream infections (CLABSI), complications related to the underlying bowel disorder, liver failure, a lower quality of life (25.), and high costs of care. Medical management to bring patients back, or closer, to enteral autonomy includes infusion of parenteral fluid, electrolytes, and nutrition while medications are employed to control symptoms and fluid balance, and enteral nutrition is advanced to promote bowel adaptation (4., 26.-28.). Surgical interventions to help promote intestinal adaptation and enteral autonomy may include feeding enterostomies, ostomy closure following prior bowel resection, procedures to slow intestinal transit (29.-31.), and intestinal lengthening procedures such as serial tapering enteroplasty (STEP) or Bianchi procedures (32.-37.). Patients who fail medical and surgical therapy, those with little potential for IR, or those who develop intractable complications become potential candidates for intestinal transplantation. Because liver failure from intestinal failure-associated liver disease (IFALD) has been an important complication of pediatric SBS, historically more pediatric intestinal transplants included livers than adult patients undergoing intestinal transplantation. In recent years, the percentage of pediatric intestinal transplants both with and without liver transplantation has, however, decreased (22.). Given evidence of more interventions and improved outcomes in patients managed by IR programs, even when patients are not clearly potential candidates for transplantation, non-transplant–related benefits are gained from referral, including interventions to reduce CLABSI, intravenous lipid modification, treatment of small intestinal bacterial overgrowth and surgical bowel lengthening, all of which may help improve outcomes. NASPGHAN recommends that patients SBS patients not making progress towards enteral autonomy and continuing on PN >3 months, those with high clinical complexity or with worsening or non-resolving IFALD, recurrent sepsis, deep vein thrombosis or loss of venous access be referred to an IR program for consultation or management(38.). Although non-SBS IF is beyond the focus of this review, similar recommendations appear appropriate for these patients as well.
Mortality and morbidity in SBS-related IF patients are often associated with residual small bowel length (negatively), absence of the ileocecal valve, recurrent episodes of sepsis, IFALD, and timing of ostomy closure (14., 17., 18., 20., 39.-41.). An intact colon has also been found to be protective (14.). In a review by Pironi et al (21.), risk factors for mortality in pediatric IF included age <1 year, lack of a nutrition care team, shorter small bowel remnant, ileostomy, and evidence of chronic liver disease. In a single-center report on pediatric outcomes, patients presenting with elevated bilirubin and bowel length <10% of predicted, however, still achieved good outcomes with aggressive medical and surgical therapy (9.). In a 4-year period, this center's overall survival among 51 patients (almost all SBS patients) was 90%. A more recent report from this same group confirmed a high survival rate (96%) in patients with ultra-short bowel patients (defined by them as <20 cm of small intestine) (42.). Among SBS patients, those with a diagnosis of NEC seem to fare better (8., 42., 43.), although not universally (21.). As reported in several large series of patients awaiting transplantation, death is most commonly associated with liver failure and/or sepsis (21., 43.-45.). Late referral for IR and transplantation in the context of transplantation is thought to contribute to this finding (38., 45.-47.). In general, patients in IR programs with diagnoses other than SBS (ie, motility disorders, congenital enteropathies, or immune deficiencies) tended to have worse outcomes (48., 49.).
Achieving enteral autonomy in IR programs has been related to longer relative or absolute bowel length (14., 50.), especially for gastroschisis and atresia (45.), lower bilirubin at referral (45.), and resolution of hyperbilirubinemia on medical and surgical therapy (51.). Presence of the ileocecal valve in the native intestine was a predictor for enteral autonomy without transplantation (14., 41.), and colonic resection was a reported negative predictor in one of these studies (14.). All care at a specific IR program center and surgical bowel lengthening were also predictive factors in 1 report (50.). A consortium of 14 North American centers identified factors statistically associated with achieving enteral autonomy in IF in 172 children that included diagnosis of NEC, lower bilirubin, longer residual bowel length, preserved ileocecal valve, and care at a non-transplant center (52.). Preserved ileocecal valve was not a significant factor in the subpopulation of 144 children with measured bowel length (52.). Failure to achieve enteral autonomy is ultimately associated with risk for increased mortality.
