Effect of atorvastatin on plasma levels of asymmetric dimethylarginine in patients with non-ischaemic heart failure
Abstract
Background:
Elevated plasma levels of asymmetric dimethylarginine (ADMA), an endothelial nitric oxide synthase (eNOS) inhibitor, may contribute to endothelial dysfunction in chronic heart failure (CHF). Since statins upregulate eNOS and ameliorate endothelial dysfunction in non-ischaemic CHF, we hypothesized that this may be in part through modification of ADMA.
Aim:
To evaluate the effect of atorvastatin on the relationship between ADMA and endothelial function in non-ischaemic CHF.
Methods:
Twenty-four patients with CHF (ejection fraction <40%, New York Heart Association Functional Classes II and III) were randomised to atorvastatin treatment (40 mg) or placebo once daily for 6 weeks in a double-blinded, placebo-controlled crossover study. Plasma ADMA and L-arginine levels were measured by HPLC. Endothelial function was assessed by flow-mediated dilatation and invasive forearm plethysmography.
Results:
Post-statin therapy, endothelial function was improved (p<0.05) independent of LDL-cholesterol reductions, but no changes were observed in ADMA levels or the L-arginine to ADMA ratio. There was a trend for ADMA to inversely correlate with endothelial function at baseline.
Conclusions:
Short-term atorvastatin treatment in non-ischaemic CHF improves endothelial function but has no effect on ADMA or the L-arginine to ADMA ratio. Our finding suggests that the observed statin-induced improvements in endothelial function are likely mediated via alternative pathways.
1. Background
Amongst the multiple factors implicated in chronic heart failure (CHF), endothelial dysfunction has emerged as an important feature, contributing to reduced cardiac output and increased peripheral vascular resistance [1]. Endothelial dysfunction is characterised by dysregulation of the L-arginine-nitric-oxide pathway [2]. Plasma levels of asymmetric dimethylarginine (ADMA), a potent endothelial nitric oxide synthase inhibitor (eNOS), are elevated in CHF, having been positively associated with disease severity [3] and increased cardiovascular risk [4]. ADMA may represent a novel marker of impaired endothelial function in CHF, thereby contributing to cardiovascular risk [5]. Furthermore, the L-arginine to ADMA ratio has also been proposed as a potential marker of endothelial function [6], with reductions seen in a number of cardiovascular disease states, including hypertrophic cardiomyopathy [7]. Statins have been reported to upregulate the expression and function of eNOS [8 9 10], and ameliorate endothelium-dependent function in non-ischaemic CHF, through lipid-independent pathways [11]. Whether statin-induced improvements in endothelial function are mediated through reductions in ADMA in patients with non-ischaemic CHF is unknown.
2. Aims
The present study was designed to investigate the effect of short-term atorvastatin treatment on plasma ADMA levels and endothelial dysfunction in patients with stable, non-ischaemic, left ventricular dysfunction. We hypothesised that statin therapy would lower ADMA concentrations, and facilitate restoration of endothelial function in CHF.
3. Methods
Twenty-four patients with symptomatic heart failure were randomised to receive atorvastatin (40 mg) or matching placebo once daily for 6 weeks in a balanced sequence double-blinded, placebo-controlled crossover study, with a 2-week washout period between treatments. A computer generated randomisation list was prepared in advance and made available to the study pharmacist. Patients were recruited from Cardiology Outpatient Clinics at the Christchurch Hospital. Twenty-three patients, aged 60.7±10.4 years, completed the study and one patient withdrew prior to the first treatment visit, due to worsening heart failure. Patients had a reduced left ventricular ejection fraction (30.1±7.7%) and New York Heart Association Functional Classes II (n=14) or III (n=9). No patient had atrial fibrillation, a prior acute coronary event or revascularisation, stenotic cardiac valve disease, impairment of liver, renal (glomerular filtration rate <100 mL/min) or pulmonary function or was on lipid-modifying medications. However, four patients had some features of atherosclerotic disease on angiogram, but with no symptoms of myocardial ischaemia. Patients were receiving furosemide (n=18), ACE inhibitor (n=18) or angiotensin II receptor antagonist (n=4) with or without digoxin (n=2), a beta-adrenergic blocker (n=13), spironolactone (n=4) and aspirin (n=14). Patients maintained their standard anti-failure therapies for the duration of the study period. Plasma ADMA and L-arginine were measured by HPLC with fluorescence detection [12]. Flow-mediated dilatation [FMD] and glyceryl trinitrate-induced, endothelium-independent dilatation of the brachial artery was measured using high-resolution ultrasound [13]. Endothelium-dependent and independent resistance vessel function was assessed by forearm venous occlusion plethysmography during sequential, intra-arterial infusion of acetylcholine, sodium nitroprusside and N-monomethyl-L-arginine (L-NMMA) alone or in combination [14]. Plasma total cholesterol, triglycerides, and HDL-cholesterol were determined using conventional enzymatic methods. LDL-cholesterol was calculated from the Friedewald equation. Measurements were performed at randomisation, and at the end of both treatment periods. Mean parameters were compared between placebo and statin therapy using paired-t-tests. Based on reported effects of statin treatment on ADMA concentrations [15], we calculated that 23 patients in a crossover design would provide sufficient power, at p<0.05, to detect a clinically significant effect of statin therapy on reductions in ADMA levels. Ethical approval was obtained from the Christchurch Ethics Committee.
