Cardiac troponin T as a predictor of cardiac death in patients with left ventricular dysfunction
Abstract
Background
Cardiac troponin T (cTnT) has been reported to be associated with cardiac mortality.
In the present study, we evaluated the role of routine assessment of cTnT as a predictor of future cardiac death in patients with left ventricular (LV) dysfunction.
Methods
Patients who were eligible for prophylactic implantable cardioverter defibrillator (ICD) were included from cardiac catheterization database. Inclusion criteria were patients with LV ejection fraction of ≤ 35% and with New York Heart Association (NYHA) ≥class II. Exclusion criteria were patients with acute coronary syndrome, ICD for secondary prevention, NYHA class IV, and lack of data. The final study patients were divided into the following three groups in accordance with two quartile points of serum cTnT levels: low cTnT, intermediate cTnT, and high cTnT groups. The primary endpoint of this study was cardiac death.
Results
A total of 70 patients were included (mean age, 62±13 years; male individuals, 56; ischemic, 36; and non-ischemic, 34). During the observation period of 2.2 years, cardiac death was observed in 17 patients (fatal arrhythmic event, 9; heart failure, 7; myocardial infarction, 1). In the Kaplan–Meier analysis, the high cTnT group showed the highest risk among all the groups (p<0.001). Even in sub-analyses for ischemic and non-ischemic patients, the results were the same, and the high cTnT group showed the highest event rate (p<0.05). In contrast, no cardiac death was observed in the low cTnT group.
Conclusion
The cTnT levels in a stable state were associated with cardiac death in patients with LV dysfunction, even in those with non-ischemic diseases.
1 Introduction
Patients with left ventricular (LV) dysfunction have been shown to be at risk of cardiac death [1], [2]. Many mega-trials have demonstrated a significant reduction in the risk of sudden cardiac death with an implantable cardioverter defibrillator (ICD) among patients with LV dysfunction [LV ejection fraction (LVEF),<35%] [3]-[6]. Therefore, the European and American guidelines recommend prophylactic use of ICDs as a class I indication in patients with symptomatic heart failure and low LVEF, even without preceding fatal arrhythmic events [1], [2], [7], [8]. Japanese guidelines have recommended prophylactic ICD implantation in patients with LV dysfunction as a class I or IIa indication [7]. However, evidence for the benefit of prophylactic ICD is much stronger among patients with ischemic heart disease (IHD) than among those with non-IHD. Køber L et al. [9] reported that prophylactic ICD implantation was not associated with improvement of mortality with respect to death from any cause in patients with non-IHD heart failure. Therefore, practical risk stratification is important to make accurate decisions on the prophylactic use of ICD, especially in patients with LV dysfunction due to non-IHD. Elevation of serum cardiac troponin T (cTnT), a sensitive biomarker of myocardial injury, has been reported to be associated with poor long-term prognosis in patients with LV dysfunction in the absence of any obvious myocardial ischemia [10]. However, the usefulness of routine assessment of cTnT in patients with LV dysfunction in a stable state has not been evaluated. In the present study, we evaluated clinical outcomes of patients with LV dysfunction who were eligible for prophylactic ICD and assessed the role of cTnT measurement as a predictor of future cardiac events in such a population.
2 Material and methods
2.1 Study population
This single-institution retrospective observational study used patient data from the cardiac catheterization database of Kitasato University Hospital. We assessed 2500 patients who underwent cardiac catheterization between 2010 and 2013. The inclusion criteria were as follows: (1) age of ≥20 years (male or female gender), (2) cardiac catheterization performed between 2010 and 2013 in our institution, (3) LV dysfunction of <35%, (4) New York Heart Association (NYHA) ≥class II (because this study was designed to evaluate future cardiac events in patients with LV dysfunction and moderate symptomatic heart failure who were eligible for prophylactic ICDs), and (5) presence of written informed consent. The exclusion criteria were as follows: (1) acute coronary syndrome, (2) ICDs for secondary prevention, (3) NYHA class IV, and (4) lack of clinical data including cTnT. LVEF was examined with transthoracic echocardiography using the modified Simpson method (Aplio500, TOSHIBA, Tochigi, Japan). IHD was diagnosed according to the presence of >75% stenosis of at least one of the three major coronary arteries or a documented history of myocardial infarction. Other cardiac diseases were diagnosed according to the findings of cardiac catheterization, echocardiography, and/or myocardial biopsy. Clinical data, such as medical history, physical examination findings, electrocardiogram findings, and blood test results, were obtained in the stable state of each underlying heart disease. We defined stable state as a condition without any changes in symptoms or heart condition in each patient at least more than a month after or before being hospitalized. All of the laboratory data, including cTnT, were obtained from outpatients who visited for regular medical check-up.
