Retracted: Effects of cardiac resynchronization therapy in patients with inotrope-dependent class IV end-stage heart failure
Abstract
Background
Cardiac resynchronization therapy (CRT) has been widely used for the treatment of refractory heart failure (HF). However, the efficacy of CRT is not well established in class IV HF patients on inotropic support.
Methods
Twenty-six patients (age 55±18 years, 73% men) with inotrope-dependent HF were reviewed to evaluate the effectiveness of CRT in class IV HF patients on inotropic support.
Results
Intravenous inotropic therapy was administered for 72±56 days before CRT and consisted of dobutamine (n=24; 3.0±1.2 μg kg−1 min−1), dopamine (n=2; 4.5±2.1 μg kg−1 min−1), and/or milrinone (n=16; 0.12±0.09 μg kg−1 min−1). CRT did not produce significant reverse remodeling in eligible patients (left ventricular ejection fraction 23±7% to 25±9%; p=0.23, left ventricular end-diastolic diameter 70±9 mm to 68±9 mm; p=0.14). After CRT device implantation, 13 (50%) patients experienced 1 or more episodes of ventricular tachyarrhythmia or sudden cardiac death. Twenty (77%) patients survived to hospital discharge with weaning from inotropic support (70±70 days after CRT implantation). The 1-year survival rate was 81%. However, data from long-term follow-up showed that 68% of the study patients who attained survival discharge had an HF hospitalization event within the follow-up period.
Conclusion
CRT did not result in significant reverse remodeling in patients with inotrope-dependent class IV end-stage HF. However, it contributed to dramatically improve the cardiovascular outcomes at least in the short-term period in some patients.
1 Introduction
Patients with inotrope-dependent class IV end-stage heart failure (HF) have an extremely poor prognosis with medical therapy alone [1]. For these patients, cardiac transplantation or left ventricular assist device (LVAD) implantation is a suitable option to improve the morbidity and mortality rates. However, because of poor number of donors, legal issues, or financial cost, these therapies could not be used widely especially in non-Western countries.
A significant proportion of HF patients with depressed left ventricular ejection fraction (LVEF) has abnormal electrical activation that is associated with cardiac dyssynchrony. Biventricular pacing has been shown to improve the prognosis of these patients [2]. Recent clinical evidences have shown that cardiac resynchronization therapy (CRT) has made remarkable progress for patients with HF [3]-[5].
According to a previous report [6], even in patients with New York Heart Association (NYHA) class IV HF, CRT significantly improves mortality and hospitalization rates. However, hemodynamically unstable severe HF patients who require inotropes are usually excluded from major CRT trials, and the current guidelines do not recommend CRT as a therapeutic option for such patients [7], [8]. Accordingly, there are limited data about CRT implantation in class IV HF patients on continuous inotropic support, and the efficacy of CRT for such patients is not well established.
2 Methods
2.1 Study population
The population of this retrospective review study comprised consecutive patients implanted with a CRT device between April 2004 and April 2011 in the National Cerebral and Cardiovascular Center in Japan. We excluded patients who could not be followed-up for at least 2 years for reasons besides death or LVAD implantation, in order to evaluate the long-term prognosis. The indications for CRT implantation in this population were based on the international standard guidelines [7], [8], which include LV systolic dysfunction (LVEF <35%), advanced HF (NYHA class >2), and wide QRS complex (>120 ms) after optimal medical therapy. Among our cohort, we identified 26 consecutive patients with NYHA class IV HF on inotropic support (age 55±18 years, 73% men) who underwent CRT implantation. Clinical characteristics and evaluation variables, including blood tests, 12-lead electrocardiogram, and echocardiography, were recorded at baseline and at all follow-up visits after CRT implantation. This study complies with the Declaration of Helsinki and was approved by the local ethics committee.
2.2 Definition of inotrope dependence
We defined inotrope dependence as the inability to stop or decrease the dose of the inotropes without hypotension, oliguria (<400 mL/day), and/or hypoxia [9]. We excluded patients who required perioperative inotropes within 4 weeks owing to inotrope dependence and a decompensated state of HF. The inotropes used included dobutamine, dopamine, and milrinone. All eligible patients were admitted non-electively, required intravenous inotropic therapy for hemodynamic maintenance, and underwent CRT implantation while on inotropic support.
