Utility of CT and MRI in assessment of mandibular involvement in oral cavity cancer
Abstract
Objective
Oral cavity squamous cell carcinoma (SCC) may present with early invasion of mandibular bone. Preoperative planning of surgery is essential considering patient's postoperative quality of life. Our purpose was to evaluate the efficacy of computer tomography scan (CT) and magnetic resonance imaging (MRI) in detecting mandibular bone involvement in oral SCC.
Methods
A retrospective study was conducted on 98 patients with SCC of floor of mouth, lower alveolus and retromolar trigone operated on with curative intent. Preoperative CT and MRI scans were re-reviewed by a consultant radiologist and original histology slides were re-reviewed by 3 pathologists.
Results
Forty-five patients were included in the final study. Combined CT and MRI had a sensitivity of 100% and a specificity of 72%.
Conclusion
The results suggest that combined CT and MRI have diagnostic utility in detecting mandibular invasion by oral cancer, but with a significant false positive rate.
Introduction
Oral cancer represents an important global healthcare problem with more than 150 cases per year diagnosed in Ireland.1 It is the 14th most common cancer in the UK (2013)2 and the 10th most common in Ireland.1 Its incidence has increased by 39% in the last decade, with similar increase in rates for males and females.2
Oral cavity squamous cell carcinoma (SCC) poses a challenge in surgical management especially when considering locally advanced cases. Mandibular invasion is common (12%–56%).3-5 The decision for mandibulectomy (in the form of marginal or segmental mandibulectomy) in order to achieve 3-dimensional clearance and negative margins should be considered and discussed with the patient in advance. Mandibulectomy may have implications for speech, swallowing and cosmetics in the postoperative period, and may require complex reconstructive techniques.
Preoperative imaging is clearly of importance in determining involvement of mandible by oral cancer and determining extent of mandibulectomy. Optimum imaging modalities for the oral cavity should be non-time consuming, cost-effective and reliable. There is controversy regarding the best technique with CT regarded by some authors to be preferable.6-8 Imaging of the oral cavity is also important for assessing tumour thickness, which is associated with local and regional recurrence, survival rates and the presence of metastatic deposits in the neck.9-11
Our study purpose was to establish the efficacy of CT and MRI alone and in combination in detecting mandibular bone invasion in oral SCC.
Materials and methods
Inclusion criteria
Inclusion criteria for the present study were patients with floor of mouth, lower alveolus and retromolar trigone SCC who underwent marginal or segmental mandibulectomy as primary surgical treatment between 2006 and 2015. Patients were identified by query of our Head & Neck Cancer database. Medical charts, radiology and histology results were retrospectively reviewed. Availability of medical charts, original histology slides and preoperative images was required for inclusion in the final study cohort. Patients with recurrent SCC of oral cavity were excluded.
Histological evaluation of bone invasion
Histological slides were re-reviewed by 3 pathologists and cases classified as “positive for bone invasion” (if invasion through cortical bone to involve spongiosa/medullary cavity was seen) or as “negative for bone invasion”.12, 13
Radiological evaluation of bone invasion
Preoperative images were re-reviewed by a consultant radiologist and cases classified as “positive for bone invasion” (if cortical bone erosion, bone destruction – on CT and abnormal marrow signal – on MRI) or “negative for bone invasion”.13-15
Computer Tomography images were achieved using a 64 slices GE MEDICAL SYSTEM OPTIMA CT 660, reconstruction matrix 512 × 512. Post intravenous iodine contrast (Omnipaque 350 mg/ml) administrated helical scan from the skull base to the sternal notch, 0.625 mm collimation and 0.9 pitch were used in every patient. This was followed by sagittal and coronal reformates and bony window reconstruction.
