Minimally invasive, pericardial implantable cardioverter-defibrillator placement in a young child
Abstract
We report the successful minimally invasive placement of a pericardial implantable cardioverter-defibrillator (ICD) in a 16-kg child. A transvenous ICD dual coil was advanced through a small subxiphoid incision and screwed into the oblique sinus pericardium under fluoroscopic guidance. An additional sense-pace lead was sutured onto the right ventricular apex, and the generator was placed in the upper abdominal wall through the same incision. Threshold testing demonstrated successful defibrillation at 15 J. After implantation, the patient had two episodes of appropriate shock for ventricular fibrillation. The ICD system continues to show stable impedance at 6 months of follow-up.
1 Case report
The use of implantable cardioverter-defibrillator (ICD) therapy for prevention of sudden cardiac death in the pediatric population has been increasing. However, the use of transvenous ICD lead systems is limited in younger children and patients with congenital heart disease. Alternative techniques such as epicardial patch placement and subcutaneous systems require extensive surgery, often with a full sternotomy or thoracotomy [1], [2]. We report a case of pericardial ICD placement using a minimally invasive subxiphoid approach.
A 6-year-old girl with left ventricular non-compaction had ventricular fibrillation (VF) arrest from which she was successfully resuscitated with an automated external defibrillator (AED). She recovered without any neurological consequences and ICD implantation was indicated for secondary prevention. However, her body weight was only 16 kg and was thought to be too small for a transvenous ICD implantation; hence, the following surgical technique was chosen.
A pericardial window was created through an approximately 5-cm subxiphoid incision. Under fluoroscopic guidance to avoid injury to surrounding structures, a transvenous ICD dual-coil lead (model 6938, Sprint Quattro; Medtronic Inc., Minneapolis, MN, USA) was directed posteriorly and superiorly towards the oblique sinus. Once further advancement was not possible, the active fixation helix was screwed into the pericardium. Fixation was confirmed by a gentle tug on the coil. The proximal coil was shaped into a loop and sutured onto the inferior right ventricular (RV) wall with adequate slack to allow growth. Pericardial steroid-eluting bipolar electrodes (model 4968, Cap Sure, Medtronic Inc.) were sutured to the RV apex for sensing-pacing. Through the same incision, a subrectus pocket was created in the upper abdominal wall to place the ICD generator (Evera XT VR, Medtronic Inc.). The posteriorly positioned high-voltage lead and upper abdominal generator allows a good vector between coil and can. Defibrillation threshold testing (DFT) demonstrated two successful conversions from VF to sinus rhythm at 15 J. A postoperative chest X-ray confirmed adequate shock lead and generator location (Fig. 1).
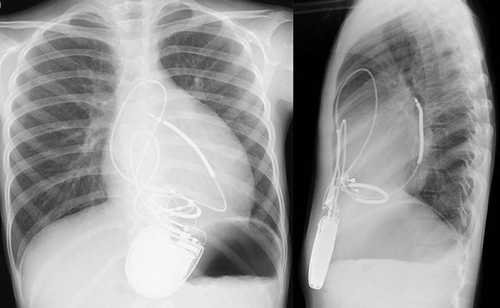
Configuration of the shock lead and generator on X-ray.
The procedure was complicated by postoperative pericardial effusion, which was likely due to postpericardiotomy syndrome. This was treated with oral nonsteroidal anti-inflammatory drugs and steroids and did not require any additional pericardial drainage.
Since implantation, the patient has experienced two episodes of appropriate ICD therapy for VF. In both episodes, ectopic atrial tachycardia degenerated into VF (Fig. 2). There was adequate VF detection, which led to successful defibrillation at 35 J, subsequent to failed antitachycardia pacing during charging.
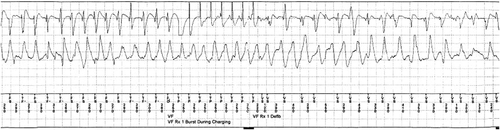
Electrogram of episode of VF.
The ICD system continues to show stable lead impedance at 6 months of follow-up. Configuration change due to growth may lead to change in the DFT, and follow-up testing to ensure adequate DFT might be necessary.
As previously described, pericardial placement of a defibrillation coil provides a safe and efficacious approach to ICD therapy in young children when a transvenous system is not feasible [3], [4]. The configuration of a posteriorly and superiorly placed coil in the oblique sinus and abdominal generator demonstrates low and stable defibrillator energy and stable impedance. To the best of our knowledge, this is the first case report in Asia of pericardial ICD placement using a minimally invasive subxiphoid approach.
Conflicts of interest
All authors declare no conflict of interest related to this study.