2.3 Echocardiographic evaluation
All patients underwent routine echocardiography before and after CRT device implantation. Standard 2-dimensional echocardiography and Doppler imaging were performed by well-trained echocardiographists and reviewed by cardiologists. LV end-diastolic diameter (LVDD), LV end-systolic diameter (LVDS), and LVEF were measured using the modified biplane Simpson rule [10]. For quantification of mitral regurgitation (MR), apical 4-chamber images were used. MR was characterized as none=0, mild=1 (jet area/left atrium [LA] area <10%), moderate=2 (jet area/LA area 10–20%), moderate-severe=3 (jet area/LA area 20–45%), and severe=4 (jet area/LA area >45%).
2.4 Device implantation and management
All patients underwent CRT implantation under general anesthesia and mechanical ventilation. All pacing and defibrillator systems were implanted transvenously. During the procedure, the sensing and pacing thresholds were measured.
During follow-up, device interrogation was scheduled, and the pacing/sensing thresholds and arrhythmic events were checked. CRT optimization, including adjustment for atrioventricular and interventricular timing, was performed using echocardiography at 1 month and when necessary after device implantation.
2.5 Clinical response and endpoints
The clinical response to CRT was evaluated at 3 months follow-up. All adverse cardiac events, including all hospitalizations due to a cardiac cause, all deaths, and all lethal arrhythmic events were followed. In addition, the number of survival discharge or in-hospital deaths after CRT was also identified. LVAD implantation was considered as the endpoint in this study.
2.6 Statistical analysis
A p-value of <0.05 was considered statistically significant. Continuous variables are expressed as mean±SD. For pairwise comparisons, a paired t test was used for normally distributed data. Non-normally distributed data were compared using the Wilcoxon signed rank test. All tests were 2-sided. The survival function was computed as the time of implantation to the event. The observation was censored at the time of the last known follow-up or at the time of the events. Event-free survival curves were calculated according to the Kaplan–Meier method. Statistical analysis was performed using the JMP 10 software.
3 Results
3.1 Baseline characteristics
We retrospectively reviewed 26 consecutive inotrope-dependent class IV patients who underwent CRT at our institution. The baseline characteristics of the eligible patients are shown in Table 1. All patients had a depressed LVEF (23±7%), wide QRS complex (159±38 ms), and high brain natriuretic peptide (BNP) level (608±481 pg/mL). Concerning the etiology of the underlying heart disease, ischemic heart disease occurred in 15% and non-ischemic heart disease occurred in 85%.
| Clinical parameters | Inotrope-dependent class IV patients (n=26) |
|---|---|
| Age (years) | |
| Male (%) | 55±18 |
| Ischemic etiology (%) | 19 (73%) |
| Diabetes (%) | 4 (15%) |
| Chronic kidney disease (%) | 6 (23%) |
| CRT-D/CRT-P (%) | 12 (48%) |
| SR (%) | 20 (77%)/6 (23%) |
| Permanent AF (%) | 16 (62%) |
| QRS duration (ms) | 10 (38%) |
| History of sustained VT (%) | 159±38 |
| History of VF (%) | 8 (31%) |
| Echocardiographic parameters | 2 (8%) |
| LVEF (%) | |
| LVDD (mm) | 24±7 |
| LVDS (mm) | 71±9 |
| Mitral regurgitation (grade) | 62±10 |
| Conduction disorders (%) | 2.3±0.9 |
| Left bundle-branch block | |
| Intraventricular conduction delay | 11 (42%) |
| Right bundle-branch block | 10 (38%) |
| Medications (%) | 5 (19%) |
| ACE inhibitor or ARB | 19 (73%) |
| β-Blocker | 23 (88%) |
| Amiodarone | 17 (65%) |
| Diuretics | 26 (100%) |
| Digoxin | 11 (43%) |
- CRT-D: cardiac resynchronization therapy with defibrillator; CRT-P: cardiac resynchronization therapy pacemaker; SR: sinus rhythm; AF: atrial fibrillation; VT: ventricular tachycardia; VF: ventricular fibrillation; LVEF: left ventricular ejection fraction; LVDD: left ventricular end-diastolic diameter; LVDS: left ventricular end-systolic diameter; ACE: angiotensin-converting enzyme; ARB: angiotensin II receptor blockers.