Our 1.5 T (Tesla) Magentic Resonance Imaging GE MEDICAL SYSTEM SIGNA HDxt, reconstruction matrix 512 × 512 was used preoperatively for the patients in this group. The protocol used for every patient was: coronal STIR (Short Time Inversion Recovery), sagittal T2, sagittal T1, axial T1, axial and sagittal T1 post intravenous paramagnetic contrast, with fat suppression. The contrast substance used was Gadolinium DTPA at a dose of 0.1 mmol/kg of body weight. The cut thickness varied between 4 mm and 5 mm.
The radiologist was blinded to the histopathological results and all our pathologists were blinded to radiological reports.
Statistical analysis was carried out processing the data through Office Excel and Office Access 2007. Sensitivity, Specificity and Accuracy were calculated.
Ethical approval for the present study was obtained from The Cork Clinical Research Ethics Committee (CREC).
Results
Forty-six is the final number of patients included in this study. The median age of our patients was 59.7 years (ranging from 42 to 81 years). Case distribution according to patient’ sex, smoking and alcohol history, oral cavity subsite, type of mandibulectomy performed and preoperative imaging modality re-reviewed is presented in Table 1.
| Variable | Number of cases | |
|---|---|---|
| Sex distribution | Male | 34 |
| Female | 12 | |
| Heavy smokers or ex-smokers | 39 | |
| Alcohol consumers | 37 | |
| Sub-site of oral cavity | Floor of mouth | 28 |
| Lower alveolus | 11 | |
| Retromolar trigone | 7 | |
| Mandibulectomy type | Marginal | 23 |
| Segmental | 23 | |
| Imaging modality | CT | 45 |
| MRI | 21 | |
| Combined CT + MRI | 20 | |
| Bone invasion on imaging | Yes | No | Bone invasion on histopathology |
|---|---|---|---|
| CT | 26 | 19 | 22 |
| MRI | 10 | 11 | 8 |
| CT + MRI | 13 | 7 | 8 |
All forty-six patients in the final study cohort had their original histopathology slides and preoperative scans (CT and/or MRI) re-reviewed to assess for the presence of bone invasion. Forty-five patients had CT performed as preoperative imaging modality, 21 had MRI scans. From all the cases included in the study, 20 patients had combined preoperative CT and MRI.
Fig. 1 illustrates mandibular invasion on axial MRI and CT of the same patient. On CT (A) cortical erosion alone can be seen whilst on MRI (low T1 signal, B) medullary invasion can be appreciated.
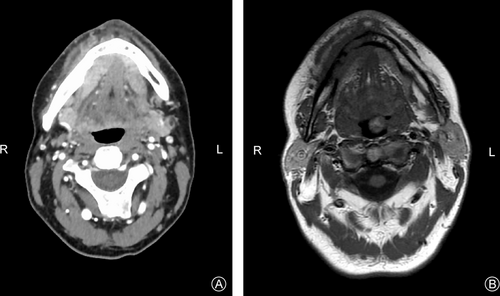
Axial CT and MRI of the same patient showing bony involvement. A: CT (cortical erosion); B: T1 MRI (cortical and medullary invasion up to the median point of mandible).
Results comparing the 3 sub-groups of scans and final histopathological assessment of bone invasion are summarized in the Table 2 shown above Fig. 1.
All of the cases with histologically confirmed bony invasion showed medullary involvement and this were confirmed by complete agreement between all three pathologists on re-review. Given these findings all cases reported to be negative for bony invasion were also re-reviewed by the same 3 pathologists and the absence of even minor cortical erosion was confirmed in all cases. Fig. 2 is a lower power microscopy image (5x) showing medullary bone invasion.
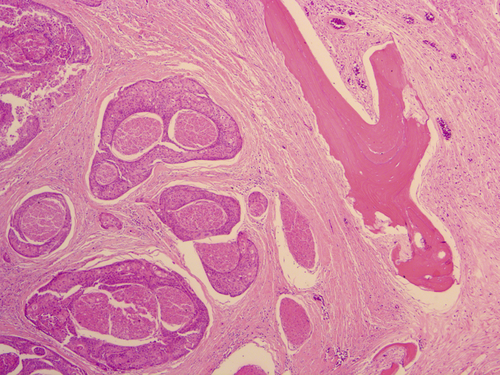
Lower power image (5x) showing bone invasion with a bony trabecula on the right of the image and invasive SCC on the left.
