Dysphagia after chemo-radiation for nasopharyngeal cancer: A scoping review
Abstract
Objective
Nasopharyngeal cancer (NPC) has distinct characteristics regarding its global prevalence, initial presentation, management and patient outcomes compared to other subtypes of head and neck cancer (HNC). The mainstay of NPC treatment is chemo-radiation (C/RT) and while dysphagia is a known early and late toxicity of C/RT treatment, the nature of dysphagia post NPC treatment has had limited investigation. The objective of this review is to summarise the existing evidence regarding dysphagia following NPC to inform the future research agenda for this population. Dysphagia incidence, characteristic deficits observed across the phases of swallowing, efficacy of current dysphagia interventions, and effect on quality of life will be explored.
Data sources
Databases including MEDLINE, CINAHL, Embase, Scopus and Web of Science were included.
Methods
A scoping review was conducted according to PRISMA-ScR guidelines. Two independent reviewers screened selected full text articles.
Results
Of the initial 2495 articles found, 28 articles were included. Reports of penetration and aspiration varied widely (0%–91.6%), with high rates of silent aspiration identified in 2 studies (42%, 66%). Oral, pharyngeal and upper esophageal phase impairments were reported. Of these, upper esophageal stasis and multiple pharyngeal stage deficits were most prevalent. The pharyngeal constrictors were found to have a significant dose–effect relationship and shielding to the anterior neck field was effective to preserve swallowing function. Six treatment studies were identified with limited evidence supporting the use of neuromuscular electrical stimulation, dilatation and swallowing exercises. Quality of life was adversely affected.
Conclusions
Dysphagia is a prevalent early and late problem post NPC treatment, with impairments across all phases of the swallow. Studies on preventing dysphagia and treatment efficacy remain limited. More systematic study of the nature of dysphagia and the efficacy of treatment in this population is warranted.
Introduction
Head and neck cancers (HNCs) are the ninth most common cancer in the world, with nasopharyngeal cancer (NPC) a subtype among them.1 NPC is a non-lymphomatous carcinoma that develops in the epithelial lining of the nasopharynx.2 It is unique in its highly specific regional distribution in the world, with the incidence of NPC the highest in the southern parts of China, followed by South East Asia and some artic areas in which Eskimos reside.3,4
The histology of the main subtype of NPC is non-keratinizing carcinomas. Compared with squamous cell carcinoma in other HNCs, they are more radiosensitive and respond better to radiation therapy (RT).2 Therefore, treatment differs from the general head and neck cancer population, with chemo-radiation therapy (C/RT) being the mainstay of treatment instead of surgery.2 Toxicities in patients who have undergone C/RT refer to the complications that they suffer from as a result of the treatment, as C/RT unavoidably affects structures adjacent to the tumor, impacting their corresponding functions. Toxicities post NPC tumor management are common and pose serious concern in the management of patients whose disease is in remission.5 Late toxicities post NPC differ from other types of head and neck cancers with endocrine and hormonal dysfunction, dental problems, hearing problems and central nervous system abnormalities frequently reported.3
An additional early and long-term consequence of NPC management is dysphagia (disordered swallowing).6 Although some studies have failed to identify dysphagia as a significant issue,7 others suggest high proportions of patients will experience swallow change long-term post NPC treatment.8-10 The specific nature of the deficits characterizing dysphagia post NPC also needs clarification. Limited numbers of studies, variability in the assessment approaches, and inconsistency in outcome measures used in the studies to date has limited the formation of a clear and comprehensive picture of presenting deficits across each stage of the swallow.
The physiological basis for these presenting swallowing deficits is also still unclear. The integrity of swallowing relies on normal function of the swallowing center in the brainstem, the key cranial nerves involved in the swallow, as well as normal function and integrity of the muscles and structures in the oral, pharyngeal and esophageal regions of the head and neck. NPC treatment has potential to impact many of these critical components – hence influencing the efficiency and safety of the normal swallow post treatment. For example, the cranial nerves that exit the skull base innervating the swallowing structures are at risk of being damaged by C/RT because their pathway is often encompassed within the radiation treatment field.11,12 Although the exact mechanism for this radiation-induced cranial nerve neuropathy is not fully understood,13 it is common in the NPC population, with lower cranial nerves usually more affected,14 creating potentially compromised swallow function.
The issue of muscle fibrosis as a contributing cause to dysphagia has also been investigated. Yeh et al12 found that 38.2% of the NPC patients in their large cohort study (n = 849) had fibrosis in at least one side of the neck post treatment. One of the factors found to be associated with fibrosis presence was a radiation dose of more than 62 Gy to the neck region, which is common in NPC management.12 Lin et al15 also confirmed the presence of fibrosis in the pharyngeal and laryngeal muscles of the patients in their cohort (n = 19) which was impacting hyoid bone anterior movement and upper esophageal sphincter relaxation.