3.2 Inotropic support and mechanical support
Intravenous inotropic therapy was administered for 72±56 days before CRT implantation and consisted of dobutamine (n=24; 3.0±1.2 μg kg−1 min−1), dopamine (n=2; 4.5±2.1 μg kg−1 min1), and/or milrinone (n=13; 0.12±0.09 μg kg−1 min−1). Three patients required mechanical ventilatory support. After CRT implantation, the intravenous inotropic agents were gradually decreased, and 20 of 26 patients (77%) were able to withdraw from inotropic support. The average time to weaning from inotropic therapy was 70±70 days.
3.3 Follow-up clinical evaluation
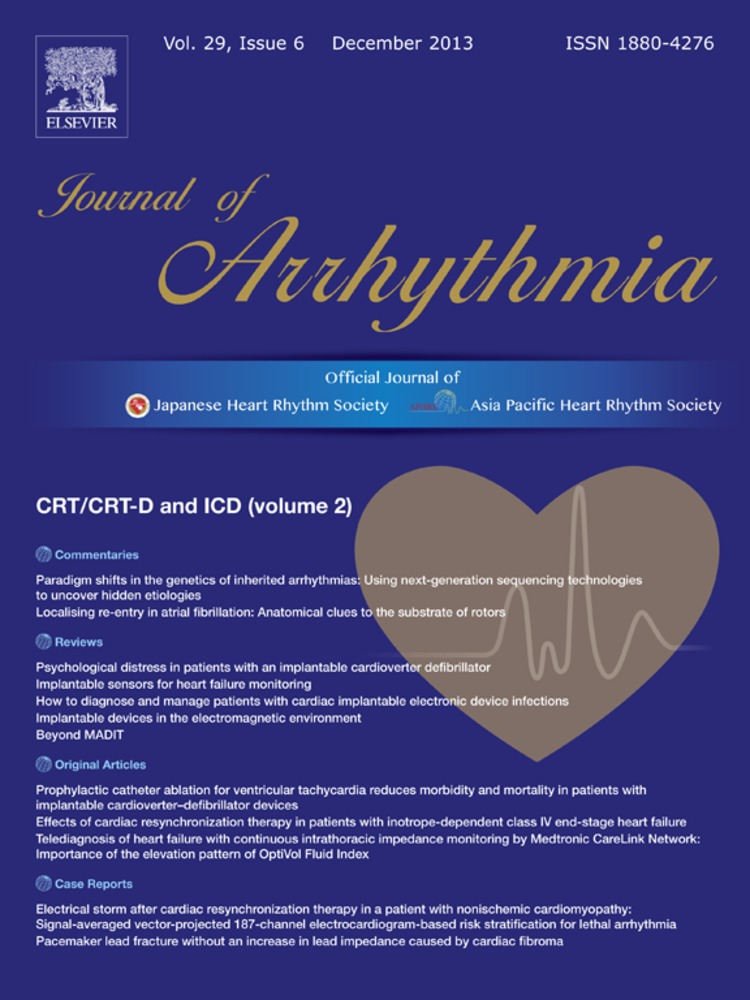
At 3 months follow-up, the symptoms of HF improved in 20 (77%) patients to NYHA class I (n=1), class II (n=10), class III (n=4), and class IV without inotropic support (n=5). However, after CRT implantation, 3 (12%) patients died within 3 months and 3 (12%) patients could not withdraw from inotropic support (Fig. 1). Concerning echocardiographic changes after 3 months follow-up, the LV systolic function and LV volumes showed no significant changes after CRT implantation (LVEF at baseline: 23±7% vs. at 3 months follow-up: 25±9%; p=0.23, LVDD at baseline: 70±9 mm vs. at 3 months follow-up: 68±9 mm; p=0.14, LVDS at baseline: 61 ±10 mm vs. at 3 months follow-up: 60±9 mm; p=0.18); however, the MR significantly decreased (mean grade at baseline: 2.2±1.0 vs. at 3 months follow-up: 1.7±1.0, p<0.005). Other changes in clinical parameters from pre-CRT to post-CRT are listed in Table 2. The BNP levels decreased significantly after CRT implantation compared with those before CRT implantation (pre-CRT: 608±481 pg/mL vs. post-CRT: 452±391 pg/mL, p=0.021).