In the recent novel-lipid and lipid-restriction era, the number of patients listed for intestinal transplant appeared to sharply decline (22.), and NEC and congenital gastrointestinal tract anomaly-related SBS have decreased as a percentage of causative reasons among patients newly listed for transplant (53.). The number of intestinal transplants peaked in 2007 at approximately 111. By 2013 the number had decreased to 36 and more recently has risen to 58 in 2015 (22.). Interestingly, children referred for transplantation in the UK from centers with nutrition support programs had better short-term survival (54.). United Network for Organ Sharing data from 2008 indicated that transplant centers with well-established IR programs had higher pediatric 1-year transplant graft survival (67%–79% vs 45%–60%) (55.).
The economic cost of managing SBS-related IF is high and adds to the motivation to minimize patient morbidity and use medical and related resources effectively and efficiently. The mean annual cost of care for this population, when receiving PN, in 2005 dollars, was determined to be approximately $500,000 in the first year and $300,000 in the subsequent 4 years at a children's hospital in Michigan (56.). Costs appear to be somewhat less in Europe. In the Netherlands, initial hospitalization costs for neonates in 2009 were estimated at about $219,000 and total 3 year costs at $431,000 (25.). In the UK, the cost of care for a stable home PN patient was estimated at roughly US$285,000 in 2006 (57.). Estimates and comparisons are fraught with issues regarding costs captured, billed versus paid costs, the population reported, the year of the study, and the currency conversion factor. There is also an additional heavy financial burden experienced by families associated with travel and lost productivity (57.).
INTESTINAL REHABILITATION PROGRAMS
Intestinal failure is analogous to other diseases with both emergent and chronic threats to health and well-being such as renal failure, heart disease, or diabetes. Like other severe, chronic medical conditions, it can be the dominating factor in an individual's life by restricting growth, development, productivity, and longevity. In fact, the condition is incompatible with life in the absence of the safe application of specialized and individualized medical therapy that includes surgery, medical equipment, nutritional products, and standard nursing care. The combined and coordinated talents and skills of multiple types of health care practitioners have the potential to ameliorate the impact of this condition and improve health outcomes and quality of life.
Intestinal Rehabilitation Programs for the care of patients with IF emerged from experience with multidisciplinary programs in other diseases such as renal failure, hospital units with expertise in complex surgical care, and nutritional support and solid organ transplantation programs (40., 44., 47., 48.). Institutional protocols for the various components of the care of these patients have enormous potential to identify and reduce complications for patients requiring nutritional support. Publications on the experience of IR programs began appearing in the mid 1980s and reports of single center experiences accelerated in the mid 2000s. IR Programs (or their equivalent) are now documented in the medical literature from multiple sites across North America and Europe.
The process for establishing a program has been described (58.). The first step includes a needs analysis and identification of the services to be included. The second is establishing the specific components of interest related to diagnosis, nutrition, surgery, and transplantation followed by creation of a business plan and budget. These authors also stress the importance of objectively demonstrating the success of the program early in its development to assure its survival. Guidance has been published on computerized data forms for accumulating standardized details of the medical and surgical history, current anatomy of the patient, diagnostic tests and surgical procedures, nutritional assessment, and fluid, food, and nutrient intake and output (45., 58.). Many of these data can be incorporated into the electronic medical record.
The mission of IR programs is to be regional, national, and/or international referral centers that provide comprehensive, safe, state-of-the-art care to improve the survival and quality of life and minimize complications in patients with IF (15., 38., 44.). The overarching goals of an IR program are to promote intestinal adaptation and enteral autonomy while decreasing the morbidity and mortality of IF. Various nutrition-related goals of an IR program include: provision of the most appropriate nutrition to support the growth and development of children with IF, best decision making for transition from parenteral to enteral nutrition, and prevention of macro and/or micronutrient deficiencies.
Promotion of enteral autonomy is achieved by enteral nutrition, maintaining somatic growth, and optimizing the bowel absorptive surface through non-transplant surgical techniques. Prevention and management of complications such as CLABSI, venous thrombosis, catheter malfunction and repair, and IFALD are of paramount importance. In the absence of enteral autonomy, an IR program should be cognizant of emerging indications for transplantation in individual patients and of the benefit of early transplant evaluation in this population. Hence, collaboration with an intestinal transplant team is essential. An IR program should strive to support families of children with IF and improve their quality of life. Research should be an important goal of every IR program. Given the small numbers of patients at any given center, it is important to strive for consistency among centers via collaboration and education for development of evidence-based care pathways and biorepositories, as well as translation of basic science discoveries (5., 59.).