While dysphagia post NPC is a recognized consequence of treatment, and there is emerging evidence that both cranial nerve function and fibrosis may be contributing factors, there is still much work needed to fully understand the prevalence and nature of dysphagia post NPC management. Variability in methodologies, and a limited numbers of papers specifically examining the issue of dysphagia in this population means that the evidence for core questions such as: (1) how prevalent dysphagia and related complications are among NPC patients; (2) whether dysphagia in this population has characteristic deficits across the phases of swallowing; (3) whether there is any collective evidence to effectively prevent and manage dysphagia in this population; (4) what are the effects on the dysphagia-related quality of life – are only just emerging. For this reason, the purpose of the current study was to conduct a scoping review to map the research done in this area, and to identify any issues and existing gaps in the knowledge base in order to inform an agenda for future research into dysphagia and its consequences post NPC treatment. At the time this review was conducted the body of evidence was limited, and no prior review specifically examining dysphagia post NPC had been conducted. Therefore, the objective of the review was to provide a broad overview of the current research in this area rather than answering a single specific question. For this reason, a scoping review was chosen over a systematic review, as it is the preferred method of revising an area where the topic has yet been extensively reviewed or the issues are heterogenous in nature.16
Methods
The scoping review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines.17
Search strategy and selection criteria
Primary searches (from inception to July 2019) were completed in MEDLINE, CINAHL, Embase, Scopus and Web of Science databases on 28th July 2019. The following keywords were used: “nasopharyngeal cancer or nasopharyngeal carcinoma” and “dysphagia or swallow or deglutition”. Additional search terms included “NPC”, “nasopharynx neoplasm”, “swallow dysfunction”, and “swallow disorder”. The reference lists of all identified studies were manually searched for additional relevant publications. The search incorporated only one filter, which was to eliminate all non-English articles. Studies sourced from electronic databases were imported into Endnote X9 (Clarivate Analytics), where duplicates were removed. The title and abstract screening and full-text review were completed in Endnote X9 (Clarivate Analytics).
Titles and abstracts were independently screened for eligibility for inclusion using pre-defined inclusion and exclusion criteria. Studies were included if: (1) participants were adults (i.e., 18+ years of age): with a diagnosis of NPC that was treated using C/RT; (2) dysphagia or swallow-related structures were investigated as post-treatment toxicities from C/RT; (3) studies reported in full-text journal articles; (4) studies reported in English. Animal studies, editorials, conference abstracts, opinion papers and studies utilizing case study designs were excluded. Two independent reviewers screened the selected full text articles.
Data extraction and synthesis
One author (RF) independently extracted descriptive data regarding sample size, study type, age and gender of participants, NPC classification, treatment type, dysphagia diagnosis, outcome measures used and the major findings. To explore accuracy, data extraction was independently repeated for a randomly selected 10% of all included articles by a second author (AR). The articles identified were then classified into: (1) studies on the prevalence of dysphagia and related complications; (2) studies with outcomes specifically for different phases of swallowing; (3) studies on the efficacy on the prevention and treatment of dysphagia; (4) studies on the dysphagia-related quality of life in this population. The results were compiled and a summary of findings in these four areas are discussed.
Results
Search, selection and methodological quality
A total of 2945 papers were identified from the database search of which 1150 were duplicates and were removed (Fig. 1). Titles and abstracts of 1795 articles were screened, with 39 deemed appropriate for full text review. After full text review, 28 studies were deemed suitable for inclusion and data extracted.
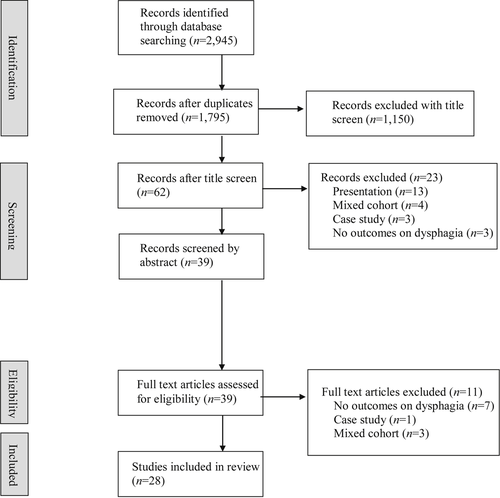
PRISMA flow diagram of search strategy and selection criteria.
The methodological quality of all included studies was evaluated using the Mixed Methods Appraisal Tool (MMAT).18 MMAT is a critical appraisal tool that was designed to appraise the quality of quantitative, qualitative and mixed methods studies. Considering the range of studies included in this review, this appraisal tool system was deemed appropriate to assess the quality of the included studies, despite their different methodologies. One of the authors (RF) first answered two screening questions, then after categorizing the study, five questions were answered regarding the corresponding study design. The article was considered of higher methodological quality with more affirmative answers across the questions. The average MMAT score was 3.82 (range 2–5) out of 5.
The majority of the 28 studies (n = 11, 39.3%) used a cross-sectional design to investigate swallowing function or specific physiological events of swallowing,7-10,19-25 while only two (7.1%) adopted a longitudinal design that investigated the swallowing function at different time-points.26,27 Six articles (21.4%) investigated the outcome of swallowing treatment,15,28-32 while 4 (14.3%) investigated or compared the effects of RT techniques on swallowing outcomes.33-36 Only two (7.1%) specifically investigated the related complications of dysphagia,37,38 while three (10.7%) investigated the impact on quality of life by dysphagia in NPC patients.39-41 Key information relating to each of the 28 studies was reviewed and information extracted regarding: (1) prevalence and characteristic deficits across the phases of swallowing (n = 15, Table 1); (2) evidence for prevention and treatment (n = 10, Table 2); (3) studies relating to impacts to dysphagia-related quality of life (n = 3, Table 3).