2.2 Grouping and data comparison
Patients were divided into the following three groups according to serum cTnT levels using the 1st and 3rd quartile points: low cTnT, intermediate cTnT, and high cTnT groups. Various clinical parameters and future cardiac events were compared among these three groups.
2.3 Evaluation of cardiac events
The primary outcome of this study was cardiac death. The causes of cardiac death were classified into fatal arrhythmic events, exacerbation of heart failure, and myocardial infarction. A fatal arrhythmic event was defined as the composite of sudden cardiac death or documentation of life-threatening arrhythmia.
2.4 Statistical analysis
The baseline characteristics were compared among the three groups using analysis of variance (ANOVA) with a Tukey-HSD post hoc test for continuous data and the Pearson's chi-square test for categorical data, respectively. Mortality levels in the three groups with different levels of serum troponin T were evaluated using Kaplan–Meier survival analysis and the log-rank test. Association between troponin T levels and mortality was also analyzed in each group using the multivariate Cox proportional hazard model, and the hazard ratios (HRs) and 95% confidence intervals (95% CIs) were determined. A p-value of <0.05 was considered statistically significant. All statistical analyses were performed using the JMP 11 (SAS Institute Inc., Cary, NC, USA) statistical software.
3 Results
3.1 Baseline characteristics
A total of 105 patients met the inclusion criteria. Of these patients, 35 met the exclusion criteria (6 had acute coronary syndrome, 10 received an ICD for secondary prevention, one had NYHA IV, and 18 did not have sufficient clinical data). Finally, the remaining 70 patients were selected as the follow-up population with LV dysfunction and moderate heart failure symptoms.
Table 1 shows the baseline characteristics of all patients and the three subgroups with different levels of serum cTnT. The low cTnT group (≤0.006 ng/ml) included 16 patients, intermediate cTnT group (0.006–0.04 ng/ml) included 36 patients, and high cTnT group (>0.04 ng/ml) included 18 patients. In the overall population, the mean patient age was 62 years, and the male:female ratio was 56:34. IHD and non-IHD were the underlying heart diseases in 36 and 34 patients, respectively. Non-IHD included idiopathic dilated cardiomyopathy (n=28), cardiac sarcoidosis (n=4), valvular heart disease (n=1), and hypertrophic cardiomyopathy (n=1). There were no significant differences in serum cTnT levels in both ischemic and non-ischemic patients (p=0.3919, data not shown). In the high cTnT group, 16 of 18 patients had NYHA class III. The prevalence of diabetes and renal failure with dialysis history was higher in the high cTnT group than in the other groups. A defibrillation device was prophylactically implanted in 16 (22.8%) patients, and all of these devices were cardiac resynchronization therapy defibrillator (CRT-D) devices. There were no differences in the parameters of electrocardiography among the three groups. With regard to laboratory data, serum blood urea nitrogen, creatinine, and sodium levels were higher in the high cTnT group than in the other two groups; however, the brain natriuretic peptide level did not show any difference. With regard to baseline medications, the use of beta-blockers was lower in the high cTnT group than in the other two groups.