Indications for referral for consideration of intestinal transplantation are not well standardized and appear to be evolving with improved IR. Ultra-short bowel and poor intestinal function (e.g., congenital enteropathies) are less predictive today of clinical need for transplantation than in the past (46., 60.-62.). Current criteria relate more to the severity of morbidities associated with providing PN, including refractory IFALD, depletion of central venous catheter access and repeated need for intensive care unit admission. In a single-center experience, the best predictors were ≥2 admissions to the intensive care unit, loss of ≥3 central vein sites and conjugated bilirubin >75 μmol/L (4.4 mg/dL) despite 6 weeks of lipid-modification therapy (61.).
Some IR programs are focused on adult patients, others on children, and many provide care to all age groups. Functions include assessment of the underlying condition and its prognosis, inpatient medical, nutritional and surgical maximization of intestinal function, support of normal growth, patient and caregiver education and, in most centers, careful selection of patients for, and performance of, intestinal transplantation and provision of post-transplant care. Another valuable role of these programs is to collect initial and subsequent data about patients with IF for tracking patient outcomes, improving quality of care, and supporting clinical research (45., 63.). Indeed, most of what we know about the outcomes of such patients in the current era comes from these programs. Such programs also provide an opportunity for educating health care personnel in the management of IF (64.).
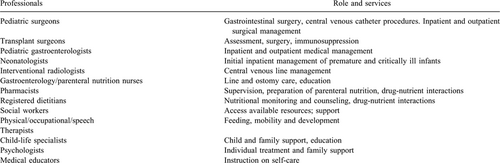
In reports describing the pediatric IR programs, almost all include pediatric surgeons (and transplant surgeons in transplant programs), pediatric gastroenterologists, specialized nurses (including advanced practice nurses), and dietitians (5., 14., 45.) (Table 2). Many include social workers, pharmacists, and 1 or more have included therapists (occupational/physical) and child life specialists, experts in palliative care or psychologists, interventional radiologists, and medical educators (6.). NASPGHAN recommends that at minimum staffing for an IR program includes a gastroenterologist, surgeon, dietitian (or registered dietitian-nutritionist), and a nurse. Close collaboration with neonatologists is strongly recommended. The presence of other specialists may be helpful: social workers, child psychologists, occupational therapists/physical therapists, speech/feeding therapists, interventional radiologists, and child-life specialists. Claimed advantages of care provided by such programs include the integration of care by multiple specialists, more discussion of patient management by involved specialists, communication of the individualized plan by the entire team to the patient/family, continuity of care through the course of various treatments, close follow-up of outpatients, improved patient and family education, earlier treatment of complications and learning from the accumulated patient databases (9., 13., 15., 38., 43., 49.). The potential to ease the anxiety and uncertainty experienced by patients facing this diagnosis also exists (65.). Quality assurance and research collaboration among centers is also a goal of many of these programs, with some published results.
INTESTINAL REHABILITATION PROGRAM EXPERIENCE
Over a dozen descriptions of IR programs that provide care for pediatric patients with IF are published, including 19 to 389 cases in each (9., 13., 15., 16., 41., 43., 45., 48., 51., 64., 66.-71.). The time period covered by these reports ranges from 1974 to 2015. Additional publications have provided recommendations/guidance on the long-term care of such patients or details on establishing an IR Program. Multiple programs have provided details on their pediatric patient population and outcomes (7., 9., 15., 16., 43., 45., 48., 49., 51., 60., 66., 68., 72.). Three networks or consortiums have contributed data on their experience (6., 69., 73.), and another focused on risk factors for poor outcome (41.). Most reports have not been limited to SBS, but include all pediatric patients with IF. In all but 1 report on a home PN population (48.), the majority of patients reported, however, had SBS, and that was true in that center as well, after exclusion of patients with non-gastrointestinal illnesses.
Successful weaning from PN occurred in 12% to 83% of patients. Transplantation rates, where reported, ranged from 0 to 31% (not including the patients with non- gastrointestinal illness in a single report) (48.). Mortality during the variable periods of follow-up ranged from 0 to 33%. In the consortium report, enteral autonomy was achieved by about half the patients. A quarter of them did not survive and a quarter came to intestinal transplantation. The reporting period for this study ended at the time when pediatric patients with IF coming to intestinal transplant peaked; the number of intestinal transplants has decreased subsequently, presumably reflecting improved outcomes. Avitzur et al (60.) have documented dramatically improved mortality and decreased need for transplantation in patients with IF referred for transplantation from 1999 to 2009 with the implementation of formal IR and other care changes during this interval.