| Author | Sample size (gender) | Age (years, Mean ± SD) | Tumour staging of participants | Treatment techniques (n) | Main objectives | Outcome measures | Main findings | MMAT quality rating |
|---|---|---|---|---|---|---|---|---|
| Chang et al20 | 12 (1F:11M) and 12 age-matched controls | 45.42 | Stage Ⅱ – 1; Stage Ⅲ – 4; Stage Ⅳ – 7 |
RT (12); Induction chemotherapy (10); Concurrent chemotherapy (11) | Evaluate the effects of RT on tongue function | IOPI | No difference of tongue function compared with normal pre- and post-RT; decreases in tongue function may not start until 2 months post-RT | 4/5 |
| Chang et al8 | 184 (47F:137M) | 48.3 ± 11.6 | Stage Ⅰ – 24; Stage Ⅱ – 45; Stage Ⅲ – 41; Stage Ⅳ – 71 |
60Co (46); Linear accelerator (138); Neoadjuvant chemotherapy (23);Combination of radiosensitizer (45) | Evaluate swallowing status and the factors influencing swallowing | VFSS and interview of participants for clinical symptoms | Swallowing abnormalities were noted in both acute and chronic groups. Swallowing function continues to deteriorate over time, even many years after RT | 5/5 |
| Chang et al27 | 76 (19F:57M) | 47.9 ± 10.7 | Stage Ⅰ – 4; Stage Ⅱ – 9; Stage Ⅲ – 21; Stage Ⅳ – 42 |
2D RT (68); 3D-RT (8); Induction chemotherapy (55); Concurrent chemotherapy (65) | Evaluate over a 2-year period the serial swallowing function NPC patients post-RT | VFSS and purpose-built questionnaire rating clinical swallowing performance | At 2 years, patients had a progressively increasing pharyngeal transit time. Dysphagia symptoms subjectively identified decreased after the first month post RT | 4/5 |
| Cheng et al24 | 40 (9F:31M) | 53.9 | Stage Ⅰ – 9; Stage Ⅱ – 11; Stage Ⅲ – 12; Stage Ⅳ – 8 |
2D-RT (18); IMRT (22); Chemotherapy (20) | Assess the relationship between suprahyoid muscle contraction, hyoid bone displacement, and penetration-aspiration status | Ultrasound and VFSS | Anterior hyoid displacement and pharyngeal constriction ratio were significantly associated with penetration-aspiration | 4/5 |
| Fong et al10 | 134 (43F:91M) | 63.0 ± 11 | T1-T2 – 48, T3-T4 -46; N0–N1 – 54, N2-3 – 40 |
Chemotherapy (90) | Investigate the prevalence and associated factors of cervical esophageal clearance issues | VFSS | Esophageal clearance issues are highly prevalent and may co-exist with more severe oral/pharyngeal deficits | 4/5 |
| Hughes et al19 | 50 (11F:39M) | 49 | Not available | RT only (50) | Investigate the prevalence of long-term dysphagia in patients treated forNPC | Questionnaire, Clinical assessment, VFSS | Both Subjective and objective swallowing abnormalities are common after RT for NPC | 4/5 |
| Ku et al21 | 100 (32F:68M) | 58 | Stage Ⅰ – 8; Stage Ⅱ – 25; Stage Ⅲ – 35; Stage Ⅳ – 13 |
RT only (100) | Investigate the laryngopharyngeal sensory deficits and aspiration | FEESST | Impaired pharyngeal contraction are more significantly related to aspiration than laryngopharyngeal sensory deficits | 4/5 |
| Ku et al26 | 20 (6F:14M) | 43.9 | Stage Ⅰ-Ⅱ – 9; Stage Ⅲ-Ⅳ – 11 |
RT (20); Boost dose for parapharyngeal extension (17); Concurrent chemotherapy (11) | Study the incidence and the degree of swallowing dysfunction in patients with NPC after RT | Self-rated questionnaire; VFSS | Swallowing problems persisted after 12 months of RT, predominantly having problems with pharyngeal stasis | 3/5 |
| Ng et al23 | 85 (23F:63M) | 56.8 ± 10.9 | Not available | Not available | Establish silent aspiration occurrence, safe bolus consistency, and their relationship with swallowing physiology in NPC patients post-RT | FEES | Silent aspiration of thin fluids is a common occurrence in dysphagic NPC post-RT, with least aspiration noted on soft diet | 5/5 |
| Patterson et al7 | 18 (4F:14M) | 52.5 ± 13.06 | T1-T2 – 11, T3-T4 – 7; N0–N1 – 12, N2–N3 – 6 |
RT only (5); Concurrent C/RT (13); Neoadjuvant chemotherapy (2) | Evaluate swallowing function in NPC patients with IMRT done | FEES and clinical assessment AusTOMs Oral health-related QoL |
Characterised by bolus residue and delay, but no aspiration. Dysphagia was of mild or moderate severity on all measures | 2/5 |
| Phua et al25 | 18 (7F:11M) | 57.3 ± 8.1 | Not available | RT only (18) | Examine the effects of RT on dysphagia and dysphagia rehabilitation | Clinical assessment and VFSS | Non-oral feeding was needed in over half of the participants and following intervention, half of them could resume oral feeding | 2/5 |
| Wang et al22 | 33 (8F:25M) and 10 controls | 55.5 ± 8.8 | Stage Ⅰ – 3; Stage Ⅱ – 4; Stage Ⅲ – 11; Stage Ⅳ – 15 |
RT only (33) | Quantitatively assess the movement of the hyoid bone and pyriform sinus stasis | VFSS | NPC patients experienced a reduction in hyoid bone displacement, occurring in a forward direction. The displacement of the hyoid bone was less in the aspiration subjects than in those without aspiration | 4/5 |
| Xiong et al38 | 217 (55F:162M) | 56 | Stage Ⅰ – 22; Stage Ⅱ – 67; Stage Ⅲ – 74; Stage Ⅳ – 54 |
RT only (84); C/RT (133) | Identify patients with NPC at risk of developing SRCIs | Retrospective chart review | Swallowing-related chest infection is common in NPC patients. Advanced age, C/RT and recurrent cancer were strong risk factors for NPC patients with RT done to develop SRCIs | 4/5 |
| Yen et al37 | 3818 (970F:2844M) | 49.2 ± 12.4 | Not available | RT only (533); C/RT (3,281); Single RT (3,285), 2nd course of RT (529) | Assess the incidence of late-onset pneumonia | Retrospective chart review | Late-onset pneumonia is not uncommon in patients with NPC after radiotherapy | 4/5 |
- NPC: nasopharyngeal cancer; MMAT: Mixed Methods Appraisal Tool; RT: radiation therapy; IOPI: Iowa Oral Performance Instrument; VFSS: videofluoroscopic swallowing study; IMRT: Intensity modulated radiation therapy; FEES: fiberoptic endoscopic evaluation of swallowing; C/RT: chemo-radiation therapy; QoL: quality of life; SRCIs: swallowing-related chest infections.
