Serum Lipid Profile, Prevalence of Dyslipidaemia, and Associated Risk Factors Among Northern Mexican Adolescents
The study was supported by Department of Health, Government of the State of Nuevo león (Mexico), State Survey of Nutrition and Health–Nuevo León 2011/2012 (EESN-NL 2011/2012) and Spanish Ministry of Health and Consumer Affairs (Programme for Promotion of Biomedical Research and Health Sciences, Projects 11/01791, 14/00636, Red Predimed-RETIC RD06/0045/1004, and CIBEROBN CB12/03/30038). Grant of support was provided by 35/2011 (Balearic Islands Gov.) and EU FEDER funds.
The authors report no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.jpgn.org).
ABSTRACT
Background:
The increase in overweight and obese children and adolescents may be linked to increased rates of dyslipidaemia. The aim was to assess the serum lipid profile, the prevalence of dyslipidaemia, and associated risk factors among the North Mexican adolescent population.
Methods:
Two hundred and ninety-three subjects (47.8% girls) ages 11 to 16 years took part in the Nuevo León State Survey of Nutrition and Health 2011–2012. According to the 2011 Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents, dyslipidaemia was defined as a presence of ≥1 of the following levels (mg/dL): Total cholesterol ≥200, low-density lipoprotein cholesterol ≥130, non–high-density lipoprotein cholesterol <40, and triglyceride ≥130.
Results:
The overall frequency of dyslipidaemia was 48.8% with no differences between sexes. Adolescents with high body mass index were more likely to have at least 1 abnormal lipid level (overweight: odds ratio [OR]: 2.07; 95% confidence interval [CI]: 1.14–3.77, P < 0.05; obesity: OR: 2.21, 95% CI: 1.11–4.41, P < 0.05) than those with normal weight. Abdominally subjects with obesity were also more likely to have at least 1 abnormal lipid level (OR: 2.30; 95% CI: 1.35–3.91, P < 0.01) than their leaner counterparts.
Conclusions:
Half of Mexican adolescents living in the State of Nuevo León have at least 1 abnormal lipid concentration. Low HDL-chol level was the most common dyslipidaemia. Body mass index and abdominal obesity were associated with the prevalence of at least 1 abnormal lipid level.
What Is Known
- Obesity is associated with dyslipidaemia.
- In Mexico, 35% of adolescents are overweight or obese, and this figure has increased by about 5% since 2006.
- The 2011 Expert Panel on Integrated Guidelines for Cardiovascular Risk Reduction has endorsed universal lipid screening of children and adolescents to identify dyslipidaemias at early age.
What Is New
- Half of the adolescents living in the State of Nuevo León, Mexico have at least 1 abnormal lipid concentration.
- Low high-density lipoprotein-cholesterol level is the most prevalent dyslipidaemia among Northern Mexican adolescents.
- Body mass index and abdominal obesity were associated with the prevalence of at least 1 abnormal lipid level.
Dyslipidaemias are abnormal amounts of lipid and/or lipoprotein in the blood that may be related to other diseases, with obesity being the most common, which is typically associated with a combined dyslipidaemia pattern with mild elevation in total cholesterol (TChol) and low-density lipoprotein cholesterol (LDL-chol), moderate to severe elevation in triglycerides (TG), and low high-density lipoprotein cholesterol (HDL-chol) (1.-3.). In Mexico, 35% of adolescents are overweight or obese according to the National Health and Nutrition Survey of Mexico (ENSANUT-2012), and this figure has increased by about 5% since 2006 (4.).
The 2011 Expert Panel on Integrated Guidelines for Cardiovascular Risk Reduction on lipid screening in childhood and adolescence (5.) has endorsed universal screening of all children and adolescents to identify dyslipidaemias at an early age. This recommendation is different from other guidelines (6.-8.), in which screening children older than 2 years is recommended if they have cardiovascular risk factors, have a family history of premature cardiovascular disease (CVD) or dyslipidaemia, are overweight or obese, have other elements of insulin resistance syndrome, or have no available family history. Significant evidence, however, exist that using family history of premature CVD or of cholesterol disorders as the primary factor in determining lipid screening for children misses approximately 30% to 60% of children with dyslipidaemias, in whom accurate and reliable measures of family history are not available (5.). Moreover, several studies have shown that in ~50% of children with high lipid and lipoprotein levels, abnormal levels will persist over time (9.-12.). Children's adverse serum lipid levels predict dyslipidaemia in adulthood and adverse levels of non–HDL-chol also are related to non–lipid cardiovascular risk factors in adulthood (13.).