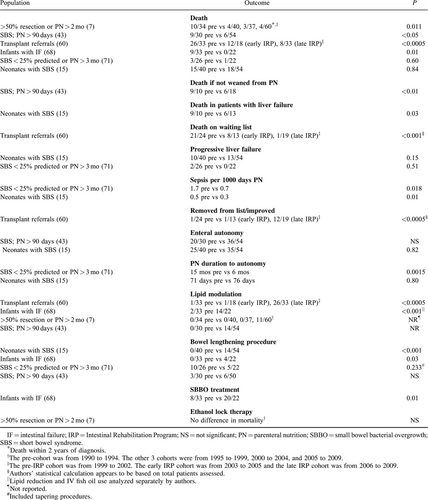
In a single-center study, 4 time cohorts were reported and the 3 most recent cohorts had notably improved survival (7.). The only factor identified distinguishing the first and other periods was the implementation of an IR program after the first cohort. Five valuable studies (3 from 1 center) included a retrospective group of patients to compare outcomes on patients treated before and after establishing IR programs, or a more comprehensive program (7., 15., 43., 60., 68., 71., 74., 75.) (Table 3). In another study, 54 SBS patients seen after establishment of the IR program in 2002 were compared to 40 retrospective partially matched controls. In general, outcomes were not different between groups for most complications, including liver failure and mortality (15.). Septic episodes per month were, however, reduced after establishment of the IR program (15.). There were also far more STEP procedures performed and a higher percentage of listed patients were transplanted (15., 60.). Mortality in those with liver failure was significantly reduced. In a more recent analysis from that center, time-series analysis indicated key factors for reducing mortality were advent of the IR Program and introduction of omega-3 lipids (74.). In a third study, 54 patients seen after establishment of the IR program in 1999 were compared to 30 patients seen in the 12 preceding years (43.). The 2 study groups appeared reasonably well-matched. Survival in the post-IR era was significantly better (89% vs 70%) and significantly more patients who were not weaned from PN survived (67% vs 10%). In the post-IR cohort, all patients who were weaned from PN survived after a mean follow-up period of a little over a year. In a Canadian study, 33 patients managed before formation of the IR program were compared with 31 after its formation in 2006 (75.). The 2 cohorts were reasonably well-matched. Mortality was significantly reduced (to zero). Differences in the management of the 2 cohorts after initiation of their IR program included more frequent treatment of bacterial overgrowth, implementation of lipid reduction/fish oil-based lipids and more STEP procedures. In a report from Finland, catheter care was improved and lipid therapy modulation standardized for the later cohort (71.). Bacteremia rates and PN duration until enteral autonomy both decreased significantly. Although differences for multiple other outcomes were statistically non-significant, 95% of the later cohort (21/22) survived, none developed progressive IFALD and no patient was transplanted. A general weakness of these studies is that they generally encompassed a fairly broad time span where the overall care of these patients improved. While it could be argued that improvements in care would have improved survival regardless of the formation of IR programs, a counter argument is that the improvement in care was the result of the formation of IR programs, which focused on the care of these patients.
The studies that have reported outcomes of IR programs is shown in Table 3. Most of the studies used a pre-/post model to assess improvement in outcomes. Two studies used several cohorts spanning different periods to further delve into outcomes (7., 60.). These studies have reported on negative outcomes (death, sepsis, and liver failure), positive outcomes (removal from intestinal transplantation listing, enteral autonomy, and duration to enteral autonomy), as well as interventions to improve outcomes (lipid modulation, bowel lengthening procedures, treatment for small bowel bacterial overgrowth, and ethanol lock therapy).
Stanger et al (76.) recently performed a systematic review and meta-analysis of the efficacy of IR programs. They identified reports of IR programs from 13 centers, with the 3 reports containing retrospective comparison groups noted above. They concluded from their analysis of the studies with comparison groups that IR programs were associated with increased survival from IF and overall survival. Any impact on achieving enteral autonomy and reduction of liver failure did not reach significance in the pooled data, but the reduction in liver failure was significant in 2 of the studies. A recent clinical guideline from the American Society for Parenteral and Enteral Nutrition (ASPEN) on support of pediatric patients with intestinal failure at risk of IFALD relied heavily on the Stanger analysis in answering the clinical question as to whether liver disease outcomes are improved by referral to IR programs (77.). They made a “weak” recommendation to refer patients to such programs and concluded that the evidence to support this recommendation is of “very low” quality. However they found “… the improvement in survival is compelling ….”