Changes of New York Heart Association (NYHA) functional class at 3 months follow-up. The symptom of heart failure improved in 20 (77%) patients to NYHA class I (n=1), class II (n=10), class III (n=4), and class IV without inotropic support (n=5). However, 3 (12%) patients died within 3 months and 3 (12%) patients could not withdraw from inotropic support.
| Variables | Pre-CRT | Post-CRT | p Value |
|---|---|---|---|
| LVEF (%) | 23±7 | 25±9 | 0.23 |
| LVDD (mm) | 70±9 | 68±9 | 0.14 |
| LVDS (mm) | 61±10 | 60±9 | 0.18 |
| Mitral regurgitation | 2.2±1.0 | 1.7±1.0 | 0.008 |
| BNP (pg/mL) | 608±481 | 452±391 | 0.021 |
| Hemoglobin (g/dL) | 11.4±1.8 | 11.6±1.8 | 0.92 |
| Sodium (mEq/L) | 134.3±4.1 | 135.8±4.7 | 0.043 |
| Creatinine (mg/dL) | 1.25±0.58 | 1.16±0.44 | 0.84 |
| Total bilirubin (mg/dL) | 1.02±0.67 | 0.68±0.47 | <0.001 |
- CRT: cardiac resynchronization therapy; LVEF: left ventricular ejection fraction; LVDD: left ventricular end-diastolic diameter; LVDS: left ventricular end-systolic diameter; BNP: brain natriuretic peptide.
3.4 Clinical outcomes
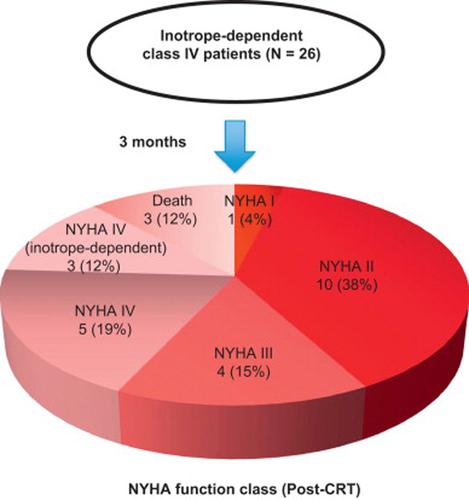
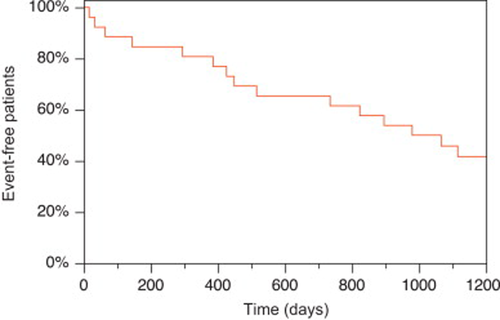
During a mean follow-up of 1033±742 days, 9 (35%) patients died within 2 years and 13 (50%) patients experienced 1 or more episodes of ventricular tachyarrhythmia or sudden cardiac death after CRT. Among those patients, 20 (77%) survived to hospital discharge, and the 1-year survival rate was 81%. However, 68% of the study patients had an episode of HF rehospitalization during the follow-up period. Only 1 patient had successful cardiac transplantation, and 6 patients required LVAD implantation. Fig. 2 shows the event-free survival curve for all-cause death or LVAD implantation. The 1-year and 2-year survival rates were 81% and 65%, respectively. Fig. 3 shows the event-free survival curve for HF rehospitalization among the patients who survived to hospital discharge after the successful withdrawal of inotropic support. The 1-year and 2-year event-free survival rates were 65% and 44%, respectively. Fig. 4 shows the event-free survival curve for ventricular tachyarrhythmias or sudden cardiac death after CRT. On the basis of the analysis, lethal ventricular arrhythmias occurred frequently within 100 days. The event-free rate at 1-year was 65%.