Comparing the initial preoperative scanning reports with the re-reviewed reports, 2 patients were upgraded to “bone invasion”, one of which was confirmed on final histopathology.
The kappa coefficient, scored interval interobserver agreement (IOA) and interval-by-interval IOA were used to evaluate the interobserver agreement on reviewing CT and MRI images. Results are presented in Table 3.
| Interobserver agreement | CT | MRI | CT + MRI |
|---|---|---|---|
| Kappa coefficient | 1 | 0.9 | 0.9 |
| Scored IOG (%) | 91 | 91 | 100 |
| Interval-by-interval IOG (%) | 95 | 93 | 95 |
Table 4 compares the sensitivities, specificities and accuracy of all 3 imaging groups: CT, MRI and combined preoperative CT and MRI group. MRI exceeded CT in diagnosing patients with mandibular invasion due to its higher sensitivity.
| Imaging modality groups | Sensitivity (%) | Specificity (%) | Accuracy (%) |
|---|---|---|---|
| CT (n = 45) | 86 | 80 | 80 |
| MRI (n = 21) | 88 | 83 | 85 |
| CT + MRI (n = 20) | 100 | 72 | 85 |
Discussion
Originality
There are no prior studies in the literature evaluating the potential role of combined CT and MRI in assessing mandibular involvement in oral carcinoma. The focus in other studies has been to establish the single best method of scanning these patients preoperatively. Li et al6, 16 found in two separate meta-analyses that CT had a sensitivity of 72% with a specificity of 90% and that MRI had a sensitivity of 78% and a specificity of 83%.
In our study MRI tends to over-estimate bone invasion which is in keeping with the literature findings.6, 16-22 This is due to similarities in signal of tumoral tissue and peritumoral inflammation or infection. Magnetic resonance imaging is known for multiple artefacts related to tissue, motion or technique.
Radiological and histopathological differences in bone invasion
When evaluating the sensitivity and specificity of CT and MRI in detecting mandibular bone invasion by oral SCC it is critical to appreciate that the radiological and histopathological definitions of bone involvement are discordant. Cortical erosion alone is required radiologically. In contrast histopathologically superficial cortical erosion is insufficient to classify a patient as having pathological bone involvement (pT4a) as this has not consistently been shown to be of prognostic significance. Instead invasion into the medullary cavity is necessary pathologically to be called positive bone invasion.12, 13 This is a likely contributory factor to the reported low specificity of both CT and MRI in the evaluation of mandibular bone invasion by SCC.6, 16-18 Although histological re-review confirmed the absence of microscopic evidence of cortical erosion in all cases in our series, some cases of minor cortical involvement may not have been identified due to incomplete sampling process.
Our false positive results on CT and MRI group (5 patients) might be due to the fact that cortical bone is not fully sampled during standard sampling procedure in the laboratory. Another possibility is that CT and MRI might supra estimate bone invasion by picking-up minor cortical inflammatory changes not related to the tumour.
Conclusions
In conclusion, our study suggests that combined CT and MRI have diagnostic utility in detecting mandibular invasion in oral cancer with a sensitivity of 100%, but with reduced specificity compared to either modality on its own. The reduced specificity may be clinically irrelevant as if there is clinical suspicion of bone involvement or if the tumour intraoperatively is contiguous or adherent to the bone, mandibulectomy would be indicated and performed. However, a more conservative approach may be prudent intraoperatively in cases where radiology is not definitive for bone invasion. Further studies, including new imaging techniques as dual energy CT are needed to determine the gold standard preoperative imaging method/s for oral SCC.23, 24
Conflict of interest
The authors have no funding, financial relationships or conflicts of interest to disclose.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.wjorl.2019.02.001.