IMPACT OF NOVEL LIPID THERAPY
IR centers have served to advance therapies that have become standard of care in the field. Innovations in the management of the intravenous (IV) lipid component of PN were largely conceptualized and practiced within IR programs and are now widely practiced by most practitioners who care for patients with IF. Novel approaches to prevent and treat IFALD have included IV lipid restriction, sole use of IV fish oil-based lipid emulsion, IV fish oil-based lipid emulsion in combination with IV soybean oil-based lipid emulsion, IV lipid emulsion blends containing fish oil, and enteral fish oil. For each of these approaches, case series suggest that cholestasis can be reversed and its progression halted and 2 meta-analyses suggesting fish oil-based lipid emulsion or lipid emulsion blends containing fish oil may reduce bilirubin levels (78., 79.). Lipid emulsion blends without fish oil have not been found to be effective in reducing cholestasis (75.). Cober et al (80., 81.) demonstrated the potential role of lipid restriction and the associated risk of essential fatty acid deficiency and have noted the potential for poor growth. Most case series are regarding patients who have been treated with IV fish oil-based lipid emulsion. In their case series of patients treated with IV fish oil-based lipid emulsion, Diamond et al (82.) discussed the impact of this innovation on the course of SBS complicated by cholestatic liver disease, “Parenteral omega-3 fatty acids have the potential to fundamentally alter the paradigm of neonatal SBS from one of early death or transplantation from liver failure to a more chronic disease.” Similar experience was reported in 1 other study (68.). In the Boston experience, 86% of patients cleared their cholestasis. Those who did not respond were characterized by lower mean birth weight (1020 vs 1608 g), increased age at IV fish oil initiation (20.4 vs 11.7 weeks), and more advanced liver disease (83.). Concerns remain that benefits of intravenous fish oil on liver histology may be far less than the improvement in liver biochemistries and the significance of this issue and its implication for appropriate lipid modification are not yet clear (62., 84.). Some survivors have evidence of persistent liver fibrosis. Nevertheless, 2014 United Network for Organ Sharing data showed that the overall number of transplants in this population dropped since 2007 (85.). In the United States, fish-oil based lipid emulsion, however, remains unapproved by the US Food and Drug Administration and must be prescribed under investigational or compassionate use protocols, which limit its use. Use of an intravenous oil blend containing 15% fish oil has been reported in infants with early cholestasis with encouraging results (86.). This lipid product is approved for use in adults in North America. Another approach has been the use of enteral fish oil in those patients tolerant of some enteral feedings, but the supporting data are anecdotal at this stage (87., 88.).
SUMMARY AND RECOMMENDATIONS
Management of patients with IF by IR programs is the current state of the art, with limited but highly encouraging, supporting data on their medical efficacy, especially since the introduction of the use of novel lipids. The concept is highly attractive and intuitive, given the complexity of these patients, the number of medical professionals involved in their care and the need to systematically track outcomes in patients who are high utilizers of health care. While outcomes are expected to improve implicitly from experienced IR programs, data are still lacking on whether IR programs reduce health care costs for patients, insurers, hospitals or health systems.
NASPGHAN recommends the following:
- that reference values based on the child's height (preferably), weight or age be used as the standard for expressing the percentage of small bowel that remains.
- a definition of intestinal failure as the need for PN for >60 days due to intestinal disease, dysfunction or resection. The recommended definition of SBS is the need for PN for >60 days after intestinal resection or a bowel length of <25% of expected. It is further recommended that patients who meet 1 or both of these criteria have access to an Intestinal Rehabilitation Program for consultation or clinical management.
- patients with SBS not making progress toward enteral autonomy and continuing on PN >3 months, those with high clinical complexity or with worsening or non-resolving IFALD, recurrent sepsis, deep vein thrombosis or loss of venous access be referred to an IR program for consultation or management.
- at minimum staffing for an IR program include a gastroenterologist, surgeon, dietitian (or registered dietitian-nutritionist), and a nurse. Close collaboration with neonatologists is strongly recommended. The presence of other specialists may be helpful: social workers, child psychologists, occupational therapists/physical therapists, speech/feeding therapists, interventional radiologists, and child-life specialists.
Finally, NASPGHAN endorses management of patients with IF by, or in consultation with, centers with IR programs and encourages further research on the medical efficacy, patient satisfaction and quality of life, and financial impact of IR programs.