In the present study we aimed to assess the serum lipid profile, the prevalence of dyslipidaemia, and associated risk factors among North Mexican adolescent population.
METHODS
Study Design, Sample Selection, Recruitment, and Approval
The present study was a population-based cross-sectional nutritional survey part of the State Survey of Nutrition and Health–Nuevo León, Mexico, 2011/2012 (EESN-NL 2011/2012), designed by the National Institute of Statistics and Geography (INEGI) to obtain information on the health and nutritional status of the state population (n = 4,653,458; 84.5% residing within the Monterrey Metropolitan area; 94% occupying urban areas). The state was divided into 4 geographical regions (percentage of urban vs rural population): northern (66.1% vs 33.9%), central (72.9% vs 27.1%), southern (15.3% vs 84.7%), and the metropolitan area (89.8% vs 10.2%); globally: 61.0% versus 39.0% (14., 15.). For the entire survey, a target of 1059 households per region was assessed using the household as the sampling unit and an average of 2 interviews per household; however, for biochemical measurements a sample size of 640 households was considered sufficient to detect risk factors with 95% confidence and a precision rate of 10% and a nonresponse rate of 40%. In the present study, inclusion criteria were to be an inhabitant censused in the State of Nuevo León and provided fasting blood sample. The analysis was also limited to 11- to 16-year-old adolescent participants who provided a fasting blood test (n = 351; 49.0% girls). Two participants in the same age group living in the same household were not selected. Missing data for lipid profile were found in 6 subjects. Moreover, anthropometric measurements (weight and height) were not available in 43 participants. Pregnant girls (n = 7) or breastfeeding girls (n = 2) were also excluded leaving an analysis sample of 293 (47.8% girls). The study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects were approved by the Scientific Technical Committee of the Public Health and Nutrition Faculty at the Autonomous University of Nuevo, León. Informed written consent was obtained from all subjects and also from the next of kin, carers, or guardians of the minors involved in the study.
Anthropometric Measurements
Height was measured to the nearest millimetre using a mobile stadiometer (SECA 213, Birmingham, UK), with the subject's head in the Frankfurt plane. Body weight was determined to the nearest 100 g using a digital scale (Seca 813, Hamburg, Germany). Waist circumference (WC) was measured to the nearest 0.1 cm using a nonstretch measuring tape (Gulik, Lafayette Instrument Co, Lafayette, IN). Height and weight measures were used to calculate body mass index (BMI; kg/m2) and WC and height were used to calculate waist-to-height ratio (WHtR).
Overweight and Obesity Definition
Overweight and obesity were determined based on age- and sex-specific BMI cut-offs developed and proposed for international comparisons by Cole et al (16.), also recommended for use by the International Obesity Task Force.
Abdominal Obesity Definition
A WHtR cut-off of 0.5 was used to define abdominal obesity for both boys and girls (17.).
Biochemical Measurements
Venous blood samples were obtained from the antecubital vein in suitable vacutainers after a 12-hour overnight fast. Serum TG, TChol, HDL-chol, and LDL-chol were determined using the Cobas 6000 analyser series (F. Hoffmann-La Roche Ltd, Basel, Switzerland), by “Dr. Bernardo Sepúlveda” laboratory at the Metropolitan Hospital under the Ministry of Health of Nuevo León, Mexico. Non–HDL-chol was calculated as TChol minus HDL-chol.
Definitions for Adverse Serum Lipid Levels and Dyslipidaemia
According to the 2011 Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents (5.), serum lipid levels were categorized into 3 subgroups (acceptable, borderline, or high) as follows: TChol (mg/dL): acceptable <170, borderline 170–199, high ≥200; LDL-chol (mg/dL): acceptable <110, borderline 110–129, high ≥130; non–HDL-chol (mg/dL): acceptable <120, borderline 120–144, high ≥145; HDL-chol (mg/dL): acceptable >45, borderline 40–45, low <40; TG (mg/dL): acceptable <90, borderline 90–129, high ≥130.
Dyslipidaemia was defined as the presence of 1 or more of the following conditions: TChol ≥200 mg/dL, LDL-chol ≥130 mg/dL, non–HDL-chol ≥145 mg/dL, HDL-chol <40 mg/dL, TG ≥130 mg/dL (15.).