| Author | Sample size (gender) | Age (years, Mean ± SD) | Tumour staging of participants | Treatment techniques (n) | Main objectives | Outcome measures | Main findings | MMAT quality rating |
|---|---|---|---|---|---|---|---|---|
| Prevention of dysphagia | ||||||||
| Cetin et al33 | 20 (5F:15M) | 3D conformal – 43.1; IMRT – 43.8 | Stage Ⅰ – 1; Stage Ⅱ – 7; Stage Ⅲ – 12 |
3D Conformal RT (10); IMRT (10) | Compare the effects of 3D conformal RT with IMRT on swallowing function | FEES and Self-rating of symptoms | No difference between 3D conformal RT and IMRT in the swallowing outcome | 3/5 |
| Fua et al34 | 28 (7F:21M) | 50.0 | Stage Ⅰ – 1; Stage Ⅱ – 5; Stage Ⅲ – 14; Stage Ⅳ – 8 |
Whole-field IMRT (20); IMRT with central shielding (8); Induction chemotherapy (21); Concurrent chemotherapy (23) | Quantify the dose delivered to the pharyngo–esophageal axis usingIMRT techniques and correlate with swallowing toxicity | Clinical assessment; feeding tube placement duration | Central shielding was effective in reducing acute RT toxicity of dysphagia | 4/5 |
| Jiang et al36 | 134 (33F:101M) | 44 | T1-T2 – 37, T3-T4 – 97; N0–N1 – 59, N2–N3 – 75 |
IMRT (134); Neoadjuvant chemotherapy (48); Concurrent chemotherapy (108) | Investigate the dose-volume effect on the swallowing function | Dose-volume histogram and RTOG/EORTC scale score and MDADI | Significant relationship between dysphagia and radiation doses to the superior and inferior constrictor muscles | 4/5 |
| Messer et al35 | 72 (15F:57M) | 52 ± 12 | T1-T2 – 29, T3-T4 – 39; N0–N1 – 28, N2–N3 – 39 |
IMRT (72); Induction chemotherapy (49); Concurrent chemotherapy (63) | Characterize the changes in the MRI signal intensity in dysphagia-associated structures as a function of RT | Signal intensity of MRI | Dose dependent decrease in the late T1 signal intensity is associated with higher RT doses to the superior pharyngeal constrictor muscle | 5/5 |
| Treatment of dysphagia | ||||||||
| Fong et al32 | 13 (2F:11M) | 42.0 | T1 – 1, T2-T3 – 10; N0–N1 – 8, N2 – 3 |
RT (9); C/RT (4) | Determine the use of balloon dilation for treating cricopharyngeal dysfunction | VFSS and MDADI | Balloon dilation was effective in treating dysphagia, reduce aspiration risk and improve quality of life | 4/5 |
| Lei et al31 | 9 (9M) | 62.5 | Not available | RT only (9) | Study the effect of modified laryngotracheal separation on patients with intractable aspiration pneumonia | Incidence of pneumonia, weight, nutritional status | Modified laryngotracheal separation is effective in eliminating intractable aspiration pneumonia. Careful patient selection is required | 3/5 |
| Lin et al15 | 20 (8F:12M) | Electrical stim group – 52.3; Exercise group – 56.1 | Stage Ⅱ – 3; Stage Ⅲ – 10; Stage Ⅳ – 6 |
Single RT (17); 2 courses of RT (3) | Assess the effectiveness of functional electrical stimulation on NPC patients | VFSS and QoL measures | Functional electrical stimulation was effective in improving swallowing function and its related quality of life | 4/5 |
| Long & Wu28 | 60 (31F:29M) | Treatment group – 56.5; Control group – 55.83 | Not available | RT (60) | Evaluate the therapeutic effect of (NMES and balloon dilation in NPC patients | Clinical assessment, VFSS | Combined NMES and balloon dilatation treatment were effective for improving swallowing function | 3/5 |
| Tang et al29 | 43 (11F:32M) | 49.3 ± 11.0 | Not available | RT only (43) | Evaluate the therapeutic effect of rehabilitation therapy on dysphagia and trismus in NPC patients | Clinical assessment of swallowing and jaw opening | Rehabilitation training can improve swallow function and slow down the progress of trismus in NPC patients | 3/5 |
| Wang et al30 | 12(3F:9M) | 52.58 ± 10.82 | Not available | RT only (12) | Evaluate the effect of cervical esophagostomy in NPC patients with severe dysphagia | QoL measures, incidence of pneumonia | Cervical esophagostomy can improve the life quality of patients with dysphagia induced by radiotherapy for nasopharyngeal carcinoma | 4/5 |
- NPC: nasopharyngeal cancer; MMAT: Mixed Methods Appraisal Tool; IMRT: intensity modulated radiation therapy; RT: radiation therapy; FEES: fiberoptic endoscopic evaluation of swallowing; RTOG: Radiation Therapy Oncology Group; EORTC: European Organization for Research and Treatment of Cancer; MDADI: MD Anderson Dysphagia Inventory; C/RT: chemo-radiation therapy; VFSS: videofluoroscopic swallowing study; QoL: quality of life; NMES: neuromuscular electrical stimulation.