Cumulative probability of survival for patients with inotrope-dependent class IV heart failure after cardiac resynchronization therapy (CRT) implantation. The Kaplan–Meier curve for all-cause mortality in patients with inotrope-dependent class IV heart failure after device implantation indicates that the 1-year and 2-year survival rates were 81% and 65%, respectively.
Cumulative free probability of heart failure (HF) hospitalization in patients with inotrope-dependent class IV HF after cardiac resynchronization therapy (CRT) implantation. The Kaplan–Meier curve for HF hospitalization in patients with inotrope-dependent class IV HF who were discharged after device implantation shows that the 1-year and 2-year event-free survival rates were 65% and 44%, respectively.
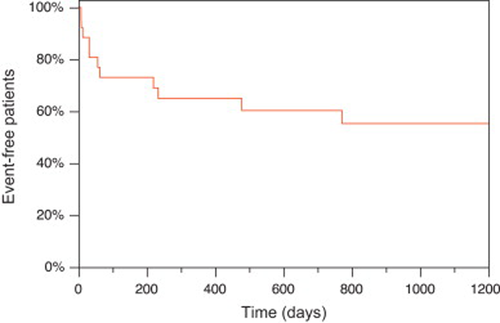
Cumulative free probability of ventricular tachyarrhythmias or sudden cardiac death in patients with inotrope-dependent class IV heart failure (HF) after cardiac resynchronization therapy (CRT) implantation. The Kaplan–Meier curve for ventricular tachyarrhythmias or sudden cardiac death in patients with inotrope-dependent class IV HF after device implantation shows that lethal ventricular arrhythmia occurred frequently within 100 days, and the event-free rate at 1 year was 65%.
4 Discussion
Our study had 3 major findings. First, most of the inotrope-dependent patients can withdraw from inotrope therapy and be discharged from the hospital after CRT implantation. Second, concerning echocardiographic parameters, CRT did not result in significant LV reverse remodeling among our study patients at 3 months follow-up. Finally, CRT improved the symptoms and short-term outcome in patients with inotrope-dependent class IV end-stage HF.
There are several reports about the clinical outcomes of patients with end-stage HF. The REMATCH trial reported extremely poor outcomes in the medical therapy—only group in patients with end-stage HF [1]. In that study, the optimal medical therapy group included 75% inotrope-dependent HF patients and the 1-year survival rate was only 25%. In relation to the comparison with LVAD patients, the HeartMate II trial studied the outcomes in continuous-flow LVAD patients [11]. Even in those patients, the 1- and 2-year survival rates were 68% and 58%, respectively. Our patients had similar baseline characteristics except that most had non-ischemic HF. However, the 1-year survival rate in our study population after CRT was 81%, which supports the favorable effects of CRT in patients with inotrope-dependent HF.
Herweg et al. [9] evaluated the benefit of CRT in 10 consecutive patients with NYHA class IV HF who were dependent on inotropic support. Their patients had received inotropic support for 146±258 days, and all patients were alive at the mean follow-up of 1088±284 days after CRT. They also reported an improvement in LVEF (23.5±4.3% to 32.0±9.1%; p<0.05). Cowburn et al. [12] identified 10 patients who required inotropic support and underwent CRT while being administered with inotropic agents. All patients were weaned from inotropic agents and survived to hospital discharge. These reports are congruent with our report and support the beneficial effects of CRT for patients with inotrope-dependent HF. However, Adelstein et al. [13] reported conflicting findings. They divided their cohort of CRT patients into 3 groups according to exposure to intravenous inotropes before CRT—(1) no inotropes, (2) previous inotrope administration, and (3) dependent on inotropes—and compared the clinical outcomes. In their study, 16 inotrope-dependent patients were identified and the 1-year survival rate was <20%. In addition, inotrope-dependent patients exhibited neither functional improvement nor reverse remodeling in their study. The discrepancy between our study and their report may be partly explained by the fact that many of their patients had LVAD implantation and cardiac transplantation. It may be easier to assess LVAD or cardiac transplantation owing to the differences in social background. Moreover, most of our patients had non-ischemic cardiomyopathy, and were generally thought to benefit more from CRT than ischemic cardiomyopathy patients.