| Overall (N=70) | Low (N=16) | cTnT | High (N=18) | p Value⁎ | p Value (vs. High) | |
|---|---|---|---|---|---|---|
| Intermediate (N=36) | ||||||
| Age, yrs | 61±13 | 60 ±15 | 59±13 | 67±11 | 0.1607 | |
| Gender male | 56 (80.0) | 10 (62.5) | 29 (80.5) | 17 (94.4) | 0.0666 | |
| IHD | 36 (51.4) | 9 (56.2) | 15 (41.6) | 12 (66.6) | 0.2024 | |
| NYHA class II | 39 (55.7) | 12 (75.0) | 25 (69.6) | 2 (11.1) | <.0001⁎ | |
| NYHA class III | 31 (44.2) | 4 (25.0) | 11 (30.5) | 16 (88.8) | ||
| CRT-D | 16 (22.8) | 3 (18.7) | 10 (27.7) | 3 (16.6) | 0.5991 | |
| SBP, mmHg | 116±27 | 113±19 | 115±30 | 121±27 | 0.648 | |
| Heart rate, bpm | 82±21 | 85±18 | 84±22 | 75±23 | 0.328 | |
| Comorbidities | ||||||
| Hypertension | 40 (57.1) | 6 (37.5) | 21 (58.3) | 13 (72.2) | 0.1217 | |
| Diabetes | 30 (42.8) | 4 (25.0) | 14 (38.8) | 12 (66.6) | 0.0222⁎ | |
| Dyslipidemia | 36 (51.4) | 6 (37.5) | 18 (50.0) | 12 (66.6) | 0.2293 | |
| Smoking | 43 (61.4) | 8 (50.0) | 24 (66.6) | 11 (61.1) | 0.5221 | |
| CVD | 17 (24.2) | 3 (18.7) | 7 (19.4) | 7 (38.8) | 0.1896 | |
| Dialysis | 6 (8.5) | 0 (0.0) | 1 (2.7) | 5 (27.7) | 0.0021⁎ | |
| Atrial fibrillation | 19 (27.1) | 2 (12.5) | 10 (27.7) | 7 (38.8) | 0.2234 | |
| NSVT | 11 (15.7) | 2 (12.5) | 6 (16.6) | 3 (16.6) | 0.9223 | |
| Electrocardiogram | ||||||
| QRS, msec | 129±36 | 137±44 | 124±28 | 132±41 | 0.4852 | |
| QTc, msec | 456±43 | 465±44 | 456±39 | 447±47 | 0.4455 | |
| Echocardiography | ||||||
| LVEF, % | 28.2±5.9 | 28.9±4.8 | 28.2±5.9 | 27.5±6.6 | 0.7809 | |
| LAD, mm | 45.0 ±16.1 | 41.9±7.7 | 47.5±20.9 | 42.7±7.9 | 0.4054 | |
| LVDd, mm | 63.9±8.5 | 65.6±8.5 | 65.2±7.4 | 59.8±10.4 | 0.0641 | |
| Laboratory data | ||||||
| Hb, g/dl | 13.4±2.1 | 13.4±1.7 | 13.6±1.7 | 12.9±2.9 | 0.5102 | |
| BUN, mg/dl | 25.1±16.5 | 18±4.5 | 22.5±14.3 | 36.8±25.3 | 0.0029⁎ | Low: 0.0045⁎ Intermediate: 0.0108⁎ |
| Cr, mg/dl | 1.5±1.4 | 0.9±0.2 | 1.1±0.7 | 2.7±2.6 | <0.001⁎ | Low: <0.001⁎ Intermediate: <0.001⁎ |
| TG, mg/dl | 124±93 | 134±90 | 122±101 | 117±73 | 0.8697 | |
| LDL-C, mg/dl | 99±33 | 101±30 | 97±34 | 103±33 | 0.8244 | |
| Na, mEq/l | 137±3.8 | 139±2.2 | 138±4.1 | 135±4.3 | 0.0136⁎ | Low: 0.0183⁎ Intermediate: 0.0361⁎ |
| K, mEq/l | 4.3±0.52 | 4.5±0.74 | 4.2±0.43 | 4.3±0.46 | 0.1218 | |
| BNP, pg/dl | 735±790 | 466±371 | 734±777 | 975±1047 | 0.1803 | |
| cTnT, ng/ml | 0.0415±0.086 | 0.0011±0.018 | 0.0188±0.012 | 0.1229±0.017 | <0.001⁎ | Low: <0.001⁎ Intermediate: <0.001⁎ |
| Medications | ||||||
| RASI | 67 (95.7) | 16 (100) | 35 (97.2) | 16 (88.8) | 0.2276 | |
| Beta-blocker | 61 (87.1) | 16 (100) | 34 (94.4) | 11 (61.1) | <0.001⁎ | |
| CCB | 9 (12.8) | 0 (0.0) | 6 (16.6) | 3 (16.6) | 0.2165 | |
| Aldosterone inhibitor | 36 (51.4) | 11 (68.7) | 18 (50.0) | 7 (38.8) | 0.2139 | |
| Statins | 34 (48.5) | 7 (43.7) | 17 (47.2) | 10 (55.5) | 0.7685 |
- Data given as mean±SD or n (%). p values represent the comparison among the 3 groups of low (cTnT <0.006 ng/ml), intermediate (0.006 ng/ml≤ cTnT <0.04 ng/ml), and high (cTnT >0.04 ng/ml). ⁎asterisk indicates statistical significance. BNP=brain natriuretic peptide, BUN=blood urea nitrogen, CCB=carcium channel blocker, cTnT=cardiac troponin T, Cr=serum creatinine, CRT-D=cardiac resynchronization therapy -defibrillator, Hb=hemoglobin, IHD=ischemic heart disease, K=serum potassium, LAD=left atrial diameter, LDL-C=low-density lipoprotein cholesterol, LVDd=left ventricular end-diastolic diameter, LVEF=left ventricular ejection fraction, Na=serum sodium, NIHD=non-ischemic heart disease, NSVT=non-sustained ventricular tachycardia, NYHA=New York Heart Association, RASI=rennin-angiotensin system inhibitor, SBP=systolic blood pressure, TG=triglyceride.