| Author | Sample size (gender) | Age (years, Mean ± SD) | Tumour staging of participants | Treatment techniques (n) | Main objectives | Outcome measures | Main findings | MMAT quality rating |
|---|---|---|---|---|---|---|---|---|
| Li et al.41 | 334 (90F:244M) | 51.07 ± 10.07 | Stage I – 5 Stage II – 49 Stage III – 163 Stage IV – 117 |
2D-RT (252), IMRT (82); Neoadjuvant chemotherapy (141); Concurrent chemotherapy (179) | Investigate the swallowing status and its impact on quality of life | VFSS and scores of the WHO quality of life – BREF | Dysphagia as proven by VFSS is negatively correlated to domains of the WHOQOL-BREF | 4/5 |
| Lovell et al.39 | 51 (11F:40M) | 46.0 ± 10 | Stage I-II – 19, Stage III-IV – 32 | RT only (20), C/RT (31) | Determine the impact of dysphagia on QoL in patients treated for NPC | QoL measurements | Swallowing difficulties negatively impacts quality of life in NPC patients | 5/5 |
| Tong et al.40 | 60 (18F:42M) | 34–71 | Not available | Not specified | Explore the perceptions and experiences of swallowing difficulties in NPC patients post-RT | Transcribed interviews on QoL | Informants' concerns focused more on the threat of cancer recurrence, thus paid less attention to the radiation-induced swallowing complication | 4/5 |
- NPC: nasopharyngeal cancer; MMAT: Mixed Methods Appraisal Tool; RT: radiation therapy; IMRT: intensity modulated radiation therapy; VFSS: videofluoroscopic swallowing study; WHOQOL-BREF: World Health Organization Quality of life - BREF; C/RT: chemo-radiation therapy; QoL: quality of life.
Prevalence
The prevalence of dysphagia was determined either by patient or clinician reported outcome measures.42 Eight of the 28 papers contained mention of dysphagia prevalence figures based on patient self-report measures.7-9,19,21,25-27 These figures varied widely between studies from 13% to 93.5%.9,27 Twelve of the 28 papers contained mention of dysphagia prevalence figures based on instrumental assessment of swallowing as part of their data analysis (Table 1).7-10,19,21-27 The prevalence of penetration ranged from 0% to 91.6% while aspiration was seen in 0%–83.9% of the participants (Table 4).8,9,19,26,27
| Oral phase | |
| Oral stasis | 27.6%–34.8%8 |
| 69%–100%27 | |
| Increased mucosal coating | 32.9%-72.4%8 |
| 96.5%27 | |
| Poor bolus formation/transfer | 46%–54%19 |
| 0–45%26 | |
| Prolonged oral transit | 76%–96%19 |
| Pharyngeal phase | |
| Residue at valleculae | 40.8%–78.3%8 |
| 0–100%26 | |
| 85.8%–100.0%27 | |
| Residue at pyriform fossa | 39.5%–82.6%8 |
| 93.5%9 | |
| 73%21 | |
| 0–60%26 | |
| 54%–100%27 | |
| Laryngeal penetration | 16.7%7 |
| 0–15.8%8 | |
| 47%–62%10 | |
| 0–68%19 | |
| 17.6%–37.6%23 | |
| 22.5%24 | |
| 10%–35%26 | |
| 48.7%–91.6%27 | |
| Aspiration | 07 |
| 0–4%8 | |
| 83.9%9 | |
| 17.0%–20.5%10 | |
| 0–22%19 | |
| 74%21 | |
| 33.3%22 | |
| 9.4%–73.0%23 | |
| 17.5%24 | |
| 83.3%25 | |
| 0–10%26 | |
| 9.7%–71.8%27 | |
- Data reported for multiple time points, bolus types, or treatment groups are indicated as ranges.
Examining the methodology of the papers revealed multiple factors were contributing to this extreme variability. Papers varied in recruitment methods from large clinical cohort studies to small clinical samples and often selected from specific caseloads leading to potentially biased sampling methods.7,8,10,21,25 Study designs were also different, including retrospective versus prospective cohorts,7-10,19,21-27 and all studies differed regarding when, relative to treatment, that the prevalence data was reported, with timing ranging from pre-RT to 47 years post treatment.10,26,27 Studies also varied in the tools used to determine dysphagia presence with 8 studies using videofluoroscopic swallowing studies (VFSS) and 4 studies using fiberoptic endoscopic evaluation of swallowing (FEES).7-10,19,21-27
Of the 12 papers to mention dysphagia prevalence, Chang et al8 had perhaps the most robust study design regarding chronic or long term dysphagia rates. They sampled a large cohort of patients (n = 184) at an average of 9.83 years post-RT and used both patient self-report questionnaire and VFSS to measure the presence of dysphagia. They found clear evidence of chronic swallowing difficulties in their cohort, with 48.6% of patients reporting swallowing difficulty and 71.8% of patients confirmed to be aspirating.8
In addition to studies reporting on actual dysphagia prevalence, two other studies reported prevalence figures for dysphagia related consequences,37,38 such as pneumonia. In a nationwide population-based study, in which a total of 3814 NPC patients who received curative C/RT were enrolled, it was found that 5.5% of the cohort had late-onset pneumonia.37 Another study reported that 26 out of 217 patients (12.0%) were diagnosed with aspiration pneumonia and required hospital admission.38 Other papers have discussed factors relating to increasing risk of dysphagia related complications. Yen et al37 reported that the addition of chemotherapy did not increase the chance of late-onset pneumonia but re-irradiation was positively correlated with increased risk. Xiong et al38 also reported that age was a strong risk factor for pneumonia post-RT in the NPC population.