4. Results
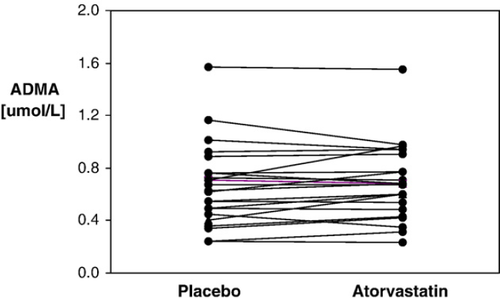
Baseline lipid profiles were total cholesterol 5.25±0.20 mmol/L (mean±SEM); LDL-cholesterol 3.32±0.16 mmol/L; triglycerides 1.60±0.13 mmol/L and HDL-cholesterol 1.22±0.08 mmol/L. Six weeks of atorvastatin therapy resulted in the expected reductions in total cholesterol (37%), LDL-cholesterol (50%), and triglycerides (26%) in comparison to placebo (p<0.001 for all). HDL-cholesterol levels remained unchanged. Statin treatment improved endothelium-dependent FMD compared to placebo (1.3% (SEM 0.6) p<0.05). Moreover, acetylcholine (ACh)-induced endothelium-dependent vasodilatation of the forearm resistance vessels (mean AUC±SEM) was greater following atorvastatin than after placebo (3.72±0.65 vs 2.67±0.48 for ACh at 15 μg/min (p=0.015) and 4.59±0.63 vs 3.68±0.53 for ACh at 30 μg/min; p=0.07). Improved resistance vessel function was eliminated during co-infusion with L-NMMA (p=0.78 for ACh at 15 μg/min and p=0.69 for ACh at 30 μg/min). Basal forearm blood flow and endothelial-independent vasodilatation of the conduit and resistance vessels did not differ between regimes. There was no change in concentrations of ADMA (Fig. 1), or the L-arginine to ADMA ratio with statin administration compared to placebo (p>0.24). However, at baseline there was a trend for ADMA to correlate with FMD and resistance vessel function at increasing ACh dosages (Table 1). Conversely, the L-arginine to ADMA ratio was not associated with endothelial-dependent function (Table 1) and neither ADMA nor the L-arginine/ADMA ratio were correlated with basal forearm blood flow (Table 1), LDL-cholesterol (for ADMA r=−0.14, p=0.52 and for L-arginine to ADMA ratio r=0.13, p=0.56) or endothelium-independent vasodilatation. Statin-induced LDL-cholesterol reductions were independent of improvements in FMD (r=−0.27, p=0.26) and resistance vessel function (r=−0.94 (p=0.71) for ACh at 15 μg/min and r=−0.42 (p=0.08) for ACh at 30 μg/min). Furthermore, endothelial-dependent vascular function was not associated with either ADMA or the L-arginine to ADMA ratio in response to 6 weeks of statin therapy.
| ADMA | l-arginine/ADMA ratio | |||
|---|---|---|---|---|
| r | p-value | r | p-value | |
| FBF basal | −0.05 | 0.86 | −0.23 | 0.42 |
| FBF ACh 7.5 | −0.17 | 0.49 | 0.19 | 0.46 |
| FBF ACh 15 | −0.41 | 0.12 | 0.27 | 0.32 |
| FBF ACh 30 | −0.42 | 0.09 | 0.27 | 0.29 |
| FMD | −0.31 | 0.18 | 0.20 | 0.41 |
- a FBF: forearm blood flow; ACh 7.5: acetylcholine at 7.5μg/min; ACh 15: acetylcholine at 15 μg/min; ACh 30: acetylcholine at 30 μg/min; FMD: flow-mediated dilatation.
5. Conclusions
We demonstrated that short-term treatment with atorvastatin has no influence on plasma ADMA levels or the L-arginine to ADMA ratio in patients with non-ischaemic left ventricular dysfunction, despite marked improvement in lipid profiles and endothelium-dependent vasodilatory responses of both the micro and macrovascular circulation. Statin-induced amelioration of endothelial dysfunction was mainly independent of LDL-cholesterol reductions, a finding consistent with comparable studies [11,16]. There is evidence that increased free radical generation, as observed in CHF [17], may impair dimethylarginine dimethylaminohydrolase activity and lead to subsequent ADMA accumulation [18]. Elevated ADMA levels have been associated with adverse cardiovascular outcomes in patients with CHF [4], but it is unclear whether ADMA may directly impair endothelial function and thus contribute to increased cardiovascular risk in CHF. Since the non-lipid mediated benefits of statins include upregulation of eNOS [8 9 10] and alleviation of oxidative stress [19], we speculated that atorvastatin would lower ADMA concentrations and may thereby facilitate restoration of endothelial function. However, no reductions in ADMA or improvements in the L-arginine to ADMA ratio were observed. In previous studies, statin therapy has been variably linked to modifications in ADMA levels in hypercholesterolaemic patients [20,21] with only one study demonstrating improved FMD in association with reduced ADMA levels [15]. Furthermore, supporting the notion that ADMA may represent a novel marker of endothelial dysfunction [4], we observed a trend for a negative association between ADMA levels and endothelium-dependent vasodilatation in patients with CHF. Conversely, there was no trend for a positive association between the L-arginine to ADMA ratio and endothelial vasodilator responses, suggesting the L-arginine to ADMA ratio may not represent a marker of endothelial function in non-ischaemic CHF. In conclusion, if elevated ADMA levels contribute to endothelial dysfunction in non-ischaemic CHF; our findings could indicate that statin-induced improvements in endothelium-dependent function are mediated via alternative pathways to ADMA in these patients.