3.2 Long-term follow-up and prognosis
The follow-up period was 38.2±20.5 months. Cardiac death was observed in 17 of 70 patients (21.4%; incidence rate, 6.8 per 100 person-years). Of the 17 patients, death was due to fatal arrhythmia in 9 (12.9%, SCD in 4, ventricular tachycardia (VT)/ventricular fivrillation (VF) post cardio pulmonary arrest in 5 patients), heart failure in 7 (10.0%), including two with CRT-D, and myocardial infarction in 1 (1.4%). In contrast, appropriate therapy for VT/VF was delivered in 2 of 16 patients with CRT-D implantation, in whom a sudden cardiac death was prevented owing to appropriate therapy with implanted devices.
Table 2 shows the incidence of cardiac death in the total population and the three groups stratified according to cTnT levels. The high cTnT group exhibited the highest incidence of cardiac death events (p<0.001). In this group, 13 of the 17 cardiac deaths were observed. The remaining 4 events were observed in the intermediate cTnT group, and all were caused by fatal arrhythmia. In contrast, cardiac death was not observed in the low cTnT group.
| Overall (n=70) | Low (n=16) | cTnT | High (n=18) | p Value | |
|---|---|---|---|---|---|
| Intermediate (n=36) | |||||
| Cardiac death –n (%) | 17 (24.9) | 0 (0.0) | 4 (11.1) | 13 (72.2) | <0.001⁎ |
| Fatal arrhythmic event | 9 (12.9) | 0 (0.0) | 4 (11.1) | 5 (27.8) | 0.0489⁎ |
| Heart failure | 7 (10.0) | 0 (0.0) | 0 (0.0) | 7 (38.9) | <0.001⁎ |
| Myocardial infarction | 1 (1.4) | 0 (0.0) | 0 (0.0) | 1 (5.6) | 0.231 |
- Data given as n (%). p values represent the comparison across the 3 groups of low cTnT, intermediate cTnT, and high cTnT. cTnT = cardiac troponin T, FAE= fatal arrhythmic event
- ⁎ Indicates statistical significance.
Fig. 1 shows Kaplan–Meier estimates in the three groups. Panel A exhibits the results of all patients. The event-free rate was lower in the high cTnT group than in the other two groups (p<0.001). Panels B and C show similar data for the IHD and non-IHD subgroups, respectively. Interestingly, in the IHD subgroup, cardiac death was observed only in the high cTnT group and not in the other two groups (p<0.05; Fig. 1B). In contrast, in the non-IHD subgroup, cardiac death was observed in the high and intermediate cTnT groups; however, the tendency was similar and the event-free rate was lower in the high cTnT group than in the low cTnT group (p=0.0068; Fig. 1C).
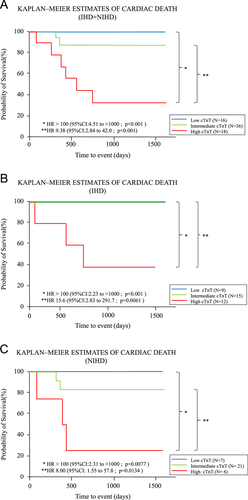
Kaplan–Meier estimates of prognoses in the three patient groups with different cTnT levels. This figure shows Kaplan–Meier estimates of prognoses in patient groups with low, intermediate, and high cTnT levels. Panel A presents the results for all patients with cardiac death. The event rate was higher in the high cTnT group than in the other groups. Panel B presents the sub-analysis data for IHD patients. The event rate was higher in the high cTnT group than in the other groups, and no event was observed in the low and intermediate cTnT groups. Panel C presents the sub-analysis data for non-IHD patients. The event rate was higher in the high cTnT group than in the other groups. IHD=ischemic heart disease, cTnT=cardiac troponin T, HR=hazard ratio, 95% CI=95% confidential interval.