Characteristics of swallowing impairment in NPC patients
Problems faced by NPC patients across phases of swallowing were reported in 13 papers (Table 1),7-10,19-27 and the specific characteristics observed, and functional deficits underlying these characteristics identified in each phase are summarized in Tables 4 and 5 respectively. Across the studies, instrumental assessments included VFSS (n = 8, 61.5%) and FEES (n = 4, 30.8%),7-10,19,21-27 while one (7.7%) used the Iowa Oral Performance Instrument (IOPI) to measure tongue strength and one (7.7%) used ultrasonography to measure suprahyoid muscle contraction.20,24
| Oral phase | |
| Impaired lingual control | 0–40%26 |
| Pharyngeal phase | |
| Velopharyngeal incompetence | 27.8%7 |
| 58.1%9 | |
| 10%19 | |
| 23.0%–95.8%27 | |
| Delay or absence of swallow reflex | 87.1%9 |
| 36%–62%19 | |
| 2.6%–52.1%27 | |
| Decreased pharyngeal contraction | 1.3%–5.7%8 |
| 80.6%9 | |
| 78%–92%19 | |
| 69%21 | |
| 1.8%–71.8%27 | |
| Incomplete hyoid bone elevation | 8.7%–15.8%8 |
| 94%19 | |
| 1.8%–23.9%27 | |
| Impaired laryngopharyngeal sensation | 88%21 |
| Esophageal phase | |
| Cervical esophageal clearance problem | 82.8%–97.0%10 |
- Data reported for multiple time points, bolus types, or treatment groups are indicated as range.
Six of the papers identified the presence of issues with the oral stage of swallow, all using VFSS.8,10,19,24,26,27 Four studies used dichotomous parameters such as “poor bolus formation” and “increased mucosal coating”,8,19,26,27 while three reported the oral transit time (Table 4).10,24,27 Chang et al27 reported patients may have oral phase impairment prior to RT, characterized by oral stasis and increased mucosal coating, though this was not reported by Ku et al26 in their studied cohort. After RT, oral phase impairments, specifically poor bolus formation and prolonged oral transit, were reported 1 year post-RT.26,27 In cohorts >1 year post-RT, an increasing trend of oral phase impairments were observed as time lapsed after RT across studies.8,27 The most common problem reported in the oral phase was increased mucosal coating, ranging from 32.9% to 96.5%.8,27
To explain the observed deficits in the oral phase of the swallow, specific functions related to the tongue have been investigated (Table 5). In one study, the IOPI was used to measure tongue strength and endurance before and 2 months after RT.20 It was found that the 12 studied NPC patients did not differ significantly from the matched healthy controls before or after RT. In another study using VFSS, no patient had lingual control problem prior to RT but 40% (n = 20) had impaired lingual control up to 1-year post-RT.26
Pharyngeal phase impairments were more well documented (Tables 4 and 5), with 12 of the papers confirming issues with the pharyngeal stage of swallow. For studies that used VFSS, 4 studies used an array of dichotomous parameters such as “poor pharyngeal contraction”,8,19,26,27 4 studies included quantitative parameters such as hyoid bone displacement,10,22,24,27 while one study only reported on the presence of aspiration.25 For studies that used FEES, all used an array of dichotomous parameters.7,9,21,23 The prevalence of residue at the valleculae and pyriform fossa was reported to range from 0 to 100% (see Table 4). The prevalence of penetration and aspiration varied (0–91.6%) as discussed earlier. In patients prior to RT, Chang et al27 and Ku et al26 reported a low incidence of penetration (10%–14.5%) and aspiration (1.3%–10%), whereas the highest incidence of aspiration post RT were reported by Phua et al25 (n = 18, 83.3%) and Wu et al9 (n = 31, 83.9%). Only 2 studies specified whether the aspiration was silent in nature. Wu et al9 reported 42% of all participants (n = 31) had silent aspiration while Ng et al23 reported 66% of the 85 patients had silent aspiration. Ng et al23 also found that it was more common on thin liquid and least likely on soft diet.
To explain the swallow deficits in the pharyngeal phase, a number of the studies investigated the physiological events in this phase of the swallow. The most commonly reported deficit was decreased pharyngeal contraction. A low incidence of such was reported prior to RT, observed in only 1.3%–10% of participants in two studies.26,27 After RT, across studies, prevalence of decreased pharyngeal contraction was reported to range from 1.3% to 92.0%,19,27 with the lower prevalence seen in studies with participants who had completed RT within 1–2 years prior to assessment.8,27 Incomplete hyoid bone movement was also reported and the prevalence varied greatly among studies, ranging from 1.8% to 23.9%.24,27 Wang et al22 found that forward movement of the hyoid bone in terms of both displacement and velocity were significantly less compared to healthy subjects. Reduced pharyngeal contraction and hyoid bone movement were identified as risk factors for aspiration.21,22,24 Apart from them, the maximum opening of the cricopharyngeus muscle,22,24 the movement of the velum,9,19 initiation of swallow8,10,19,24 and laryngopharyngeal sensation have all been reported to be impaired.21
There has only been one study to date that has specifically examined esophageal phase impairments in NPC patients (Table 5). Fong et al10 investigated the prevalence and associated impacts of cervical esophageal clearance issues by VFSS. It was found that stasis in the cervical esophagus was highly prevalent, present in 82.8% and 97.0% of their participants on thin liquid and semi-solids respectively. There was also a trend of more severe or opharyngeal impairments, including aspiration, with a greater impairment of cervical esophageal clearance. It was suggested that swallowing evaluation, in particular VFSS, for NPC patients should also include the cervical esophagus region in order to fully assess the swallowing function.