Statistical Analysis
Analyses were performed with the SPSS statistical software package version 21.0 (SPSS Inc., Chicago, IL). Level of significance for acceptance was P < 0.05. Significant differences in prevalence were calculated by means of χ2 test. Differences between group means were tested by Mann-Whitney U test. Univariate binary logistic regression analyses were used to assess the association between age group, sex, and anthropometric indicators (independent variables) and dyslipidaemia (dependent variable).
RESULTS
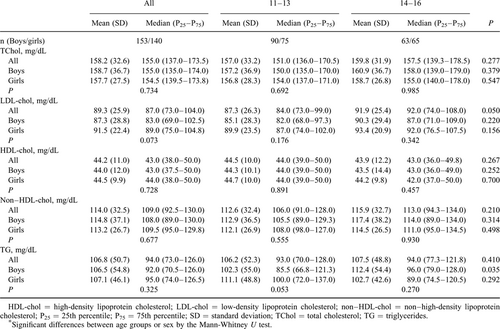
Table 1 shows the lipid serum and lipoprotein levels of the participants. There were no significant differences in lipid serum levels between sex and age groups (except for TG levels in boys).
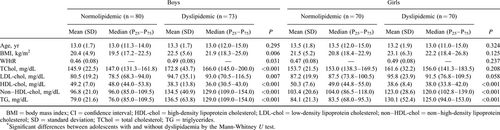
The overall prevalence of dyslipidaemia was 48.8%, with no differences between sexes. They have at least 1 abnormal lipid concentration, and low HDL-chol followed by high TG were the most common dyslipidaemias. The association of age, anthropometric variables (BMI and WHtR), and serum lipid and lipoprotein levels (TChol, LDL-chol, non–HDL-chol, HDL-chol, and TG) among adolescents with or without dyslipidaemia was also evaluated (Table 2). No differences in age means were obtained. Boys with dyslipidaemia showed higher BMI and WHtR than their normolipidaemic counterparts, whereas no differences in anthropometric variables were found among girls. Boys with dyslipidaemia also showed lower values for HDL-chol levels and higher values for all other parameters than normolipidaemic participants.
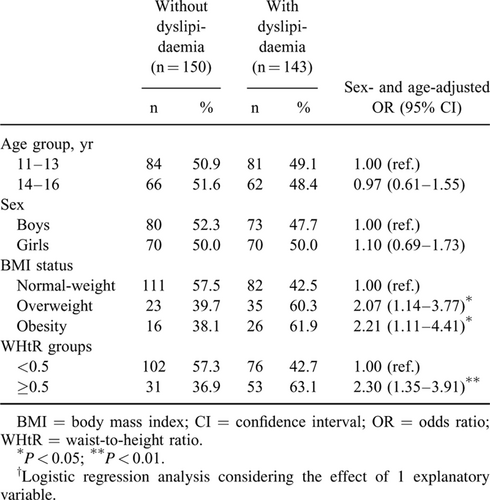
The logistic regression analysis with anthropometric variables (Table 3) showed that the risk of dyslipidaemia was associated with BMI status and abdominal obesity after adjustment for sex and age. Adolescents with high BMI were more likely to have at least 1 abnormal lipid level (overweight: odds ratio [OR]: 2.07; 95% confidence interval [CI]: 1.14–3.77, P < 0.05; obesity: OR: 2.21, 95% CI: 1.11–4.41, P < 0.05) than those with normal-weight. Abdominally obese subjects were also more likely to have at least 1 abnormal lipid level (OR: 2.30; 95% CI: 1.35–3.91, P < 0.01) than their leaner counterparts. None of the other variables considered in the present study (age and sex) were significantly associated with dyslipidaemia.
Prevalence of risk categories for lipid serum and lipoprotein levels, and dyslipidaemia components among adolescents are shown in Supplemental Digital Content, Tables 1 and 2, http://links.lww.com/MPG/A732.
DISCUSSION
The main finding of the present study is that half of the Nuevo León adolescents have at least 1 abnormal lipid concentration. Alterations in lipid profile have also been registered in more than half of the paediatric populations of Latin America (18.-20.). Despite differences in studied ages and the cut-off values for serum lipid level, which hampered direct comparison across studies, this prevalence of dyslipidaemia is higher than that in the previous studies in Brazil (21.), Mexico City (22.), and the United States (23.).