Table 3 shows the results of Cox proportional hazards model adjusted for serum creatinine. In this analysis, high cTnT was associated with cardiac death even after consideration of renal function.
| Cardiac death | |||
|---|---|---|---|
| High vs. Low | HR | 95%CI | p Value |
| Unadjusted | >100 | 4.51 to >1000 | <0.001⁎ |
| Adjusted for Cr | >100 | 4.92 to >1000 | <0.001⁎ |
| High vs. intermediate | HR | 95%CI | p value |
| Unadjusted | 9.38 | 2.85 to 42.1 | <0.001⁎ |
| Adjusted for Cr | 10.5 | 2.97 to 48.7 | <0.001⁎ |
- Cr=serum creatinine, HR=hazard ratio, CI=confidence interval, IHD=ischemic heart disease.*Indicates statiscal significance.
4 Discussion
The present study had several important findings. First, of the 70 patients with LV dysfunction (LVEF,<35%) and NYHA class II/III heart failure, 17 patients (24.9%) experienced cardiac death during the observation period of 38.2±20.5 months. Second, the incidence of cardiac death was different among the subgroups stratified by serum cTnT levels evaluated in a stable state, and the incidence was highest in the high cTnT group among all the groups, while no cardiac death was observed in the low cTnT group. Finally, these results were obtained even after adjusting for serum creatinine levels. To the best of our knowledge, this is the first systematic demonstration of the correlation between elevated cTnT in a stable state and cardiac death among patients with LV dysfunction and heart failure in a Japanese population that included non-IHD patients.
4.1 Indication for prophylactic implantation of defibrillation devices
In patients with IHD and LV dysfunction, the MADIT-I and MADIT-II trials have shown that prophylactic use of ICD therapy reduced mortality when compared to that with conventional therapies [3], [4]. Even in non-IHD patients, the SCD-HeFT trial indicated that ICD therapy would reduce cardiac mortality in patients with NYHA class II/III and LVD (LVEF ≤ 35%) regardless of underlying diseases [5]. Based on these results, the European and American guidelines suggest prophylactic ICD implantation for prevention of sudden cardiac death in patients with LV dysfunction regardless of underlying heart diseases [1], [2]. However, the use of prophylactic ICD implantation was reportedly limited in clinical practice. Prophylactic ICD use has been reported to be only 16% and 38% in the US and Canada, respectively, even among patients who are eligible for ICD use for the primary prevention of sudden cardiac death [11], [12]. In the Japanese population, a similar or more emphasized tendency has been reported. Satake et al. reported that the prophylactic use of ICD/CRT-D was limited to 10.8% of patients with LVEF of ≤ 35% and symptomatic heart failure who were in the category of patients receiving prophylactic ICD for the primary prevention of sudden cardiac death, even with consideration of the Japanese guidelines [13]. Several reports have shown better outcomes in the Japanese population than in the European or American population [14], [15]. However, the recent CHART study documented a considerably high incidence of cardiac death in patients with LV dysfunction, even in the Japanese population, which is almost comparable to that in reports from Western countries [16]. In the present study, we observed cardiac death in 17 of 70 patients (24.9%) with LV dysfunction and heart failure, including non-ischemic heart disease, which was also considerably high. The precise reason for discrepancy in Japanese reports evaluating a similar Japanese population is unclear, but it may partly depend on the underlying disease and the difference in occurrence of cardiac events. In an American report, prophylactic ICD use did not demonstrate a significant improvement in the prognosis of a patient population with non-IHD [9]. Therefore, further accumulation of clinical data is necessary to clarify the patient population that is appropriate for prophylactic ICD use, especially in the Japanese population.