Prevention and treatment of dysphagia in NPC patients
Prevention of dysphagia by RT techniques
One of the ways to reduce the occurrence of dysphagia and its impacts, is to minimize the effect of RT on the structures of the head and neck. There were 4 studies that investigated the effect on swallowing function by different RT techniques and the dose–effect relationship (Table 2).33-36 Three different RT techniques were compared across two studies33,34; 3D conformal RT, intensity modulated radiation therapy (IMRT) and IMRT with anterior neck field shielding. Jiang et al36 found that the severity of dysphagia was significantly correlated to the radiation dosage delivered to the superior and inferior pharyngeal constrictors. In other work, the dosage to the pharyngo-esophagus area and the duration of feeding tube dependence were both found to be significantly less in participants with shielding. However, one other study found no obvious difference in swallowing function when patients were treated with 3D conformal RT against IMRT.33 More work is needed to determine if any modifications to RT dose and field can lead to positive benefits for swallowing outcomes in this population. As Messer et al35 noted, although serial imaging was able to identify the early and late radiation-induced changes in dysphagia-associated structures, the relationship between functional changes and the structural changes needs further investigation.
Efficacy of dysphagia treatment
In this review, 6 included studies (Table 2) investigated the effectiveness of treatment of dysphagia.15,28-32 Two of the studies investigated the outcomes of surgical methods (cervical esophagostomy and laryngotracheal separation) and concluded that, after careful selection of surgical candidates, those surgeries can be beneficial to NPC patients in terms of prevention of pneumonia and improving quality of life.30,31 In the other 4 studies, effects of electrical stimulation, swallowing exercises and balloon dilation were studied. Lin et al15 concluded that electrical stimulation led to a significantly greater improvement on the penetration–aspiration scale when swallowing paste and the hyoid bone velocity when swallowing thin liquid than the regular exercise group.43 The effect of rehabilitation exercises were investigated by Tang et al29 and found that the rehabilitation group (tongue, jaw and swallow exercises) had significant improvement in swallowing function and trismus, as measured by water swallowing test and inter-incisor distance respectively.29 The effect of balloon dilation on 13 NPC patients was investigated by Fong et al32 and it was concluded that after a single dilation done under endoscopy, the status of penetration-aspiration improved on swallowing thin liquid, there were also functional gain and also an improvement in the patient self-reported scores. Finally, the effect of a combination of electrical stimulation and balloon dilatation on NPC patients was investigated.28 In that study, 60 subjects were recruited and 31 received both treatments and 29 were in the control group of which traditional strengthening exercises were prescribed. In both groups, there was significant improvement in all parameters following a 4-month rehabilitation program.
Dysphagia-related quality of life
The impact of dysphagia on the quality of life has been investigated in 3 studies (Table 3).39-41 Lovell et al39 conducted a cross-sectional survey of 51 NPC patients using the Washington Quality-of-life Questionnaire and the Swallow Quality-of-life Questionnaire,44,45 Li et al41 used the World Health Organization quality of life – BREF on 334 patients,46 while Tong et al40 used semi-structured interviews on 60 patients. Across studies, patients’ self-reported swallowing difficulties ranged from 84% to 85%,39,40 the problem was more apparent with solids.39,40 Discomfort during swallow was also frequently reported.39-41 Patients with swallowing difficulties were found to have worse quality of life in all three studies.39-41 Lovell et al39 found that with increase in time-post-onset, the health-related quality of life showed improvement despite the negative impact of dysphagia. The authors postulated that this could be due to patients being more adapted to the condition or had a more realistic expectation of the condition. Tong et al40 reported that the risk of aspiration was often neglected by patients themselves and they were not aware of the signs associated with it.
Discussion
The purpose of the review was to collate the findings from the literature on dysphagia in NPC patients. Using different instruments, the problems across the oral, pharyngeal and esophageal phase of swallowing were revealed. The literature also covered how C/RT affects swallowing function and whether the negative effects can be minimized, as well as whether swallowing treatment is effective on dysphagia. From the literature, it can be concluded that dysphagia is prevalent in the NPC population, regardless of the outcome measure used. The exact prevalence is difficult to be determined, but across studies that reported the incidence of aspiration the rates were as high as 83.9%,9 with negative long term consequences such as aspiration pneumonia reported in up to 12.0%. This figure was similar to what has been reported for head and neck cancer survivors.47 These figures support that dysphagia is prevalent post NPC treatment and should be assessed and managed appropriately.
However, to inform management, further work is required to fully understand the nature of the swallowing impairments in this population. This scoping review has revealed that the few existing studies confirm deficits across all phases of the swallow, though again there is high variability in the evidence reported to date. Oral phase impairments have been investigated and oral stasis and increased oral mucosa coating reported.8,27 It was seen that, across studies, oral phase impairment was common regardless of the time lapse post-RT, and appeared to worsen with time lapse post RT.8,26,27 Although these swallow features would suggest lingual dysfunction, in the one study to date that used IOPI to measure tongue strength and endurance, NPC patients did not differ from the controls pre and 2 months post RT, suggesting that tongue strength and endurance were preserved after RT within 2 months.20 However it is well understood that lingual function on non-swallow tasks such as strength and endurance tasks versus lingual function during bolus control and manipulation during swallowing do not directly equate. Therefore, the issue of whether lingual dysfunction exists in this population remains to be further investigated. It is also possible that other factors, for example xerostomia, could also be contributing to features such as mucosal coating.