According to previous studies conducted in Mexico City (22., 24., 25.), low HDL-chol level followed by high TG levels were the most prevalent dyslipidaemias, and were related to BMI. In other countries, high TG levels were followed by low HDL-chol and high TChol levels (20., 25.-27.). High TChol prevalence was similar to previously reported data (28., 29.), but higher than that in the previous studies (22., 24.-26., 30.). High LDL-chol levels were the least frequent dyslipidaemia and closely similar to previously reported data in Mexico City (22., 24.), and in non–Latin American countries (29., 31.), but higher (25.) and lower (27.) than that in Latin American and Asian countries, respectively.
Similar to Brazilian adolescents (19.), there were no sex differences in lipid concentrations among Nuevo León adolescents. Several studies, however, found higher levels for TChol, LDL-chol, HDL-chol, and TG (25., 26., 28., 32.-34.), and lower prevalence of high LDL-chol levels (34.), and low HDL-chol levels in girls than in boys (25., 26., 28.). In Mexico City, low HDL-chol was more frequently found among boys than girls (22., 24.), but women showed higher TChol, LDL-chol, and TG levels (25., 26., 28., 32.-35.) but lower ultimate CVD risk than men (35., 36.).
Obesity is associated with increased rates of dyslipidaemia and other CVD risk factors (37.). Higher values of TChol, LDL-chol, and TG (22., 24., 38.), non–HDL-chol (39.), and lower of HDL-chol (22., 24.) have been found among overweight and/or obese adolescents than in normal-weight adolescents. In our study, adolescents with abdominal obesity were twice as likely to have at least 1 abnormal lipid level. Previously, WC has been positively associated with LDL-chol (22.), TG (19., 22., 40.), and non–HDL-c (39.), and negatively associated with HDL-chol (22., 40.). Waist-to-hip ratio has been also correlated to HDL-chol and TG (40.) and WHtR correlated to TG and non–HDL-chol in adolescents (19.). These findings agree with previous studies showing that WC is correlated with an abnormal lipid profile in teenagers (22., 40.), and with a previous work which reported that WC is more closely associated with dyslipidaemia in children and adolescents than does BMI, which is more closely related to hypertension (41.).
Dyslipidaemia is a modifiable CVD risk factor. The first step proposed to manage children and adolescents with elevated lipid levels is an intensive lifestyle modification, focused on normalizing body weight in patients with obesity, promoting a sensible diet, increasing levels of physical activity (5., 6., 35.), and the active smoking prevention. Multiple studies have shown the efficacy of weight reduction in improving lipoprotein levels in paediatric obesity (35.). The safety and effectiveness of the recommended diet for the general population is supported by large randomized trials. Increased physical activity has been associated with increased life expectancy and decreased risk of CVD (42.). Therefore, lifestyle intervention is vital in managing a disease process that eventually carries high morbidity and mortality (2.). Nevertheless, for individuals with familial hypercholesterolemia and high LDL-chol levels, healthy lifestyle behaviours are rarely enough to achieve lipid targets, and the expert panel set out specific steps for more intensive clinical management (43.).
Strengths and Limitations
The main strength of the present study includes confirmation of the high dyslipidaemia prevalence among the Mexican population, making it necessary to develop effective preventive measures. Early intervention to encourage appropriate nutrition and physical activity at early ages could be relevant strategies to prevent and/or reduce the high risk for atherosclerosis in this population. This article also has limitations. First, the cross-sectional study design decreased the ability to show causality compared with longitudinal studies. The complex basis that, however, addresses the beginning of CVD risk in childhood, and the absence of long event-driven clinical trials, demands to consider any consistent evidence from observational studies (43.). Second, data on the use of lipid-lowering medication are not available in EESN-NL 2011/2012 and therefore participants on lipid-lowering therapy were not excluded. Third, the guidelines do not account for variations in lipids due to race, sex, pubertal status (35.), and geography (5.), all of which are known to have a clinically relevant effect on lipoprotein values. Biological rhythms and seasonal variation in lipid profiles exist which should be particularly accounted for in cross-sectional analysis of relative risk, prevalence, or the rate of target achievement for lipid parameters (44.). Finally, the differences in the ages studied and the cut-off values for serum lipid level could hamper the direct comparison across the different studies.
CONCLUSIONS
Half of the Mexican adolescents living in the State of Nuevo León have at least 1 abnormal lipid concentration. A low HDL-chol level was the most common dyslipidaemia. BMI and abdominal obesity were associated with the prevalence of at least 1 abnormal lipid level.