4.2 cTnT as an independent predictor of cardiac death
It is important to identify patients at a high risk of a sudden cardiac death in order to determine the strict indication of prophylactic ICD use in clinical practice. In several previous reports, the importance of cTnT evaluation as a marker for worse prognosis has been assessed in various types of patients [17]-[22]. Sato et al. demonstrated that elevation of serum cTnT levels was associated with higher mortality and myocyte degeneration in patients with idiopathic dilated cardiomyopathy [17]. cTnT is a highly specific material that originates only from the myocardium; therefore, acute myocardial injury, such as acute coronary ischemia, should be ruled out to interpret the clinical meaning of elevated cTnT levels. In previous studies, the investigators obtained samples in a stable state, which was at least 1 month apart from the acute phase of underlying heart diseases [10], [17]. The mechanism of cTnT elevation in such a stable state is controversial; however, it might indicate a small amount of myocardial injury and/or damage to myocytes in the presence of underlying heart diseases, i.e., apoptosis and/or necrosis, interstitial degeneration, overloaded calcium handling, stimulation of angiotensin, endothelin, inflammatory cytokines, oxidative stress, etc. [23]-[28]. In the present study, we evaluated cTnT levels in the stable state among patients with LV dysfunction and heart failure, and found that high cTnT levels were strongly associated with cardiac death, regardless of underlying heart diseases. This indicates that cTnT might be a predictor of cardiac events in patients with LV dysfunction and heart failure.
It is well known that cTnT or brain natriuretic peptide elevation might be exaggerated by chronic kidney disease (CKD) and that CKD sometimes shows false elevations in these values. Additionally, CKD itself can be associated with LV dysfunction in the mechanism of cardiac-renal interaction [29]. In our study, higher serum creatinine levels and higher incidence of NYHA class III heart failure were noted in the high cTnT group and not in the other groups. Although several reports have demonstrated a worse prognosis for patients with elevated cTnT in the mechanism of cardiac-renal interaction [30]-[32], we found that elevation of serum cTnT levels in a stable state was associated with a worse prognosis even after population adjustment for renal function.
4.3 Who benefits from prophylactic use of defibrillation devices?
Because patients of the present study were potential candidates for the prophylactic use of defibrillation devices, they might have been saved from a sudden cardiac death due to fatal arrhythmia, if such episodes had occurred [3]-[5]. On the other hand, inappropriate shock therapy would increase the chance of mortality through myocardial injury especially in patients with LV dysfunction [33]. Therefore, the actual indication of a defibrillation device should be discussed more precisely beyond simply blind adherence. In the present study, the prophylactic use of a defibrillation device was indicated in only 16 of 70 patients and only two patients were saved by appropriate therapy with CRT-D. If a defibrillation device would have been implanted in all 70 patients, nine patients with fatal arrhythmic events might have been saved, which is a considerable number, while the six patients with cardiac death, i.e., heart failure and myocardial infarction, might not have been saved. Although cTnT is a useful marker to predict cardiac death, its usefulness for prediction of fatal arrhythmia could not be evaluated because the number of patients was limited. In the PROSE-ICD study, elevation of cTnT levels was well correlated with an increase in the risk of death, but it poorly predicted the incidence of ICD shock in patients with LV dysfunction [21]. In addition, the impact of shock therapies on the prognoses of patients for all-cause death was more prominent in patient population with higher cTnT [34]. Therefore, it appears difficult to identify patients who will highly benefit from prophylactic defibrillation therapy even by using cTnT as the predictor [35]. However, interestingly, no cardiac death event, including a fatal arrhythmic event, was observed in the patient group with low cTnT levels. This suggests the possibility that a low cTnT level is a negative predictor of cardiac death, and this may be helpful for risk stratification to consider the accurate indication of prophylactic use of defibrillation devices.
This study has several limitations. First, this was a retrospective, single-center study with a small number of patients; therefore, our results might not be accurate in a larger population. Second, because the number of patients with cardiac death was small, statistical analysis was limited and the event cases might have involved some selection bias. Finally, because cTnT levels were assessed at limited time points, there may have been information bias in our results.
5 Conclusions
The cardiac death rate was considerably high in patients with LV dysfunction and symptomatic heart failure who were eligible for prophylactic use of defibrillation devices in our study population. The use of defibrillation devices was limited owing to various reasons. cTnT levels evaluated in a stable state were highly associated with prognoses even in IHD and non-IHD patients, and it appears to be useful as a predictor for future events in patients with LV dysfunction.
Disclosures
This study was partly supported by a grant for scientific research from the Ministry of Education Science and Culture of Japan (No. 26461085).
Conflict of interest
All authors declare no conflict of interest related to this study.
Acknowledgments
None.