Bhattacharya et al. [14] also reported negative effects of CRT for patients with HF on inotropes at implantation. They retrospectively analyzed >700 CRT-defibrillator recipients and categorized them as never on inotropes (NI group), weaned from inotropes before implantation, or on inotropes at implantation (II group). Their control group comprised patients with a standard defibrillator. They compared the overall survival and survival free from heart transplant or LVAD between those 4 groups. On the basis of their report, the II group patients demonstrated significantly shorter survival than the NI group patients at 12 months (hazard ratio, 2.95; 95% confidence interval, 1.05–8.35), and CRT may not have a survival advantage over a standard defibrillator for patients who had received inotropes before CRT. The propensity score-adjusted event-free survival rate in II group patients with regard to LVAD and heart transplantation at 12 months was around 60%, and the overall survival at 12 months was about 70%. Their survival rate was much better compared with that in the previously described reports; however, the authors reported no beneficial effects of CRT for inotrope-dependent HF patients. Their cohort was the largest study cohort of CRT patients on inotropic support; however, the II group was not exactly inotrope-dependent (i.e., they simply defined the II group as patients on inotropes at CRT implantation). Furthermore, the control group of patients with a standard defibrillator comprised only 3% of NYHA class IV patients, and these control group patients were thought to have milder HF than the II group patients. From this point of view, the effectiveness of CRT in inotrope-dependent HF patients could not be entirely denied.
4.1 Clinical implications
Previous large CRT trials excluded patients with NYHA class IV HF on inotropic support. Thus, the clinical evidence associated with the role of CRT in the management of those patients was unclear. On the basis of the results of our study, >75% of the studied patients showed improvement in HF symptoms, and the 1-year survival rate was >80%. The findings of this study strongly support the beneficial effects of CRT even in inotrope-dependent HF patients.
We have shown the event-free survival curve for ventricular tachyarrhythmias after CRT implantation in this study. The incidence of lethal ventricular arrhythmias was remarkably high especially within 100 days after CRT implantation. This finding may be related to the unstable hemodynamics owing to weaning from inotropes or the proarrhythmic effects of biventricular pacing [15]-[17]. These observations raise the concern that patients with inotrope-dependent HF would need to be managed carefully in the early phase after CRT to avoid arrhythmic events.
Concerning the mechanical changes after CRT, the eligible patients did not show significantly increasing LVEF and decreasing LV volume despite the improving MR at 3 months follow-up. The discrepancy between prognostic and mechanical improvement after CRT is probably attributable to the inotropic therapy itself. Inotropic agents usually emphasize systolic function and the pre-CRT LVEF could be overestimated. The changes in BNP level, serum sodium, and total bilirubin in patients after CRT implantation support the improvement in their hemodynamics. Even if significant reverse remodeling was not observed after CRT in this study, the benefit of CRT for functional improvement could not be denied. The prognosis of patients with inotrope-dependent class IV end-stage HF is still very poor; however, in the absence of an indication for heart transplantation or LVAD as a destination therapy, CRT is one of the most important therapeutic options for those patients.
4.2 Study limitations
This study was a single-group, non-randomized, retrospective review study. Although this study had the largest population among studies on the effects of CRT in patients with inotrope-dependent class IV end-stage HF, the number of patients was still small. Further study with a large sample is needed to confirm the efficacy of CRT for patients with inotrope-dependent class IV end-stage HF. In addition, the influence of underlying comorbidities could be an important factor for determining prognosis besides CRT effects alone.
5 Conclusions
CRT did not result in significant reverse remodeling in patients with inotrope-dependent class IV end-stage HF. However, it contributed to dramatically improve the symptoms, hemodynamics, and cardiovascular outcomes at least in a short-term period in some patients.
Conflict of interest
There was no financial support from any specific company for this study or any conflict of interest, and no specific unapproved use of any compound or product was made.
Acknowledgments
The encyclopedic cardiology knowledge of Fumihiko Miyake is gratefully appreciated.