Although limited in the number of studies conducted, the problems in pharyngeal phase have been more extensively investigated in the NPC population with both VFSS and FEES studies conducted. In most of the 13 studies currently available, the prevalence of penetration and aspiration were high. In one of the studies where a relatively lower prevalence of aspiration was reported,7 the authors postulated that it could be due to the fact that they all received IMRT and not two-dimensional RT, and the technique that was used was a single field technique and no anterior neck junction was applied. The laryngeal dose was also below 40 Gy, which may have better preserved the laryngeal vestibule closure during swallow in this cohort.7 Apart from that particular study, in most studies where more chronic patients were studied, the prevalence of aspiration was as high as 83.9%.9 NPC patients were also prone to silent aspiration and this is secondary to their impaired laryngopharyngeal sensory deficit as confirmed by Ku et al.21 The “silent” nature of aspiration could also be one of the factors why patients tend to under-estimate the severity of their swallowing problem, as revealed by Tong et al40 in their semi-structured interviews. Hence the existing evidence supports that NPC patients should receive routine instrumental assessment of swallowing post C/RT to monitor their swallowing function and determine aspiration risk.
To date the esophageal phase has been the least studied phase of swallowing post NPC management. Currently, only one study has examined esophageal clearance problems,10 finding that difficulty with esophageal clearance was highly prevalent, and potentially was associated with aspiration. That study was a retrospective study, and acknowledged issues with the modified outcome measure employed. Therefore, much more research is needed to make any definitive statements regarding the extent of issues with the esophageal stage. In the future, the potential to include manometric assessments could also help understand the nature of esophageal phase deficits and the interaction between esophageal stasis and issues with the oropharyngeal phase in this population.
In the HNC population, compensatory strategies and rehabilitative exercises have been used to improve the swallowing efficacy.48 The number of studies on the effectiveness of swallowing therapy in NPC population is very small. As such, it is difficult to draw any firm conclusions. In the literature, the effect of traditional muscle strengthening and swallowing exercises for NPC patients remains in question.29 The use of electrical stimulation was reported to have significant effect on improving the status of aspiration,15 however, the results of those studies must be interpreted with caution due to the limited nature of the outcome measure used (the water swallow test) to document treatment effect. In particular, the high rates of silent aspiration in this population question the accuracy and use of that tool for this population. Equally, in the treatment study that combined dilation and electrical stimulation,28 the exact therapy regime and dosage were not clearly described in the article. Balloon dilation alone was shown to be effective in one other study,32 however the study was a pilot study and the sample size was small and long term data on sustained benefit was not reported. In conclusion, the evidence regarding treatment options for dysphagia post NPC management is very limited and is another area that warrants further systematic research.
The potential for modified RT management to have positive impact on swallowing outcomes is another area with emerging evidence. The limited studies to date on the RT dose–effect relationship have suggested that dose to the pharyngeal constrictors is highly correlated with swallowing deficits over time.35,36 There are also studies that have identified superior swallowing benefits with more highly conformal RT techniques such as IMRT. IMRT has been shown to be more superior in tumor control and survival in NPC patients,6 it has now been adopted as the standard of care. Compared to older forms of 2 dimensional RT, potential swallowing benefits may have also been achieved through the adoption of IMRT.6 At present, the emerging literature supports that RT techniques, especially shielding and avoiding structures critical for swallowing (the pharyngeal constrictors), can be used to prevent, or at least lessen the severity of, dysphagia.34-36
The current review has highlighted the need for systematic use of clinical and instrumental assessments to ensure that the extent of dysphagia in this population to detected and supported over time post NPC. However, additional tools, including those that assess quality of life are also critical to help understand how dysphagia is impacting the life of the individual patient.49 Very few studies have been conducted to date, with quality of life reported to be adversely affected by dysphagia.39-41 Though, it was also reported that the extent of the impact changed as time lapsed after RT,40 or when dysphagia became more chronic.40 As previously discussed, existing evidence suggests a trend of worsening of swallowing function over time post C/RT.8,9,27 It has been proposed that this pattern of improving quality of life, despite potentially declining swallow function long term, may simply indicate how patients adapt and adjust to having a swallowing problem – and how they feel it affects quality of life.40 While a degree of long-term adjustment is expected for people living with chronic conditions, the impacts of dysphagia should be discussed with all patients to ensure that any patient needing psychosocial supports receives timely intervention and management.
Limitations
This was the first review paper to collate the existing evidence regarding swallowing and dysphagia management in NPC patients and there are a number of acknowledged study limitations. Firstly, the heterogeneity of the methods used across the existing literature made it very difficult to create summaries and/or compare problems reported in different phases of swallowing across different research. There was high variability in the instruments/tools used, the bolus types assessed, and the parameters used to analyze the results – thus limiting the capacity to combine data or find common patterns in findings across studies. Secondly, the number of longitudinal studies were minimal (n = 2). Therefore, any discussion of changes to presenting features over time need to be interpreted with caution.
Conclusion
The pattern in the literature to date supports that dysphagia is a common long term toxicity in individuals with NPC after C/RT, although specific incidence figures remain highly variable across studies. Aspiration, particularly silent aspiration rates are reported to be high and instrumental assessments, though limited in number, highlight deficits in the oral, pharyngeal and esophageal stages of the swallow. The presence of dysphagia can impact quality of life in this population and should not be overlooked. More emphasis should be placed on patient education about potential swallowing changes post NPC management. Medical professionals who manage NPC patients clinically should also be aware of the risks and long term swallowing status of their patients. Future studies are needed in the area of effective treatment for this population. Further research into dysphagia, its nature and its consequences for the patient is still needed to achieve optimal management for this population.
CRediT authorship contribution statement
Raymond Fong: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing - original draft. Elizabeth C. Ward: Conceptualization, Methodology, Supervision, Validation, Writing - review & editing. Anna F. Rumbach: Conceptualization, Methodology, Supervision, Validation, Writing - review & editing.
Declaration of Competing Interest
None.